When you start a new medication, you’re not just choosing a drug-you’re choosing a set of risks. Whether it’s a prescription pill, an over-the-counter painkiller, or a herbal supplement bought online, each one comes with its own pattern of possible side effects. And not all side effects are created equal. Some are mild and temporary. Others can be serious, even life-threatening. The key is understanding which class of medication you’re taking and how that changes what to watch for.
Prescription Drugs: Consistent, But Not Risk-Free
Prescription medications go through years of testing before they hit the market. The FDA requires clinical trials to prove they work and to map out their side effects. That’s why you get detailed leaflets with your pills. But even with all that scrutiny, side effects still happen. Take antibiotics, for example. About 5% of people develop a rash after taking them. It’s not rare. It’s expected. And it’s not always an allergy-it can just be your body reacting to the chemical structure. The bigger issue comes when switching between brand-name and generic versions. The FDA says generics must be bioequivalent-meaning they deliver the same active ingredient at the same rate and amount. In practice, that’s usually true. For most drugs like statins, blood pressure meds, or antidepressants, switching from brand to generic doesn’t change much. Studies of over 800 patients found no meaningful difference in outcomes for drugs like beta-blockers or ACE inhibitors. But there’s a catch. The inactive ingredients? Those aren’t regulated the same way. Lactose, dyes, preservatives-these fillers can trigger reactions in sensitive people. If you’re lactose intolerant, a generic version of your thyroid medication might give you bloating and cramps, even though the active ingredient is identical. Some people actually do better on generics because they’re allergic to something in the brand-name version. It’s not about quality. It’s about ingredients.Narrow Therapeutic Index Drugs: Tiny Changes, Big Consequences
Then there are the drugs where even a 5% difference in absorption can be dangerous. These are called narrow therapeutic index (NTI) drugs. They sit right on the edge between helping and harming. Levothyroxine (for hypothyroidism) and warfarin (a blood thinner) are two of the most common. A tiny shift in how your body absorbs the drug can mean your thyroid levels go too high-or your blood won’t clot properly. That’s why doctors and pharmacists urge caution when switching between brand and generic versions of these drugs. Even switching between two different generic brands can cause problems. One patient might do fine on one generic version of levothyroxine, but then switch to another-and suddenly feel fatigued, shaky, or have heart palpitations. That’s not the drug failing. It’s the formulation. The body doesn’t treat all pills the same, even if the label says they’re identical. Studies from 2008 showed that patients on generic antiepileptic drugs who switched brands had more seizures and needed more doctor visits. That’s not because generics are bad. It’s because for NTI drugs, consistency matters. If your thyroid med works, stick with the same manufacturer. Don’t let the pharmacy swap it out without telling you.
Over-the-Counter (OTC) Medications: The Hidden Risks
OTC drugs like ibuprofen, acetaminophen, or antihistamines feel harmless because you can buy them without a prescription. But they’re still powerful chemicals. Taking too much acetaminophen can cause liver failure. Long-term use of NSAIDs like ibuprofen can lead to stomach ulcers or kidney damage. And many people don’t realize they’re doubling up-taking a cold medicine with acetaminophen on top of their daily painkiller. Even “natural” OTC products like melatonin or magnesium supplements aren’t risk-free. Melatonin can make you groggy the next day. Magnesium can cause diarrhea at high doses. And because these aren’t regulated like prescription drugs, the actual dose in the bottle might not match what’s on the label. One 2023 review found some supplements contained 20% more or less than claimed. The real danger? Combining OTC meds with prescriptions. A common mix: ibuprofen and blood pressure meds. Together, they can reduce the effectiveness of the blood pressure drug and strain the kidneys. Or, taking antihistamines with sleep aids-both cause drowsiness. Stack them, and you might not wake up safely.Herbal Supplements: The Wild West of Medication
Herbal remedies and dietary supplements are the most unpredictable class. They’re not tested for safety or effectiveness before sale. The FDA can’t stop them from being sold unless they prove they’re dangerous-which often happens only after people get hurt. Echinacea, often taken for colds, can trigger asthma attacks, hives, or muscle aches in some people. Feverfew, used for migraines, has been shown in animal studies to cause uterine contractions. Pregnant women who take it risk miscarriage. St. John’s Wort, promoted as a natural antidepressant, can cause serotonin syndrome when mixed with SSRIs like Lexapro or Zoloft. Symptoms? Tremors, high fever, rapid heartbeat-sometimes fatal. Ginkgo biloba and chamomile increase bleeding risk. If you’re on warfarin or aspirin, adding these herbs can turn a minor cut into a serious bleed. And because these supplements aren’t tracked in medical records, doctors often don’t know patients are taking them. That’s why it’s critical to tell your pharmacist or doctor about every pill, powder, or tea you swallow-even if you think it’s “just herbal.”
How to Stay Safe: A Simple Checklist
You don’t need to avoid all medications. You need to manage them wisely. Here’s what to do:- Know your active ingredient. If you’re on lisinopril for blood pressure, don’t switch to another brand unless your doctor approves. Same active ingredient, but different fillers can still cause issues.
