When you pick up a bottle of generic blood pressure medicine, antibiotics, or cholesterol pills, chances are it was made in a factory thousands of miles away-likely in India or China. About 80% of the active ingredients in U.S. medicines and 40% of finished generic drugs come from foreign factories. The FDA says these facilities must meet the same quality rules as U.S. plants. But for years, the reality looked very different.
Same Rules, Different Enforcement
The FDA requires every drugmaker-whether in Ohio or Odisha-to follow Current Good Manufacturing Practices (CGMP). These rules cover everything from how workers wash their hands to how test results are recorded. Every batch must be tested. Every machine must be cleaned and logged. Every error must be documented and fixed. But here’s the catch: while U.S. factories get surprise inspections with no warning, foreign plants often got 8 to 12 weeks’ notice. That’s enough time to clean up, fix records, or hide problems. In 2024, the FDA found violations in 45% of foreign inspections-more than twice the rate of domestic ones. Data integrity issues alone were 38.7% in foreign facilities versus 17.2% in the U.S. Contamination problems showed up in 22.4% of foreign inspections, compared to just 9.8% at home. This wasn’t a mistake. It was a system designed for convenience, not safety. Inspectors couldn’t travel as often. Budgets were tight. And there was a quiet assumption: if the company said it was compliant, maybe it was.The Turning Point: Unannounced Inspections Begin
On May 6, 2025, the FDA made a public shift. Commissioner Marty Makary announced that unannounced inspections of foreign facilities would jump from 15% to at least 50% of all overseas checks by mid-2026. This wasn’t just a policy tweak-it was a reset. No more advance notice. No more time to clean up. If you’re making drugs for Americans, you’re subject to the same sudden knock on the door as a plant in New Jersey. Why now? Pressure. A ProPublica investigation exposed how the FDA allowed drugs from a banned Indian facility to keep entering the U.S. market. Senators Kirsten Gillibrand and Tim Scott demanded answers after learning the FDA’s own inspectors had flagged safety issues-but those warnings were sometimes overruled. And then there was the executive order. President Trump’s EO 14135, signed May 5, 2025, forced the FDA to eliminate the inspection gap within 18 months. The message was clear: if you want to sell drugs in America, you play by American rules-no exceptions.What Happens During an FDA Inspection?
An FDA inspector doesn’t just walk in and ask for paperwork. They show up with a checklist that’s been hardened over decades.- They check training logs-did the technician who mixed the batch actually get certified?
- They pull raw data from lab equipment-was the chromatograph calibrated? Were results altered?
- They inspect storage areas-were raw materials kept dry? Were expired chemicals still in use?
- They review complaint files-how many customers reported pills that didn’t dissolve? Were those reports buried?

Why India and China Are the Center of This Storm
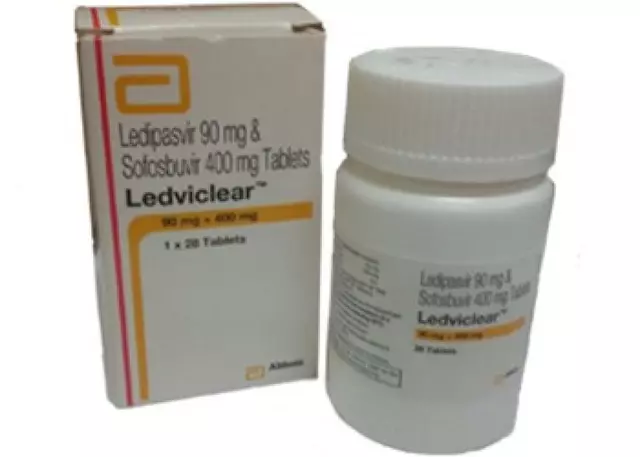
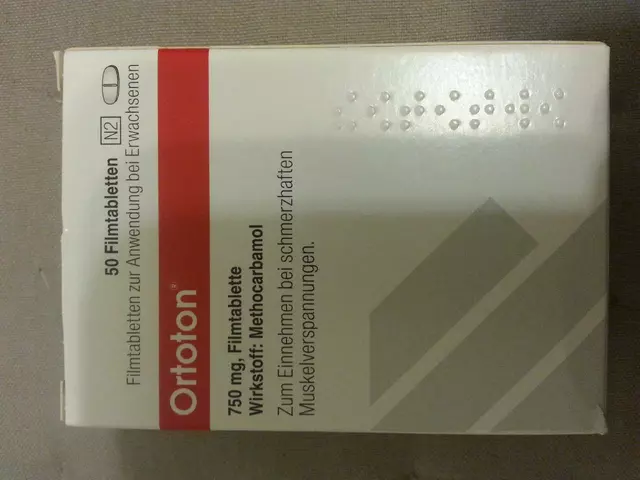
India makes 40% of the active pharmaceutical ingredients (APIs) for U.S. generics. China supplies another 13%. Together, they’re the backbone of affordable medicine in America. But scale creates risk. A single factory in Hyderabad might produce 200 million pills a month. One mistake-wrong temperature, contaminated water, falsified data-can affect millions of patients. The FDA’s 2024 report showed that 68% of foreign manufacturers believed the new unannounced inspection policy would raise their compliance costs by 15-25%. Smaller suppliers, especially, are struggling to afford the upgrades: new software for data logging, real-time environmental monitoring, full-time quality staff. Some are adapting. The Generic Pharmaceutical Association found that 42% of its members with overseas plants have already added extra audits, trained staff on documentation, and run mock inspections. Others are cutting corners-or leaving the market entirely.The EU Model: A Better Way?
