BV Intimacy Impact Calculator
Bacterial Vaginosis can affect your intimate life. This tool helps you understand symptom severity and estimate when you may safely resume sexual activity after treatment.
Symptom Assessment
Select symptoms you're experiencing:
Treatment Information
Imagine getting ready for a night out, feeling confident, only to have a lingering worry about an invisible guest that could ruin the mood. Bacterial Vaginosis isn't just a medical term - it can creep into the bedroom and mute the spark that intimacy relies on.
Key Takeaways
- Bacterial Vaginosis alters the natural balance of the vaginal microbiome, leading to noticeable symptoms.
- These symptoms often cause anxiety, reduced desire, and awkwardness during sex.
- Untreated BV raises the risk of STIs, pregnancy complications, and recurrent infections.
- Effective treatment includes antibiotics like metronidazole, lifestyle tweaks, and sometimes probiotics.
- Open communication with partners and preventive habits can keep intimacy enjoyable.
What Is Bacterial Vaginosis?
Bacterial Vaginosis is a common vaginal condition caused by an overgrowth of certain anaerobic bacteria that displace healthy lactobacilli. It isn't classified as a sexually transmitted infection, but sexual activity can shift the bacterial balance and trigger symptoms. Around 1 in 3 women will experience it at some point, often between the ages of 20 and 40.
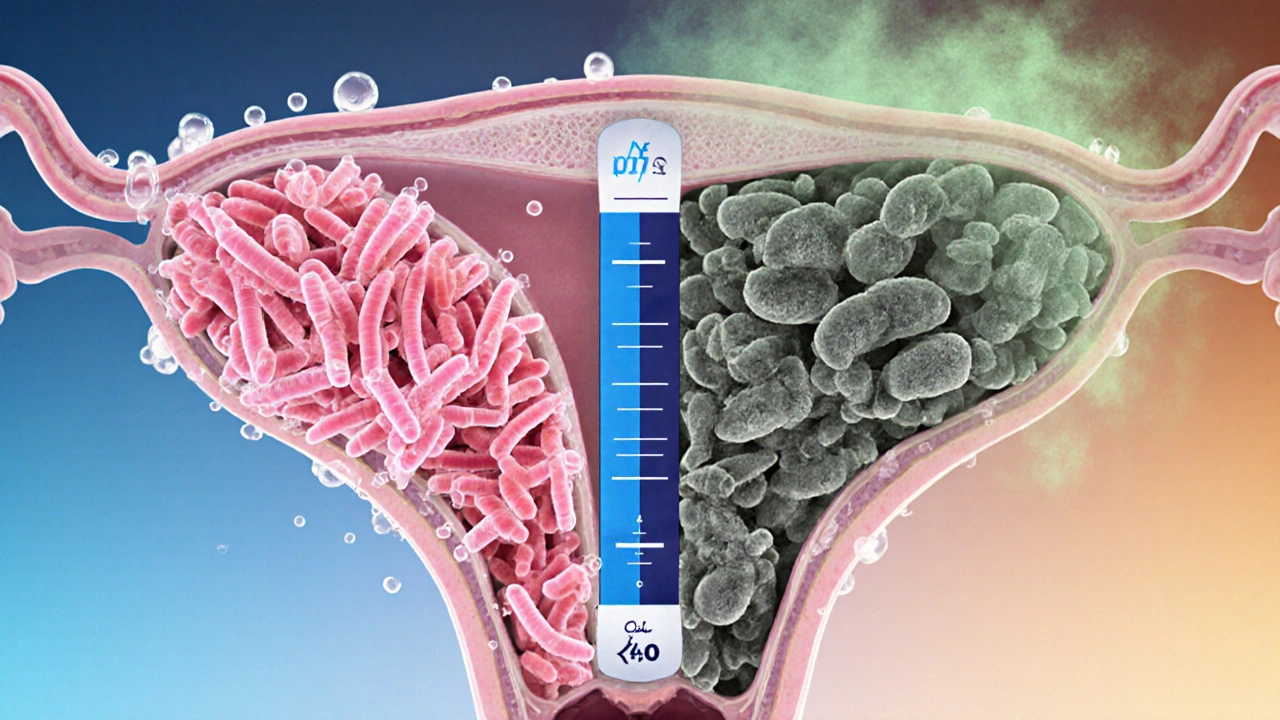
How BV Changes the Vaginal Environment
Under healthy circumstances, the vaginal microbiome is dominated by lactobacilli that maintain an acidic pH (around 3.8‑4.5). These good bacteria produce lactic acid, keeping the environment hostile to harmful microbes.
When BV takes hold, the balance tips. Lactobacilli drop dramatically, allowing overgrowth of Gardnerella, Mobiluncus, and other anaerobes. This shift raises the pH level to above 4.5, which makes the vagina less acidic and more hospitable to pathogenic bacteria. The result is a distinctive fishy odor and a thin, grayish discharge.
Symptoms That Can Disrupt Intimacy
Even mild BV can feel like a relationship spoiler:
- Odor: A strong, fishy smell becomes noticeable after sex or during menstruation.
- Discharge: Thin, gray‑white fluid that may coat the vulva.
- Irritation: Mild itching or burning, especially during intercourse.
- Feeling of “wetness”: Unwanted lubrication can lead to self‑consciousness.
These cues often spark embarrassment. Many women report hesitating to initiate sex or feeling the need to “air out” before getting intimate. The mental load adds a layer of anxiety that can diminish desire even before the physical symptoms appear.
The Direct Impact on Sexual Activity
Sexual intimacy isn't just a physical act; it’s a dance of confidence and connection. When BV shows up, the dance can stumble:
- Reduced Libido: Fear of odor or discharge can make the idea of getting close unappealing.
- Physical Discomfort: Irritation can turn pleasurable friction into pain, especially with condom use.