- Check the inactive ingredients. Look at the label. If you’re allergic to sulfites, lactose, or soy, avoid pills that list them. Generic versions often change fillers without changing the name.
- Don’t assume “natural” means safe. Echinacea, ginkgo, St. John’s Wort-all have documented risks. Treat them like drugs, not tea.
- Track interactions. Alcohol can react badly with antibiotics, sedatives, and even some painkillers. It doesn’t just make you sleepy-it can stop your liver from processing the drug properly.
- Stick with one pharmacy. They can flag dangerous combinations. If you switch pharmacies, you lose that safety net.
- Monitor for changes. If you start a new drug or switch generics and feel different-fatigue, dizziness, rash, nausea-don’t ignore it. Call your doctor. It might not be “all in your head.”
Why This Matters Now
Insurance companies are pushing harder for generic drugs. Step therapy means you have to try the cheaper option first. That’s fine-for most people. But for those on NTI drugs, or with allergies to fillers, it can backfire. Pharmacists are now trained to flag these cases, but you have to speak up. If your thyroid med suddenly doesn’t feel right after a refill, ask: “Is this the same brand?” The future may bring personalized medicine-genetic tests to match you with the right drug. But that’s still years away. Right now, your best protection is awareness. Medication isn’t one-size-fits-all. Side effects aren’t random. They’re tied to the class, the formulation, and your body’s unique response. Know your drugs. Know your risks. And never assume a pill is harmless just because it’s cheap or labeled “natural.”Are generic drugs always as safe as brand-name drugs?
For most medications, yes. Generic drugs contain the same active ingredient and must meet FDA bioequivalence standards. But inactive ingredients-like fillers, dyes, or preservatives-can differ. These can trigger allergies or intolerances in sensitive people. For example, a generic version of a thyroid pill might contain lactose, which can cause stomach issues in lactose-intolerant individuals. The drug works the same, but your body might react differently.
Can herbal supplements really interact with prescription medications?
Absolutely. St. John’s Wort can cause dangerous serotonin buildup when taken with antidepressants, leading to tremors, high fever, or even death. Ginkgo and chamomile increase bleeding risk when combined with warfarin or aspirin. Echinacea can interfere with liver enzymes that break down many drugs, making them stronger or weaker than intended. These aren’t rare cases-they’re documented in medical literature. Always tell your doctor what supplements you’re taking.
Why are narrow therapeutic index (NTI) drugs so risky when switching generics?
NTI drugs like levothyroxine and warfarin have a very small window between an effective dose and a toxic one. Even a 5% difference in how your body absorbs the drug can push you out of that safe range. One study showed patients switching between generic versions of levothyroxine had abnormal thyroid levels within weeks. That’s why doctors recommend sticking with the same manufacturer-especially for these drugs. Don’t let your pharmacy switch it without checking with you first.
What should I do if I think a new medication is causing side effects?
Don’t stop taking it suddenly unless it’s an emergency (like swelling, trouble breathing, or chest pain). Instead, write down exactly what you’re feeling, when it started, and whether you changed anything-new drug, different brand, added a supplement. Call your doctor or pharmacist. Many side effects are mild and temporary, but some need adjustment. Your body might just need time to adapt. But if symptoms worsen or you’re unsure, get it checked. It’s better to be safe than sorry.
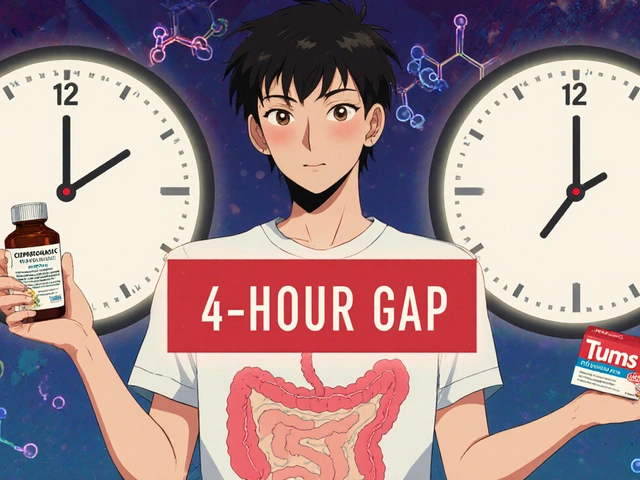
Is it safe to take OTC painkillers with my prescription blood pressure medicine?
It depends. NSAIDs like ibuprofen or naproxen can reduce the effectiveness of some blood pressure medications and increase strain on your kidneys. If you’re on an ACE inhibitor or diuretic, mixing these can be risky. Acetaminophen is usually safer for occasional use, but even that can be harmful if taken too often or with alcohol. Always check with your pharmacist before combining OTC and prescription drugs. They can spot interactions you might miss.
Why do some people do better on brand-name drugs than generics?
