Medication Safety Savings Calculator
Input Your Facility Data
Key Safety Interventions
Estimated Savings
Calculate your potential savings by entering data and selecting interventions
Medication costs are rising fast. In 2023, the average price of a prescription in the UK rose by 10.2%, and hospital systems are feeling the pinch. But cutting corners on drugs isn’t the answer. A single medication error can cost a hospital over £15,000 in extended stays, lawsuits, or readmissions. The real challenge? Saving money without putting patients at risk. The good news? It’s not only possible-it’s already happening in hospitals across the UK and beyond.
Pharmacists Are the Secret Weapon
Most people think of pharmacists as the people who hand out pills. But in top-performing hospitals, they’re clinical decision-makers. A pharmacist reviewing a patient’s full medication list before discharge can catch dangerous interactions, stop unnecessary prescriptions, and switch someone from a £200 brand-name drug to a £5 generic with the same effect. One study of 830 high-risk patients found that pharmacist-led transitions of care saved nearly £1,700 per patient in the first six months after leaving hospital. That’s £1.4 million saved for a single hospital with just 830 patients.These aren’t just busywork checks. Pharmacists trained in pharmacotherapy (BCPS-certified) spot things EHR systems miss. They notice when a patient is still on a drug they were told to stop. They see that a heart failure patient is on three different diuretics, doubling the risk of kidney damage. They ask: Do they really need this? And when they do, they find cheaper, safer alternatives.
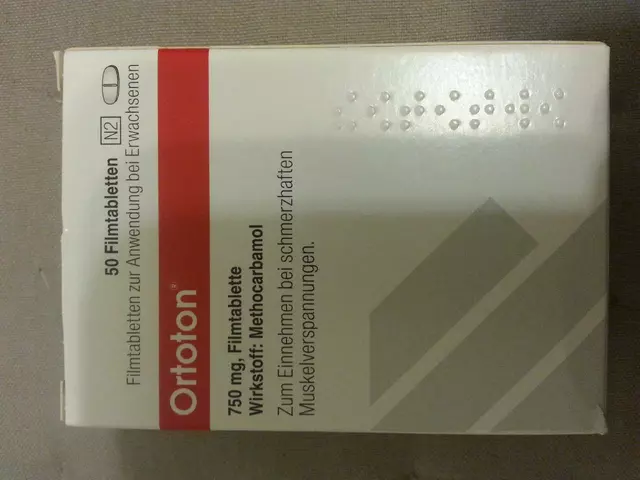
Generic Drugs Work-When Used Right
About 82% of patients in the UK already use generic medications. That’s a win. But here’s the catch: not all generics are created equal. In 2021, a hospital in Manchester switched 400 patients from a branded anticoagulant to a cheaper generic. Within three months, 12 patients had abnormal blood tests. Turns out, the generic had slightly different fillers that affected absorption in older adults with kidney issues. The hospital reversed the switch and added pharmacist-led monitoring. Costs went up a little-but hospitalizations dropped by 60%.Generic drugs are safe when used with clinical oversight. Don’t just swap them blindly. Use them for drugs with wide therapeutic windows (like statins or blood pressure meds). Avoid them for narrow therapeutic index drugs (like warfarin, levothyroxine, or epilepsy meds) unless a pharmacist is involved in the transition. The goal isn’t to pick the cheapest pill-it’s to pick the right pill at the right price.
Standardize Communication-It’s Free
One of the cheapest, most powerful tools in medication safety is a simple 4-step handoff: SBAR. Situation. Background. Assessment. Recommendation. It sounds basic. But in a hospital where a nurse says, “The patient’s BP is low,” and the doctor hears, “Give more fluids,” when the real issue is a missed dose of beta-blocker? That’s how errors happen.After implementing SBAR across all shift changes in a 390-bed hospital in Leeds, adverse drug events dropped by 50%. No new software. No new hires. Just training. Nurses and pharmacists started using the same language. Doctors stopped guessing. Patients got the right meds at the right time. And the hospital saved £300,000 in avoided readmissions in one year.
