DPP-4 Inhibitor Joint Pain Assessment Tool
Joint Pain Assessment
This tool helps determine if your joint pain might be related to DPP-4 inhibitor medications based on FDA-confirmed patterns.
Assessment Results
If you're taking a DPP-4 inhibitor for type 2 diabetes and suddenly start having bad joint pain, don't just assume it's aging or overuse. This isn't just a coincidence - it's a known side effect that's been confirmed by the U.S. Food and Drug Administration (FDA). Since 2015, all medications in this class have carried a warning about severe, disabling joint pain. And yet, many patients - and even some doctors - still miss the connection.
What Are DPP-4 Inhibitors?
DPP-4 inhibitors are oral diabetes drugs that help control blood sugar by boosting natural hormones that tell your body to release insulin and reduce glucagon. They’re not new - sitagliptin (Januvia) was the first, approved in 2006. Since then, others like saxagliptin (Onglyza), linagliptin (Tradjenta), alogliptin (Nesina), and vildagliptin (Galvus) have joined the list. Together, these drugs are prescribed tens of millions of times each year in the U.S. alone. They’re popular because they’re generally well-tolerated, don’t cause weight gain, and have a low risk of low blood sugar when used alone.
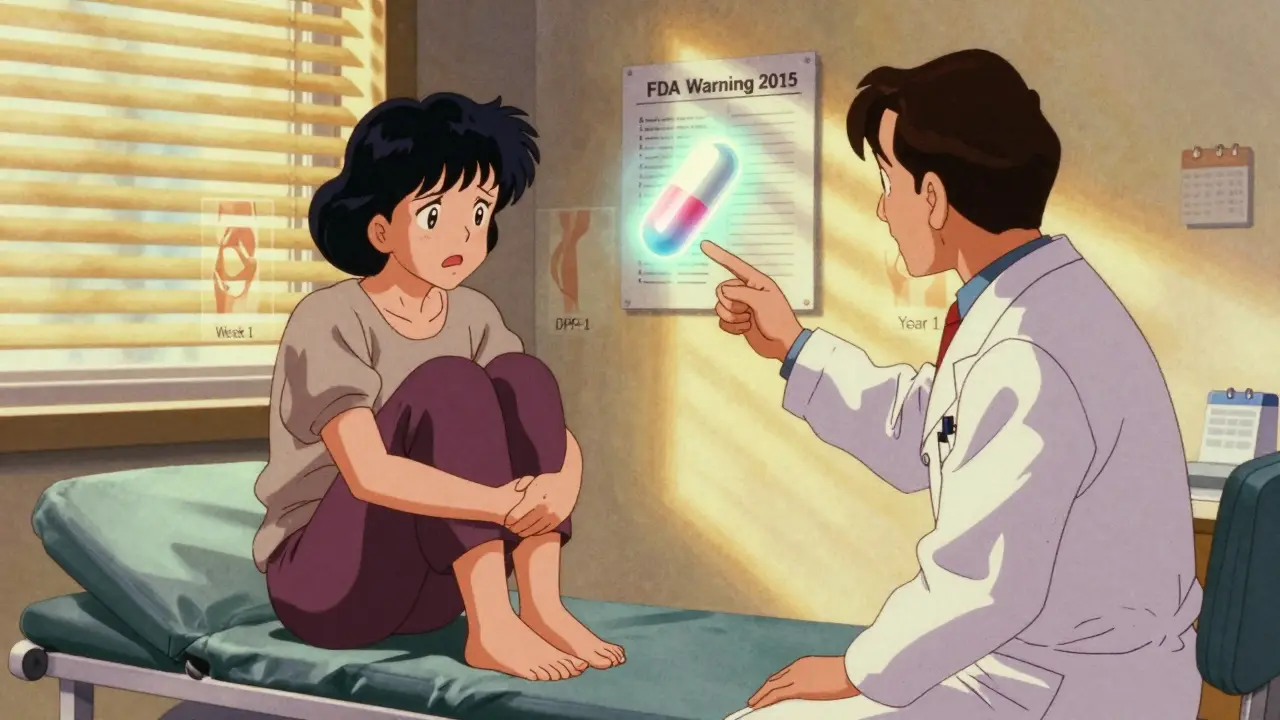
The FDA Warning: What You Need to Know
In August 2015, the FDA issued a formal safety alert after reviewing over 7 years of adverse event reports. They found 33 confirmed cases of severe joint pain directly linked to DPP-4 inhibitors. The pain wasn’t mild. It was bad enough to stop people from walking, working, or doing basic chores. Ten patients had to be hospitalized. In 23 cases, the pain went away within a month after stopping the drug. And in 8 cases, the pain came back - fast - when the patient took the same medication again. That’s a clear sign of cause and effect.
