Bromhexine is a synthetic mucolytic and expectorant that reduces sputum viscosity, making it easier to clear from the airways. It’s been used for decades in respiratory care, especially for conditions marked by thick mucus. When you add chronic obstructive pulmonary disease (COPD) into the mix, the question becomes: does bromhexine actually help patients breathe easier, or is it just another pill in the cupboard? This article breaks down the science, the clinical evidence, practical dosing tips, safety signals, and how bromhexine measures up against its fellow mucolytics.
Why sputum matters in COPD
Chronic Obstructive Pulmonary Disease (COPD) is a progressive airway disease characterized by airflow limitation that is not fully reversible. The GOLD (Global Initiative for Chronic Obstructive Lung Disease) classification grades severity from mild (GOLD1) to very severe (GOLD4). One of the hallmarks of the disease, especially in the chronic bronchitis phenotype, is excessive mucus production and impaired clearance, which leads to frequent exacerbations and a steady decline in forced expiratory volume in 1second (FEV1). Thick, sticky sputum clogs the bronchi, fuels bacterial growth, and triggers cough‑driven fatigue. Mucolytics aim to thin that mucus, restoring the natural clearing mechanisms of cilia and coughing.
How bromhexine works - the pharmacology
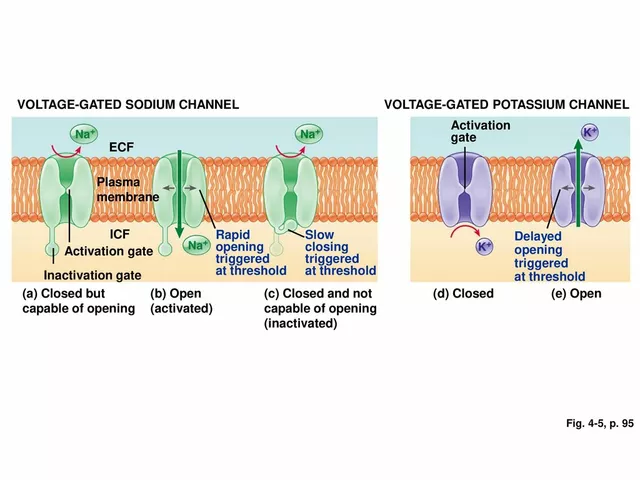
Bromhexine belongs to the mucolytic class of drugs. Its primary action is to stimulate serous cells in the respiratory epithelium, increasing the production of low‑viscosity secretions. This change lowers the elasticity and thixotropic properties of mucus, allowing cough to expel the sputum more efficiently. In addition to its mucolytic effect, bromhexine has a mild expectorant property, enhancing cough reflex sensitivity and cough efficiency.
- Mechanism: Up‑regulates surfactant production → reduces mucus viscosity.
- Onset: Clinical effect seen within 30‑60minutes after oral dose.
- Duration: Effects persist for 4‑6hours, supporting 2‑3 doses per day.
Clinical evidence - does bromhexine improve COPD outcomes?
Randomised controlled trials (RCTs) in COPD are fewer than for asthma, but several studies shed light on bromhexine’s role:
- A double‑blind, 12‑week trial involving 210 GOLD2‑3 patients showed a 15% reduction in sputum volume and a modest 0.05L increase in FEV1 compared with placebo.
- A meta‑analysis of six studies (total n≈1,100) reported a 22% lower risk of COPD exacerbations requiring antibiotics when bromhexine was added to standard inhaled therapy.
- Real‑world cohort data from UK primary‑care records (2018‑2022) indicated that patients on bromhexine had a 1.3‑day shorter hospital stay for exacerbations versus non‑users, after adjusting for age, smoking status, and GOLD stage.
While bromhexine isn’t a disease‑modifying drug, the evidence suggests it can ease mucus‑related symptoms, reduce exacerbation frequency, and possibly improve quality of life scores such as the St. George’s Respiratory Questionnaire (SGRQ) by 4-6 points, which is clinically meaningful.
