Understanding Betamethasone and its Uses
Betamethasone is a type of corticosteroid medication that is used to treat a variety of health conditions, such as skin disorders, allergic reactions, and rheumatic disorders. This powerful anti-inflammatory drug works by suppressing the immune system and reducing inflammation in the body. While it is highly effective in treating these conditions, it is important to be aware of the potential side effects and interactions it may have with other medications and health conditions, such as diabetes.
In this article, we will explore the potential impact of betamethasone on blood sugar levels, and what precautions should be taken by individuals with diabetes or those at risk for developing diabetes. We will also discuss the various forms of betamethasone available, and how they may affect blood sugar levels differently.
How Betamethasone Affects Blood Sugar Levels
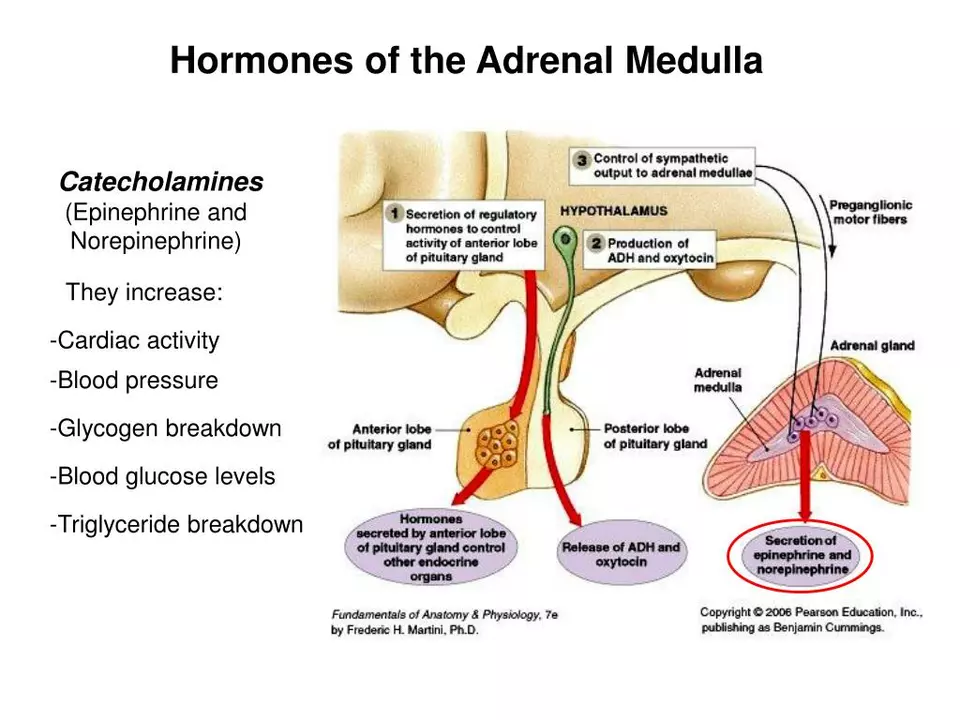
One of the most common side effects of corticosteroid medications, like betamethasone, is their impact on blood sugar levels. This occurs because corticosteroids can increase glucose production in the liver and reduce the sensitivity of cells to insulin, the hormone that helps regulate blood sugar levels. As a result, blood sugar levels can rise, leading to hyperglycemia, or high blood sugar.
For individuals with diabetes or those at risk for developing diabetes, this increase in blood sugar levels can be concerning. It is important to monitor blood sugar levels closely when taking betamethasone, and to work closely with a healthcare provider to manage any changes that may occur. In some cases, adjustments to diabetes medications or insulin dosages may be necessary to maintain proper blood sugar control.
Forms of Betamethasone and their Impact on Blood Sugar
Betamethasone is available in several different forms, including oral tablets, injectable solutions, creams, lotions, and gels. The impact of betamethasone on blood sugar levels can vary depending on the form and dosage of the medication.
Oral and injectable forms of betamethasone tend to have a more significant impact on blood sugar levels, as they are absorbed directly into the bloodstream and have a systemic effect on the body. Topical forms of betamethasone, such as creams and lotions, generally have a lesser impact on blood sugar levels, as they are absorbed through the skin and have a more localized effect.
However, it is still important to monitor blood sugar levels closely when using any form of betamethasone, as individual reactions may vary. Always follow the directions and dosages provided by your healthcare provider, and report any changes in blood sugar levels or other concerns immediately.
Managing Blood Sugar Levels While Using Betamethasone
There are several strategies that can help manage blood sugar levels while using betamethasone. These include:
1. Monitoring blood sugar levels closely: Regularly checking blood sugar levels is crucial when taking betamethasone, especially if you have diabetes or are at risk for developing diabetes. This will help you and your healthcare provider identify any changes in blood sugar levels and make adjustments to your treatment plan as needed.
2. Following a balanced diet: Eating a healthy, balanced diet that is low in simple sugars and high in complex carbohydrates, fiber, and lean protein can help maintain stable blood sugar levels. Be sure to discuss any dietary changes or restrictions with your healthcare provider first.
3. Staying active: Regular physical activity can help improve insulin sensitivity and maintain blood sugar levels. Aim for at least 30 minutes of moderate-intensity exercise most days of the week, but be sure to consult with your healthcare provider before starting a new exercise routine.