Europe doesn’t rely on surprise visits alone. Every batch of medicine leaving a factory must be signed off by a Qualified Person-a trained professional who physically verifies that every step met standards before the product leaves the country. That person is legally responsible. If something goes wrong, they can be held accountable. It’s not a formality. It’s a legal duty. Brookings Institution researchers argue the U.S. should adopt a similar model. Instead of only inspecting factories, the U.S. could require U.S.-based importers to appoint their own Qualified Person. That person would review every batch before it crosses the border. No signature? No entry. It’s not a perfect fix. But it adds a second layer of control-something the current system lacks.
What This Means for Patients
You might wonder: is my medicine safe? The answer is: mostly. The FDA still approves over 90% of generic drugs. Most foreign manufacturers are honest, skilled, and compliant. The problem isn’t the workers-it’s the system that let some bad actors slip through. The new inspection rules are already making a difference. In the first quarter of 2025, the number of warning letters issued to foreign facilities jumped by 37% compared to the same period last year. Companies that ignored documentation rules are now being blocked at the border. But there’s a cost. Evaluate Pharma warns that in the short term, supply chains could tighten. Up to 15-20% of generic drug availability might dip as factories fix problems or shut down. That could mean temporary shortages of common drugs like metformin or lisinopril. The FDA is hiring 200 new inspectors for international work by 2026. They’re training them to spot falsified data, hidden records, and manipulated equipment logs. They’re working with agencies in the EU, Japan, and Australia to share inspection reports. The goal isn’t to punish foreign companies-it’s to make sure every pill you take works like it should.What Foreign Manufacturers Need to Do Now
If you’re a factory making generics for the U.S. market, here’s what you need to do:- Stop relying on advance notice. Assume an inspection could happen tomorrow.
- Review every document-paper or digital. Are records signed? Are timestamps accurate? Are deletions logged?
- Train every employee on data integrity. Falsifying a test result is a felony.
- Run weekly mock inspections. Bring in an outside auditor if you can.
- Prepare a response plan. Who answers the door? Who handles the inspector? Who logs the Form 483?
What Comes Next?
The FDA isn’t stopping here. By 2026, they plan to expand inspections to include supply chain transparency-tracing raw materials back to their source. They’re also looking at labor practices, responding to concerns about forced labor in some Chinese factories. The goal is simple: no more double standards. No more hidden problems. No more excuses. The system is changing. And for the first time in decades, the safety of your medicine isn’t left to chance-it’s being enforced.Are generic drugs made overseas safe?
Yes, most are. The FDA approves over 90% of generic drugs, even those made abroad. But safety depends on consistent compliance with U.S. manufacturing rules. The FDA’s new push for unannounced inspections is designed to catch facilities that cut corners, falsify records, or hide contamination. If a drug is approved, it meets the same standards as brand-name versions.
Why does the FDA inspect foreign factories less often than U.S. ones?
For years, the FDA lacked the budget and staff to conduct as many inspections overseas. Travel costs, visa delays, and political sensitivities made surprise visits harder. That changed in 2025, when the agency committed to increasing unannounced foreign inspections to at least 50% of all inspections by mid-2026, closing the gap with domestic oversight.
What happens if a foreign factory fails an FDA inspection?
The FDA issues a Form 483 listing violations. If the issues aren’t fixed, the agency sends a warning letter. Repeated or serious failures can lead to an import alert-blocking all shipments from that facility. The factory must prove corrections are made before any drugs can enter the U.S. again.
Can the FDA ban a drug from entering the U.S. even if it’s already been approved?
Yes. Approval is not permanent. If new inspection data shows a facility is no longer compliant, the FDA can issue an import alert-even for drugs already on the market. This happened in 2021 with Sun Pharma’s Indian facility, where drugs were blocked despite prior approval.
How can I tell if my generic drug was made overseas?
The FDA doesn’t require country-of-manufacture labels on prescription bottles. But most generic drugs sold in the U.S. are made abroad-especially in India and China. You can check the manufacturer’s name on the label and search the FDA’s database of approved facilities to see where it’s based.