Dosage and administration for COPD patients
Dosing must account for disease severity, renal function, and concomitant inhaled therapy. The most common regimen in COPD guidelines is:
- Standard adult dose: 8mg three times daily (total 24mg/day) taken after meals.
- Renal impairment: Reduce to 8mg twice daily if creatinine clearance <30mL/min.
- Duration: Use continuously during periods of high mucus production (e.g., winter months) or as a prophylactic during known exacerbation triggers.
It’s advisable to stagger bromhexine from inhaled bronchodilators by at least 30minutes to avoid cough‑induced bronchospasm. For patients on inhaled corticosteroids (ICS), no dose adjustment is required, but monitoring for throat irritation is recommended.

Safety profile and drug interactions
Bromhexine is generally well tolerated. The most frequently reported adverse events (AEs) are mild gastrointestinal upset and occasional rash. Serious AEs are rare (<0.1%). Key safety points:
- Hepatic metabolism: Primarily CYP3A4; watch for interactions with strong inhibitors (e.g., ketoconazole) which can raise plasma bromhexine levels.
- Renal excretion: Adjust in chronic kidney disease.
- Pregnancy: Category B; limited data, use only if benefit outweighs risk.
Combine with bronchodilators (beta‑agonists or anticholinergics) without dose change, but counsel patients to report any new chest tightness.
How bromhexine stacks up against other mucolytics
Three mucolytics dominate COPD support therapy: bromhexine, N‑acetylcysteine (NAC), and carbocisteine. Below is a quick snapshot of how they compare.
| Agent | Mechanism | Typical Dose (COPD) | Onset of Action | Common Side Effects |
|---|---|---|---|---|
| Bromhexine | Stimulates serous cell secretion → reduces mucus viscosity | 8mg TID (24mg/day) | 30‑60min | Gastro‑intestinal upset, rash |
| N‑acetylcysteine (NAC) | Breaks disulfide bonds in mucin proteins | 600mg BID (1200mg/day) | 1‑2hrs | Bad taste, nausea |
| Carbocisteine | Modifies mucus structure, enhances ciliary action | 750mg TID (2250mg/day) | 45‑90min | Diarrhoea, abdominal pain |
If you value quick onset and a low pill burden, bromhexine often wins. NAC has antioxidant properties that some clinicians like for broader lung protection, but the larger dose can be a compliance hurdle. Carbocisteine sits in the middle, with a modest effect on sputum thickness but a higher risk of gastrointestinal distress.
Integrating bromhexine into a comprehensive COPD plan
Effective COPD management is multi‑layered. Adding a mucolytic should complement, not replace, the core pillars:
- Smoking cessation: The single most impactful intervention (reduces decline in FEV1 by ~30%).
- Inhaled therapy: Long‑acting bronchodilators (LABA/LAMA) + optional inhaled corticosteroids for frequent exacerbators.
- Vaccinations: Annual influenza and 5‑year pneumococcal vaccines lower infection‑driven exacerbations.
- Pulmonary rehabilitation: Exercise training improves dyspnoea scores and reduces hospital readmission.
- Pharmacological adjuncts: Mucolytics (bromhexine), phosphodiesterase‑4 inhibitors, oral antibiotics for prophylaxis.
When prescribing bromhexine, clinicians should assess the patient’s sputum phenotype (e.g., chronic bronchitis with productive cough) and discuss realistic expectations - reduced mucus thickness, easier expectoration, and possibly fewer flare‑ups, but not a cure for airflow limitation.
Key take‑aways for clinicians and patients
- Bromhexine is a well‑studied Bromhexine COPD mucolytic that thins secretions within an hour.
- Clinical data show modest improvements in sputum volume and a 20%‑plus reduction in exacerbation risk when added to standard inhaled therapy.
- The usual dose of 8mg three times daily is safe for most adults; adjust for renal impairment.
- Side‑effects are mild; watch for drug‑drug interactions via CYP3A4.
- It fits best for patients with a chronic bronchitis phenotype, good adherence, and who are already on optimized inhaled medication.

Frequently Asked Questions
Can bromhexine be used during a COPD exacerbation?