4. Communicating with your healthcare provider: Keep your healthcare provider informed about any changes in your blood sugar levels or other concerns related to your betamethasone treatment. They can help you adjust your medications or treatment plan as needed to maintain proper blood sugar control.
Alternatives to Betamethasone for Individuals with Diabetes
If you have diabetes or are at risk for developing diabetes, your healthcare provider may recommend alternative medications to betamethasone that have a lesser impact on blood sugar levels. Some possible alternatives include:
1. Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications, such as ibuprofen and naproxen, can help reduce inflammation and pain without significantly affecting blood sugar levels. However, they may not be as effective for severe inflammation or certain health conditions as corticosteroids like betamethasone.
2. Topical corticosteroids with lower potency: Some topical corticosteroids, such as hydrocortisone, may have a lesser impact on blood sugar levels than more potent corticosteroids like betamethasone. However, they may not be as effective for certain skin conditions or symptoms.
Always discuss any concerns about your medications and their potential impact on blood sugar levels with your healthcare provider. They can help you determine the most appropriate treatment options for your individual needs and health conditions.
Conclusion
Betamethasone is an effective medication for treating various health conditions, but its potential impact on blood sugar levels should not be overlooked. By closely monitoring blood sugar levels, following a balanced diet, staying active, and communicating with your healthcare provider, you can manage blood sugar levels and maintain your overall health while using betamethasone. Always consult with your healthcare provider before making any changes to your medications or treatment plan, and be sure to discuss any concerns about blood sugar levels or other side effects.





I've been on betamethasone for eczema and my sugar spiked so bad I thought I was gonna pass out. Doc said it's normal but still scary as hell.
Worst part? No one warns you.
Oh wow. So we're just supposed to 'monitor' our glucose like it's a cute little pet? Meanwhile my insurance won't cover the test strips but will pay for a $500 steroid cream. Classic.
I'm a type 2 and used betamethasone cream for psoriasis. Didn't realize it was affecting me until I started feeling dizzy after meals. My doc said it was fine but I stopped it anyway. Not worth the risk.
I just want to say that I feel you all. I've been through this. The anxiety of checking your glucose every two hours, the guilt of eating a banana because you're scared it'll spike, the way your partner looks at you like you're a robot when you say 'no sugar' for the 17th time.
It's not just a medication. It's a lifestyle overhaul. And no one talks about the emotional toll. I cried in the pharmacy aisle last week because I couldn't find a sugar-free popsicle. I'm not even joking.
I use the cream for my rash. Never had issues with sugar. Maybe it's the dose? Or maybe I'm just lucky.
I had the same thing happen with prednisone 😔 my sugar went from 110 to 220 in a week. My endo said 'it's temporary' but it felt like my body was betraying me. I'm still scared to try it again even though I need the cream for my dermatitis.
America's healthcare system is a joke. You get a drug that can wreck your metabolism and then charge you $200 for a glucometer. Get your priorities straight. We don't need more steroids. We need better policies.
So basically we're all lab rats for Big Pharma. Betamethasone? More like Betametha-why-did-you-let-this-happen-to-me. The system is rigged. We're just pawns in a game where the only winners are the CEOs with yachts.
You guys are all so brave for sharing this. I just started on the cream and I'm already checking my sugar every morning. It's scary but you're right - awareness is power. Keep speaking up!
I've been using topical betamethasone for years with no issues. But I also eat clean, walk 8k steps a day, and never skip my metformin. Maybe it's not the drug - maybe it's the lifestyle.
In India, we use betamethasone cream for kids with eczema. Sugar spike is rare. Usually under 5% of cases. But yes, monitor.
You think this is bad? Back in my village, we used neem leaves and turmeric paste. No pills. No glucose monitors. No corporate overlords. Just nature and wisdom. Now we're all just broken machines on insulin and anxiety meds.
It is important to note that systemic absorption of topical corticosteroids can vary significantly based on skin integrity, application site, and duration of use. Patients with compromised skin barriers may be at increased risk for metabolic effects.
I've seen this too many times. People get prescribed this and then show up in the ER with DKA. It's preventable. Why aren't pharmacists giving better warnings?
I used the cream and forgot to check my sugar for a week. Ended up in the hospital. Don't be like me. Check it. Every. Day.
They don't want you to know this but betamethasone is part of a larger agenda. The pharmaceutical industry profits from diabetes meds. They know the steroid will spike your glucose. They count on it. They want you dependent. The FDA is in their pocket. Wake up.
Betamethasone? More like Betametha-soul-crusher. I used it for a bad case of poison ivy and suddenly my body felt like a sugar factory with a broken valve. I miss being able to eat a cookie without a panic attack.
I used the cream for my back and my sugar went up but I didn't notice till I started getting really thirsty. I thought I had the flu. Turns out I was pre-diabetic. This stuff is sneaky.
The pathophysiology of corticosteroid-induced hyperglycemia is mediated through gluconeogenesis upregulation, glycogenolysis, and insulin resistance via downregulation of GLUT4 translocation. The clinical relevance is amplified in individuals with latent metabolic syndrome. You're not 'just diabetic' - you're a metabolic outlier in a system designed for homeostasis.