It’s usually not about the active ingredient. It’s about the fillers or how the pill is made. Some people are sensitive to dyes, gluten, or other inactive components in the brand-name version. Switching to a generic without those ingredients can actually improve their tolerance. In rare cases, the dissolution rate-the way the drug releases in the body-can vary slightly. For most drugs, this doesn’t matter. For NTI drugs, it can. If you feel worse after switching, it’s worth discussing with your doctor.






Wow, this is such a needed post. I’ve had to fight with my pharmacy three times because they switched my levothyroxine brand without telling me-and I ended up in the ER with atrial fibrillation. Never assume ‘bioequivalent’ means ‘identical.’ The fillers? They matter. Always check the inactive ingredients. Always.
LET ME TELL YOU SOMETHING-this isn’t just about pills, it’s about SYSTEMS FAILING US. Insurance companies push generics like they’re candy. Pharmacists swap them like trading cards. And then we’re left wondering why we feel like garbage. I switched from brand to generic for my blood pressure med-and my heart started racing like I’d downed three espressos. It wasn’t in my head. It was in the lactose. And no one warned me. #WakeUp
Thank you for this thorough breakdown. I appreciate how you distinguish between active ingredients and excipients-it’s a critical point often overlooked. Many patients don’t realize that even minor changes in formulation can trigger physiological responses, especially with NTI drugs. This is precisely why medication reconciliation should be standard practice during every pharmacy visit.
Of course you’re ‘allergic’ to lactose. Of course you ‘feel different’ after switching generics. Everyone’s sensitive. But you know what? You’re not special. You just didn’t read the label. If you can’t read ‘lactose’ or ‘FD&C Red No. 40,’ maybe you shouldn’t be managing your own meds. This isn’t a conspiracy-it’s basic pharmacology. Stop blaming the system and start reading the tiny print.
OMG I’M SO GLAD SOMEONE FINALLY SAID THIS 😭😭😭 I’ve been on St. John’s Wort for 3 years ‘for anxiety’-then started Lexapro and almost died. I thought it was ‘just herbs’… until my hands shook like I was in a snowstorm and my temperature hit 104. ER. ICU. Now I tell EVERYONE. Herbal = not harmless. 🚨🩸 #SerotoninSyndromeIsReal
As someone who works in global health, I’ve seen how this plays out in underserved communities. People take OTC meds because they can’t afford prescriptions-and they combine them with traditional remedies without knowing the risks. The real tragedy isn’t just the side effects-it’s the lack of accessible, culturally competent education. We need more community pharmacists, not just corporate ones.
NTI drugs require pharmacokinetic precision-any deviation in Cmax or AUC can precipitate therapeutic failure or toxicity. Generic bioequivalence thresholds (80–125%) are statistically acceptable but physiologically perilous for drugs like warfarin or levothyroxine. The FDA’s ‘same active ingredient’ standard is a regulatory loophole, not a safety guarantee. Always request the manufacturer’s lot number. Document everything.
I used to think generics were fine until I started having migraines after switching my antidepressant. Turned out the new version had a dye I was sensitive to. I didn’t even know I was sensitive until I stopped and switched back. Now I keep a list of every filler I can’t tolerate. It’s annoying, but it’s saved me from a lot of pain.
My mom had a stroke because her pharmacist switched her warfarin brand without telling her. The INR went from 2.4 to 5.1 in two weeks. She didn’t feel different. No bruising, no bleeding. Just… stroke. They didn’t catch it until it was too late. This isn’t theoretical. It’s life or death. Always ask. Always check.
so like i took some turmeric for my knee and then got dizzy and my blood pressure dropped. i thought it was the heat. turns out it was the herb. now i just take ibuprofen. simpler. less drama.
This is one of the most important posts I’ve read all year. We’re taught to trust pills because they’re FDA-approved, but we’re never taught how to read the fine print. I’m so grateful for the checklist. I’m printing it out and taping it to my medicine cabinet. Knowledge isn’t power-it’s protection.
USA thinks it’s so advanced but you guys still don’t know your own medicines? In India we just take what the doctor says and don’t question. You people overthink everything. Also St John’s Wort? We call it ‘dope tea’ and it’s free at the temple. You’re all so scared of natural things. Chill.
One must question the ontological status of pharmaceutical identity: if two pills contain identical active ingredients, are they ontologically equivalent? Or is the body a phenomenological field wherein the excipient becomes a metaphysical variable? The pill, in its inert form, is a cipher; but in its ingestion, it becomes a conduit of corporeal alienation. The FDA’s bioequivalence standard is a colonial relic-a quantification of the soul’s chemistry.
People like you think you’re being ‘proactive’ by reading labels, but you’re just reinforcing the medical-industrial complex. The real problem? Pharma owns the FDA. The ‘side effects’ are designed to keep you coming back. Stop trusting the system. Go off all meds. Eat turmeric. Meditate. The body heals itself-if you stop poisoning it.
There’s a quiet tension here between standardization and individuality. We want drugs to be predictable, yet our bodies are wildly variable. Perhaps the future isn’t in better generics, but in personalized dosing-tailored not just to genetics, but to lived experience, diet, stress, even sleep patterns. The pill is a blunt instrument. Maybe it’s time we stopped treating it like a scalpel.