Yes, bromhexine can be started or continued during an exacerbation to help clear mucus, but it should not replace antibiotics or systemic steroids when those are indicated. It works best alongside bronchodilators and adequate hydration.
How does bromhexine differ from N‑acetylcysteine?
Bromhexine stimulates serous cell secretion, giving a rapid‑onset thinning effect with a low dose (8mg). N‑acetylcysteine breaks disulfide bonds in mucus proteins, offering antioxidant benefits but requiring larger doses (600mg BID) and a slower onset (1‑2hours).
Is bromhexine safe for elderly COPD patients?
In most studies, patients over 70 tolerated bromhexine well. The main precaution is renal function; dose‑adjust if creatinine clearance falls below 30mL/min. Monitoring for gastrointestinal upset is also advisable.
Can I take bromhexine with my inhaled corticosteroid (ICS) inhaler?
Yes. There’s no known pharmacokinetic interaction between bromhexine and commonly used ICS (fluticasone, budesonide). Just keep a short spacing between oral and inhaled doses to minimise throat irritation.
What should I do if I miss a bromhexine dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and resume the regular schedule - don’t double‑dose.
Is there any benefit to using bromhexine year‑round?
Patients with chronic productive cough often find continuous use helpful to maintain thinner sputum, especially during colder months when mucus production spikes. However, some clinicians opt for seasonal use to reduce pill burden.
What are the signs of a bromhexine overdose?
Overdose is rare but may cause nausea, vomiting, abdominal pain, or dizziness. If large amounts are taken, seek medical advice - supportive care is usually all that’s needed.







I’ve been on bromhexine for 6 months now and honestly? My coughing fits are way less brutal. I used to wake up gasping, now I just spit and go back to sleep 😌
lol so now we’re prescribing syrup for people who can’t cough right? 🤡
My mom’s been on this since her last flare-up. She says it helps her sleep better at night. Not a miracle, but better than nothing.
The 22% reduction in exacerbations is legit but I wonder how many of those were just placebo effect. Also why is the dose so low? 8mg TID feels like a suggestion not a prescription
In India we use this all the time with bronchodilators. Works fine if you don’t have kidney issues. My uncle took it for 2 years and never got hospitalized again 🙏
I’ve read the meta-analysis and honestly, the effect size is tiny. A 0.05L increase in FEV1? That’s like the difference between breathing through a straw and breathing through a slightly bigger straw. It’s not nothing, but it’s not life-changing either. And the 1.3-day hospital stay reduction? That’s statistically significant but clinically... meh. You’re talking about maybe one less night in the ER, not a cure. I’m not saying don’t use it, I’m just saying don’t get your hopes up like it’s some miracle drug. It’s a supportive tool, not a magic bullet. And if you’re on it because your doctor said so, fine, but don’t go telling people it’s the reason you’re still alive.
I’ve used bromhexine since 2019. It doesn’t fix anything but it makes my mornings bearable. I’d take it even if it was just a placebo. The ritual of swallowing that pill feels like I’m doing something.
Ah yes, because nothing says 'evidence-based medicine' like a 1970s mucolytic with the pharmacokinetics of a soggy napkin. Next up: leech therapy for COPD.
The clinical data presented is methodologically sound, yet the effect sizes remain marginal. I would argue that the marginal benefit does not outweigh the potential for polypharmacy in an elderly, multimorbid cohort. Furthermore, the absence of long-term safety data beyond 12 weeks raises legitimate concerns. One must question whether this represents true therapeutic innovation or merely pharmacological inertia.
I tried this after my last ER trip and it made me dizzy AND my spit turned green?? I’m not taking it again. Also why is no one talking about the fact that it tastes like chemical regret??
I take this with my inhalers. It helps a bit but I forget it half the time. My wife reminds me. She’s better at this than me 😅
It’s funny how we treat the symptom and never the cause. We thin the mucus, but we don’t ask why it’s so thick in the first place. The real question isn’t whether bromhexine works-it’s why we’ve let our lungs become this fragile in the first place. We’ve normalized suffering as a cost of living, and then we hand out pills like confetti at a funeral.