Ready-to-Administer (RTA) Packs-Costly Upfront, Cheaper Long-Term
RTA packs are pre-filled, unit-dose medications wrapped in blister packs labeled for each patient, each time. They cost 15-20% more per dose than bulk medication. But they cut preparation time by 30%, reduce waste from expired or spilled pills, and eliminate dosing errors during mixing. One NHS trust in Manchester switched to RTA packs for ICU patients. Their pharmacy techs went from spending 4 hours a day preparing IV bags to just 2.5. Medication errors dropped by 45%. Staff burnout decreased. And because fewer patients had adverse reactions, average length of stay fell by 1.2 days. The extra cost? Paid for itself in 8 months.Antimicrobial Stewardship Saves Big
Antibiotics are among the most overused-and most expensive-drugs in hospitals. A patient on IV antibiotics for 7 days might cost £800. Switch them to an oral version on day 3? Cost drops to £40. That’s the power of antimicrobial stewardship.Hospitals with formal antimicrobial programs-where pharmacists review every antibiotic order daily-see 30-40% lower antibiotic use. At Aultman Hospital, this saved $2 million a year. In the UK, one NHS trust cut its antibiotic spend by £450,000 in 18 months by: stopping unnecessary prophylaxis, switching IV to oral early, and avoiding broad-spectrum drugs unless absolutely needed. The bonus? Fewer cases of C. diff infections, which cost £10,000+ per case to treat.
Technology Helps-But Only With People
Barcode scanning, e-prescribing, and automated dispensing machines sound like the future. And they are. But here’s the truth: hospitals that rely only on tech see only a 55% drop in medication errors. Those that combine tech with pharmacists on the floor? 85% drop.Barcodes catch the wrong drug. But only a pharmacist can catch the wrong dose for a kidney patient. E-prescribing stops illegible handwriting. But only a pharmacist can say, “This patient is 87, has three heart conditions, and is on eight drugs-adding another antidepressant is a bad idea.” Technology reduces errors. People prevent them.
What Patients Can Do (Without Breaking the Bank)
Patients aren’t just passive recipients-they’re part of the safety net. Nearly 40% of patients in the UK use at least one cost-saving strategy. Here’s what works:- Ask for generic alternatives-always. Even if it’s not the first option on the script.
- Use mail-order pharmacies for maintenance drugs (like blood pressure or diabetes meds). You can save up to 50% on 90-day supplies.
- Ask your doctor for samples. Many manufacturers still give them out-especially for new or expensive drugs.
- Don’t skip doses to make pills last. It’s dangerous. Instead, ask about patient assistance programs. Most big drugmakers have them.
- Keep a written list of all your meds-including supplements-and bring it to every appointment.
What Doesn’t Work-And Why It’s Dangerous
Some hospitals try to cut costs by cutting staff. That’s a trap. One hospital in Birmingham reduced pharmacy technicians by 30% to save £200,000 a year. Three months later, medication errors jumped 22%. Two patients had severe reactions. One needed intensive care. The hospital paid £1.2 million in legal fees and extended stays. The savings? Gone.Another common mistake: switching to the cheapest generic without checking bioequivalence. For drugs like levothyroxine or warfarin, tiny differences in absorption can cause serious harm. Always involve a pharmacist in these swaps.
And don’t assume patients will speak up. Many won’t. They’re scared, confused, or think asking questions makes them a “difficult” patient. Your job isn’t just to give the right drug-it’s to make sure they understand why they’re taking it.
The Bottom Line: Safety Pays
Every £1 spent on pharmacist-led medication safety programs returns £6.03 in savings. That’s not a guess. It’s from a study at Walter Reed Army Medical Center that tracked over 3,000 patients. It’s backed by the American Society of Health-System Pharmacists. It’s why the NHS is now funding pilot programs to embed pharmacists in GP practices and discharge teams.The future isn’t about choosing between cost and safety. It’s about seeing them as two sides of the same coin. Cut waste. Prevent errors. Use generics wisely. Train staff. Empower patients. And always-always-let the pharmacist be part of the team.
Medication safety isn’t a cost center. It’s a profit center. And the people who know how to make it work? They’re already in your hospital. You just need to let them do their job.
Can using generic drugs really save money without risking safety?
Yes-when done correctly. Generic drugs are safe for most medications, especially those with wide therapeutic windows like statins, blood pressure pills, and antidepressants. But for drugs with narrow therapeutic windows-like warfarin, levothyroxine, or epilepsy meds-switching generics without clinical oversight can lead to dangerous fluctuations. Always involve a pharmacist in these transitions to ensure bioequivalence and monitor patient response.
Do pharmacist-led programs really save money, or are they too expensive to implement?
They save far more than they cost. A single pharmacist-led transition-of-care program can save £2,139 per patient in the first 180 days after discharge. At Walter Reed, every £1 invested in pharmacist services returned £6.03 in healthcare savings. While hiring pharmacists requires upfront investment, the reduction in readmissions, adverse events, and unnecessary prescriptions quickly offsets the cost. Hospitals that delay hiring pharmacists often pay more later in lawsuits, extended stays, and lost reputation.