The data breaks down like this: 28 cases tied to sitagliptin, 5 to saxagliptin, 2 to linagliptin, 1 to alogliptin, and 2 to vildagliptin. Five patients had the pain with more than one drug in this class, which suggests the issue isn’t just one drug - it’s likely a class-wide effect.
When Does the Pain Start?
You might think if it’s a side effect, it shows up right away. But it doesn’t always. In 22 of the 33 cases, joint pain began within the first month of taking the drug. But in others, it took months - even up to a year. That’s why it’s easy to miss. Someone might blame arthritis, gout, or an old sports injury. One patient, a 58-year-old woman, developed severe knee pain just three weeks after starting sitagliptin. Her pain vanished two weeks after stopping it. Then, when she accidentally restarted the medication, the pain returned within 48 hours. That kind of pattern is hard to ignore.
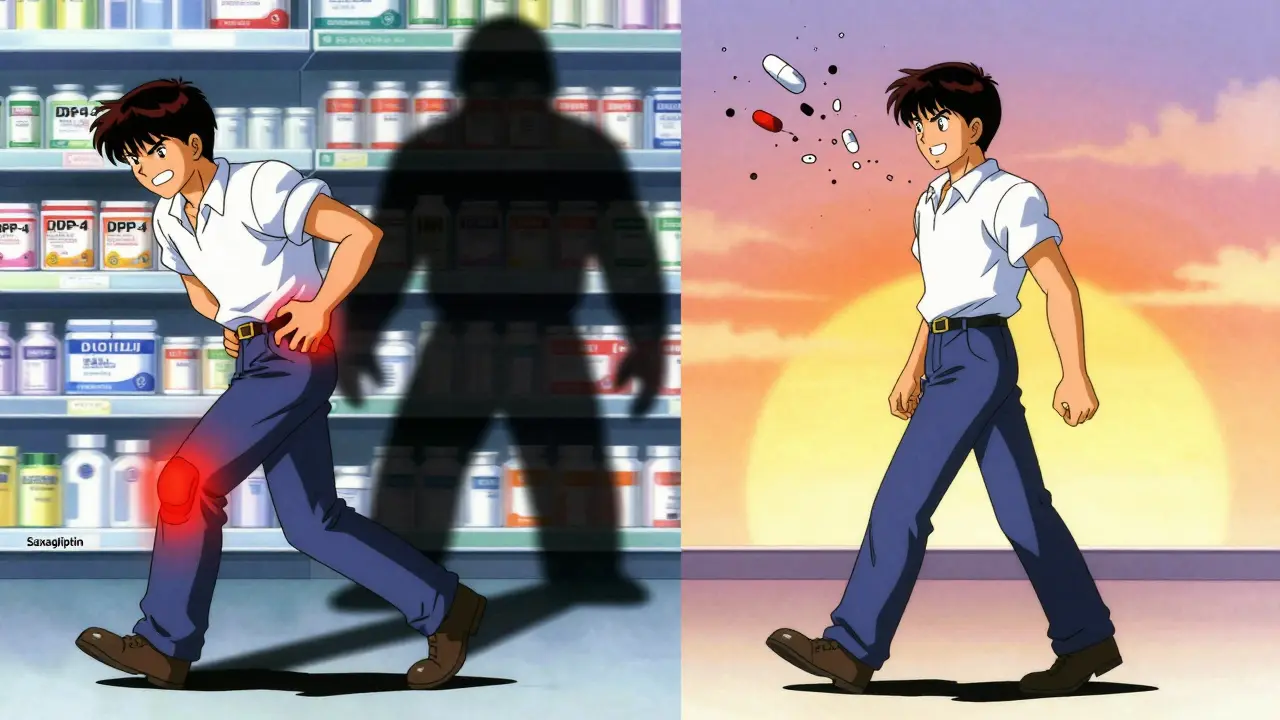
How Bad Is the Pain Really?
It’s not just discomfort. The FDA described it as severe and disabling. Patients reported being unable to walk without help, losing their jobs because they couldn’t stand for long, or needing help just to get dressed. Social media groups for people with diabetes are full of stories where patients were misdiagnosed with rheumatoid arthritis or lupus before someone finally connected the dots to their diabetes pill. One man, after months of failed treatments, stopped his saxagliptin - and within days, his hip and knee pain vanished. He hasn’t had a recurrence since.
What Do Studies Say?