Will these changes make generic drugs more expensive?
In the short term, yes. Manufacturers are spending more on compliance-new equipment, training, audits. That cost may trickle up to prices. But long-term, better oversight reduces recalls, shortages, and health risks, which saves money overall. The goal is stable, reliable access-not higher prices.



So let me get this straight-we’re trusting our lives to pills made in factories we’ve never seen, with rules that used to be optional? Wild. I just took my blood pressure med this morning. Hope it’s not secretly made of glitter.
As someone who works in pharma in Hyderabad, I can say this change is long overdue. We’ve been cutting corners for years just to keep prices low. Now? We’re hiring QA staff, installing real-time monitoring, and training everyone like their license depends on it-because it does. The FDA knock on the door? We’re ready. No more hiding. Good for America, good for us.
While the FDA’s shift toward unannounced inspections is statistically significant, one must consider the epistemological foundations of regulatory oversight. The assumption that compliance can be verified through sporadic, reactive audits rather than systemic, proactive accountability structures remains fundamentally flawed. The EU’s Qualified Person model introduces a continuous, legally binding fidelity mechanism-a paradigm shift from enforcement to institutionalized responsibility. Until the U.S. adopts analogous fiduciary duties for importers, we are merely performing regulatory theater.
Okay, I get it, inspections are happening now. But let’s not pretend this is new. I’ve been reading FDA warning letters since 2018. They’ve been flagging the same issues for years. Why now? Because someone got caught on camera? Because a senator got mad? This feels less like reform and more like PR. The system’s still broken. We’re just making it look like we’re fixing it.
Let’s be honest: this isn’t about safety. It’s about control. The FDA doesn’t care if your pills work-they care if you’re American enough to follow their rules. Meanwhile, China’s making the same drugs with better quality and no inspections. And now they’re going to block imports? This is protectionism with a lab coat. Next they’ll ban aspirin because it’s made in a country that doesn’t salute the flag.
India’s been ripping us off for decades. Cheap drugs? Sure. But at what cost? I’ve seen the reports-bacteria in the water, falsified logs, workers paid $2/hour. Now they’re finally getting slapped? Good. If you want to sell to America, you play by American rules. No more free passes. No more ‘cultural differences.’ We don’t need your cheap pills if they’re made in sweatshops with dirty water. Send them back. We’ll make our own.
Yessss!! 🙌 Finally someone’s holding these factories accountable! I’ve been taking generics for 10 years and never knew where they came from. Now I feel a little safer. Also, can we PLEASE put country-of-origin on the bottle? I want to know if my metformin was made in a place with running water 😅
So now we’re gonna punish the global south for being poor? The FDA’s got a budget bigger than some countries’ health ministries and they’re still too lazy to inspect properly? Unannounced inspections? That’s like blaming the kid who didn’t study for the test after you gave him no syllabus. The real problem? Capitalism. Pharma’s profit-driven. Safety’s a footnote. This is just window dressing with a fancy press release.
Hey everyone-just wanted to say this is actually a huge win. A lot of folks think this is just about drugs, but it’s about dignity. The workers in those factories? They’re skilled. They want to do good work. This new system gives them the tools and respect they deserve. No more pressure to fake data. No more fear of getting fired for speaking up. That’s the real win here.
im just glad theyre finally doin somethin. i had a bad reaction to a generic once and the bottle didnt even say where it was made. kinda scary. hope this helps. also, can we get a website where you can type in your med and see where it came from? thatd be awesome.
So the FDA spent 20 years letting foreign plants lie, cheat, and falsify data-and now they’re suddenly gonna fix it? Let me guess: Trump’s EO did it? Not because the FDA cared, but because it was politically convenient? Classic. And now we’re supposed to believe this is about safety? Nah. It’s about optics. The same people who ignored 45% violation rates in 2023 are now posing for photos with inspectors. The real problem? We’ve outsourced our healthcare to a global supply chain and now we’re mad the chain broke. Fix the system, not the inspections.
I come from South Africa, where we’ve been dealing with counterfeit medicines for decades. We don’t have the FDA. We have desperation. So I see this from both sides. Yes, the foreign factories need to be held accountable. But also, the U.S. has been the biggest buyer of cheap generics-creating the demand that incentivized corners being cut. Maybe instead of just punishing factories, we invest in building local manufacturing capacity in low-income countries? Not as a charity, but as a partnership. Because if we don’t, the next crisis won’t be in India or China-it’ll be in a place where no one’s even checking.
Oh wow. The FDA is finally doing something. Took them long enough. I mean, I’m sure the Indian factory workers are just *so* grateful that their livelihoods are being threatened by American regulatory ego. Meanwhile, the real scandal? The fact that the FDA approved 90% of these drugs without ever seeing the facility. But hey, at least now we can all sleep better knowing our pills are being inspected… after the fact. What a revolution.