What’s the biggest mistake hospitals make when trying to cut medication costs?
The biggest mistake is cutting staff-especially pharmacy technicians or pharmacists-to save money short-term. One hospital in the UK reduced pharmacy support staff by 30% and saw a 22% spike in medication errors within three months. That led to £1.2 million in extra costs from patient harm and litigation. Cost-cutting without safety safeguards doesn’t save money-it creates risk and liability.
How can patients help reduce medication costs and improve safety?
Patients can ask for generic alternatives, use mail-order pharmacies for long-term meds, request free samples from doctors, and keep an updated list of all medications-including supplements-to share at every appointment. They should never skip doses to make pills last-instead, ask about patient assistance programs. Being informed and involved reduces errors and helps avoid unnecessary prescriptions.
Is technology enough to ensure medication safety?
No. Technology like barcode scanning and e-prescribing reduces errors by about 55%, but it can’t replace clinical judgment. A system can’t know that a patient’s kidney function dropped last week, or that a new drug interacts with an herbal supplement they’re taking secretly. Only a pharmacist can connect those dots. The most effective systems combine technology with human expertise-especially clinical pharmacists embedded in care teams.





OMG this is SO true!! 🥹 I had a relative who got switched to a generic blood pressure med without any monitoring-ended up in the ER with a near-stroke. Pharmacists are the unsung heroes of healthcare. We need MORE of them, not fewer. Why are we still treating them like pill counters??
Let’s be real-this whole ‘pharmacist-led’ nonsense is just UK socialist healthcare propaganda. In Canada, we don’t need fancy programs. We just tell patients to stop being lazy and take their meds. Also, generics are fine. If your body can’t handle it, maybe you’re just weak.
Ah yes, the eternal dance of capitalism and compassion. We reduce costs by commodifying human life, then pretend to ‘optimize safety’ with pharmacists as emotional laborers. The real tragedy? We don’t pay them enough to heal their own burnout. The system doesn’t want safety-it wants efficiency disguised as care.
Okay but like… I just found out my antidepressant is a generic and I’m basically a lab rat now?? 🤯 I feel violated. Also, why is everyone so obsessed with pharmacists? Are they the new therapists?? 😭
Every time I see someone say ‘just use generics,’ I think of my grandma who took levothyroxine for 15 years and switched brands once. She went from feeling fine to crying in the grocery store for no reason. It’s not about cost-it’s about stability. The body isn’t a spreadsheet. 💙
While the data presented is statistically compelling, one must consider the confounding variables inherent in observational studies conducted within single-institution settings. The generalizability of these findings across heterogeneous healthcare systems remains empirically unverified. Furthermore, the attribution of cost savings to pharmacist intervention may be partially attributable to concurrent quality improvement initiatives.
Pharmacists don’t save money. They just make the system feel better about spending it.
generic good
pharmacist good
staff cut bad
done
My cousin works as a pharmacy tech in Ohio. She says the RTA packs are a godsend-less stress, fewer mistakes. But they’re always short-staffed. The system’s broken, but the people? They’re doing their best. Just give them the tools.
wait so if i use mail order i save 50%?? omg i’ve been overpaying for my diabetes meds for YEARS 😭 i’m switching tomorrow. also why do doctors always act like i’m dumb when i ask about generics??
Pharmacists are the ultimate gatekeepers. They’re the ones who stop the chaos before it hits the patient. If your hospital doesn’t have them on the floor, you’re not running a healthcare system-you’re running a gamble.
Let’s deconstruct this neoliberal mythos of ‘cost-saving’ as if it’s some moral imperative rather than a euphemism for austerity. We’ve turned healing into a profit-and-loss statement, then hired pharmacists to patch the holes with their emotional labor. The real ROI? Not in pounds-but in the dignity of a system that refuses to commodify breath. The pharmacist isn’t a cost center. She’s the last priest in a cathedral of bureaucracy.
In India, we have a similar challenge with counterfeit medications. The solution isn’t just cost control-it’s supply chain integrity. Pharmacists are critical, but so are regulatory frameworks. Without trust in the source, even the best clinical oversight cannot guarantee safety.
Wait-I just read this whole thing… and I’m crying. Not because it’s sad-but because it’s so obvious. We know all this. We’ve had the data for years. Why do we still wait until someone dies before we listen? Pharmacists aren’t ‘extra.’ They’re essential. And if we keep treating them like disposable staff, we’re not saving money-we’re just building a house of cards… and then blaming the wind.