Some studies back up the FDA’s findings. A meta-analysis of 67 clinical trials found a small but statistically significant increase in joint pain among people taking DPP-4 inhibitors (13% higher risk). Another study of older veterans showed a 17% higher chance of joint pain compared to those not on these drugs. But not all research agrees. A large study in Taiwan using insurance claims found no link, though researchers admitted their data might have missed severe cases because of how diagnoses were coded.
What’s clear is this: the risk isn’t high for everyone. But when it happens, it can be devastating. The American Diabetes Association says the absolute risk is low compared to how many people take these drugs - but that doesn’t mean it’s not real for the people it affects.
What Should You Do?
If you’re on a DPP-4 inhibitor and you start having new, unexplained joint pain - especially if it’s in multiple joints, worse at rest, or doesn’t improve with rest or over-the-counter painkillers - talk to your doctor right away. Don’t stop the drug on your own. The FDA says: keep taking it until you’ve spoken to your provider. Abruptly stopping could cause your blood sugar to spike.
Your doctor should consider whether this could be drug-related. They may ask you to temporarily stop the medication to see if symptoms improve. If they do, and the pain goes away, that’s a strong clue. If you restart it and the pain returns? That’s confirmation.
Other Side Effects to Watch For
Joint pain isn’t the only possible side effect. DPP-4 inhibitors have also been linked to:
- Pancreatitis (inflammation of the pancreas)
- Severe allergic reactions (like swelling of the face or throat)
- Bullous pemphigoid (a serious skin condition with blisters and peeling)
- Low blood sugar (especially if combined with sulfonylureas or insulin)
Januvia’s prescribing info specifically says to call your doctor if you develop blisters or skin erosion. These aren’t common, but they’re serious. Always report unusual symptoms - even if they seem unrelated.
What’s the Bottom Line?
DPP-4 inhibitors work well for millions of people with type 2 diabetes. For most, the benefits far outweigh the risks. But if you’re one of the rare people who develops severe joint pain, it’s not in your head. It’s real. And it’s reversible. The key is recognizing it early. Don’t wait for it to get worse. Don’t assume it’s just old age. Don’t let your doctor brush it off. This side effect is documented, studied, and tracked. You have the right to ask: Could this be the medication?
Keep a journal: note when the pain started, where it hurts, how bad it is, and whether anything makes it better or worse. Bring this to your next appointment. It might be the piece of evidence that helps you get relief.
Can DPP-4 inhibitors cause joint pain even after years of use?
Yes. While most cases of joint pain linked to DPP-4 inhibitors occur within the first month, the FDA has documented cases where symptoms didn’t appear until after a year of continuous use. This delay makes it harder to connect the dots, but it doesn’t rule out the drug as the cause. If you’ve been on one of these medications for a long time and suddenly develop severe joint pain, it’s still worth discussing with your doctor.
Does everyone who takes DPP-4 inhibitors get joint pain?
No. Severe, disabling joint pain is rare. Clinical trials show about 5-10% of people report mild joint discomfort, but only a small fraction experience the severe, disabling form. The FDA identified 33 confirmed cases out of millions of prescriptions. That means the risk is low - but it’s real enough to warrant attention.
If I stop the drug, will the joint pain go away?
In most cases, yes. The FDA found that 23 out of 33 patients saw their joint pain resolve within one month of stopping the medication. For some, relief came in just days. If the pain returns after restarting the drug, that’s a strong indicator it was caused by the medication. Always consult your doctor before stopping any diabetes medication.
Are some DPP-4 inhibitors more likely to cause joint pain than others?
Sitagliptin (Januvia) was linked to the most cases - 28 out of 33 - but that’s likely because it’s the most prescribed. The FDA found that 5 patients developed joint pain with more than one DPP-4 inhibitor, suggesting the issue affects the entire class. So while one drug might be more commonly reported, the risk appears to be shared across all of them.
Should I switch to a different diabetes medication if I have joint pain?
It depends. If your joint pain is severe and you suspect it’s linked to your DPP-4 inhibitor, your doctor may recommend switching to another class of diabetes drugs - like SGLT2 inhibitors (e.g., empagliflozin) or GLP-1 receptor agonists (e.g., semaglutide). These alternatives also help with blood sugar control and may have different side effect profiles. Never switch on your own. Work with your provider to find the safest option for your health.






I was on Januvia for two years and never thought my knee pain was related until I read this. I stopped it last month, and within 10 days, I could walk without wincing. My doctor was skeptical, but I brought the FDA alert. Now he’s checking everyone on DPP-4s. Don’t ignore it. It’s not 'just aging.'