When you hear generic drugs, medications that contain the same active ingredients as brand-name drugs but are sold without a brand name. Also known as generic medications, they work the same way, cost far less, and are held to the same safety standards by the FDA. Most people assume generics are cheaper because they’re weaker—but that’s not true. The FDA requires them to deliver the same dose, work the same way, and produce the same results as the original. A generic version of metformin, for example, lowers blood sugar just like Glucophage. The only differences? The color, shape, or inactive fillers—and the price, which can be 80% lower.
What makes a drug go from brand-name to generic? It’s all about drug patents, legal protections that give the original manufacturer exclusive rights to sell a drug for a set time. In the U.S., that’s usually 20 years from the patent filing date, but with extensions, it can stretch longer. Once that clock runs out, other companies can apply to make the same drug. But they don’t just copy it—they have to prove it’s bioequivalent. That means your body absorbs it at the same rate and to the same extent. The FDA approval, the process the U.S. Food and Drug Administration uses to evaluate whether a drug is safe and effective for generics is strict. They check manufacturing sites, test batches, and review clinical data. And they don’t stop there—post-market monitoring catches any unexpected side effects.
Not all drugs have generics. Biologics—like insulin, rheumatoid arthritis treatments, or cancer drugs—are complex molecules made from living cells. You can’t just copy them like a pill. That’s where biosimilars, highly similar versions of biologic drugs that are not exact copies but are proven to work the same way come in. The FDA’s 2025 rules made it easier for these to reach the market, cutting approval time and lowering costs for patients with chronic conditions. Meanwhile, in countries like Canada and the UK, generic entry happens faster, which is why prices drop sooner there than in the U.S.
Why does this matter to you? Because if you’re taking levothyroxine, sildenafil, or escitalopram, there’s almost always a generic version that works just as well. Buying it can save you hundreds a year. But not all online pharmacies are safe. Some sell fake generics with no active ingredient at all. That’s why knowing how to spot a legitimate source matters just as much as knowing what generic means.
The posts below cover real-world situations where generics make a difference—from comparing Vigora and sildenafil to buying cheap generic Lexapro in the UK, to understanding how patent laws delay access in different countries. You’ll find guides on how to check if your prescription has a generic, how to talk to your pharmacist about switching, and what to watch for when your insurance changes your drug. No fluff. Just what you need to save money without risking your health.

Discover proven, evidence-backed ways to cut medication costs without risking patient safety. From pharmacist-led care to generic drugs and SBAR communication, learn how hospitals are saving millions while preventing errors.

The Hatch-Waxman Act created the modern system for generic drugs in the U.S., balancing innovation and affordability. It let generics enter faster while giving brand companies patent extensions-saving billions but also opening the door to abuse.
Generic drugs make up 90% of U.S. prescriptions and save billions yearly. Learn how they're made-from reverse engineering brand-name drugs to FDA-approved manufacturing and bioequivalence testing-without clinical trials.
Mail-order pharmacies dispense 90% generic drugs with strict quality controls. Learn how temperature tracking, batch testing, and double verification ensure your meds are safe-even when shipped across the country.

Different medication classes-prescription, OTC, and herbal-come with unique side effect risks. Learn how to spot dangerous interactions, why generic switches matter for some drugs, and how to stay safe with every pill you take.
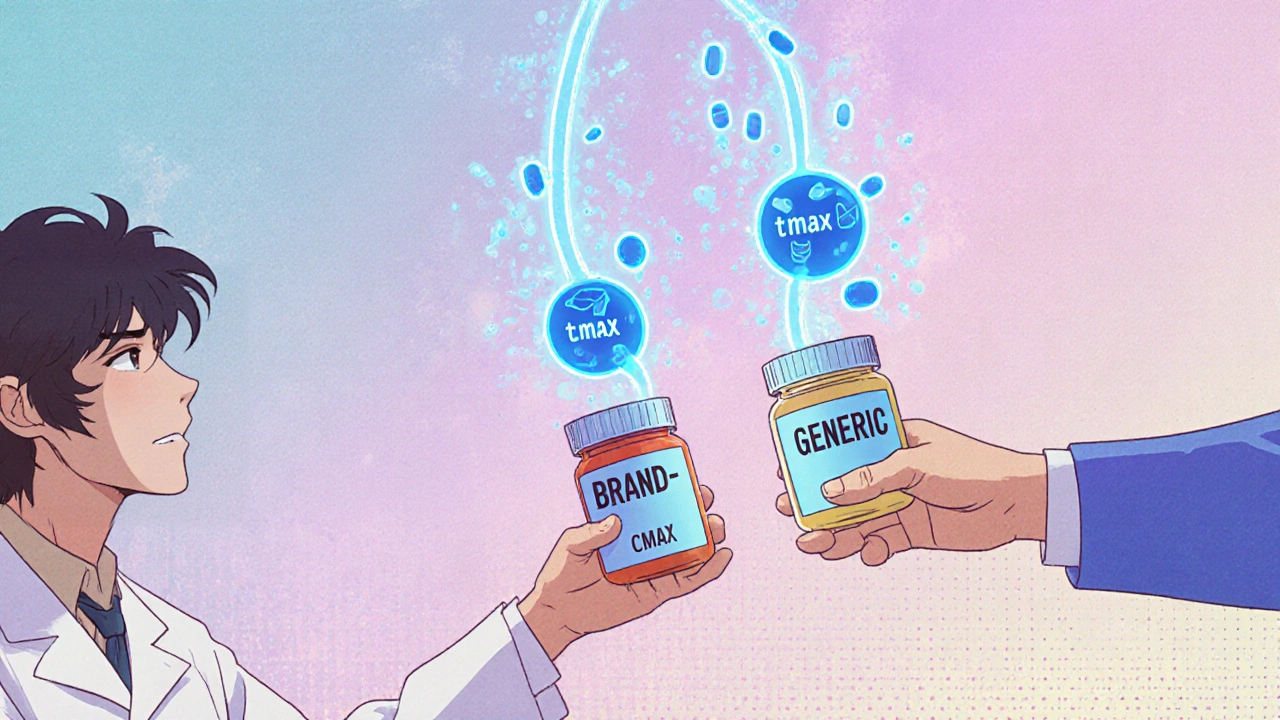
Bioequivalent medications are generic drugs proven to work the same as brand-name versions in your body. Learn how the FDA tests for equivalence, why it matters, and when to ask questions.
The FDA now enforces strict, unannounced inspections on foreign generic drug factories to ensure safety. Learn how CGMP standards, inspection gaps, and new policies are reshaping global drug manufacturing for American patients.
Stability testing ensures generic drugs remain safe and effective over time. The FDA requires rigorous testing of three batches under real and accelerated conditions to prove shelf life, potency, and purity match brand-name drugs.