- Communication Breakdowns: Partners may misinterpret avoidance as rejection, leading to tension.
Studies from women's health clinics in 2023 found that 42% of those with recurrent BV reported a noticeable dip in sexual satisfaction, compared with only 14% of women without the condition.
Hidden Risks: STIs and Pregnancy
BV itself isn't an STI, but the altered environment makes it easier for sexually transmitted infections to take hold. The higher pH reduces the natural barrier that lactobacilli provide, increasing susceptibility to chlamydia, gonorrhea, and even HIV.
Pregnant women with untreated BV face a higher chance of preterm birth, low birth weight, and premature rupture of membranes. The Centers for Disease Control and Prevention (CDC) cites a 1.5‑fold increase in preterm delivery among pregnant patients diagnosed with BV.

Diagnosis and Treatment Options
Diagnosing BV usually involves a quick pelvic exam and a “whiff test” that detects the characteristic odor. Lab analysis may check the Nugent score, a microscopic grading system.
First‑line treatment relies on antibiotics:
- Metronidazole is taken orally (500mg twice daily for 7days) or applied as a gel. It attacks the anaerobic bacteria directly.
- Clindamycin is another option, available as a cream or oral capsule, useful for patients who can’t tolerate metronidazole.
About 20% of women experience recurrence within three months, so many clinicians add a probiotic regimen to restore lactobacilli. Strains like Lactobacillus rhamnosus GR‑1 and Lactobacillus reuteri RC‑14 have shown promise in reducing repeat infections.
Important tip: Complete the full antibiotic course, even if symptoms fade early. Stopping prematurely can allow resistant bacteria to rebound.
Prevention and Partner Considerations
Keeping BV at bay is partly about lifestyle and partly about partnership dynamics:
- Condom Use: Condoms provide a barrier that can reduce bacterial transfer during sex. They’re especially helpful if a partner has a known imbalance.
- Hygiene Practices: Avoid douching, scented soaps, and tight synthetic underwear that trap moisture.
- Probiotic Supplementation: Daily oral probiotics or vaginal suppositories can keep lactobacilli levels steady.
- Partner Testing: While BV isn't an STI, treating a male partner can lower recurrence in some couples, according to a 2022 randomized trial.
Open conversation is the unsung hero. Letting your partner know what you're experiencing removes mystery and lets you both decide on preventive steps together.
Quick Comparison: Bacterial Vaginosis vs. Yeast Infection
| Feature | Bacterial Vaginosis | Yeast Infection |
|---|---|---|
| Cause | Overgrowth of anaerobic bacteria | Overgrowth of Candida fungus |
| Typical pH | >4.5 (more alkaline) | ≈4.0 (acidic) |
| Discharge | Thin, gray‑white, fishy odor | Thick, white, “cheese‑like” |
| Itching | Mild or none | Intense itching, burning |
| Treatment | Metronidazole or clindamycin | Antifungal (e.g., fluconazole) |
Frequently Asked Questions
Can Bacterial Vaginosis be caught from a partner?
BV isn't classified as an STI, but sexual activity can shift vaginal bacteria. Treating both partners may lower recurrence, especially if one has symptoms.
How long does treatment usually take?
A standard oral course of metronidazole lasts 7days. Some women feel better in 2‑3days, but finishing the full regimen is crucial to prevent relapse.
Will I be able to have sex during treatment?
It’s best to avoid intercourse until the antibiotic course is finished and symptoms subside. Condoms can reduce irritation and bacterial spread if you must be intimate.
Are probiotics effective for preventing BV?
Certain lactobacilli strains have shown a 30‑40% reduction in recurrence when taken daily for three months after antibiotics.
Can BV affect pregnancy outcomes?
Yes. Untreated BV is linked to a higher risk of preterm birth and low birth weight. Pregnant women should seek treatment promptly.
Bottom line: Bacterial Vaginosis can dim the glow of intimacy, but it’s a treatable condition. By understanding how it works, catching it early, and communicating openly, you can keep both your health and your love life on track.






Stop ignoring the fact that you need to finish the full antibiotic course.
First off, BV isn’t classified as an STI, but sexual activity can certainly tip the balance of vaginal bacteria. The condition arises when the natural Lactobacillus population is displaced by anaerobic microbes, leading to the characteristic odor and discharge. It’s important to note that the symptoms can vary from barely noticeable to quite disruptive, depending on the individual’s microbiome. Treating the infection promptly with the full antibiotic course cuts down the chance of a relapse, and using condoms during the treatment period can help minimize irritation. If you or your partner notice persistent symptoms, a follow‑up visit is advisable to rule out resistance.
BV is often misunderstood, and the misconceptions start early. Some people think it’s a harmless “smell” that can be ignored, but the reality is far more complex. The bacterial imbalance can cause irritation that makes any sexual activity uncomfortable. It also creates a psychological barrier; many women feel embarrassed and avoid intimacy altogether. The fishy odor, while distinct, is just a symptom of an underlying shift in the vaginal microbiome. Treating the infection with the full course of antibiotics is non‑negotiable, otherwise the bacteria rebound. Partner treatment is not always required, but it can reduce the odds of recurrence when the male partner exhibits symptoms. Probiotics, especially lactobacilli strains, have been shown to lower the chance of a second episode by up to forty percent when taken after antibiotics. Lifestyle factors such as douching, tight clothing, and scented products can perpetuate the imbalance. The immune system also plays a role; stress and hormonal fluctuations can exacerbate symptoms. Many clinicians advise abstaining from intercourse until the treatment is complete and the discharge has cleared, which is typically around a week. Condoms can reduce friction and bacterial spread, but they are not a cure. Open communication with a partner can alleviate anxiety and promote a supportive environment. If BV is left untreated during pregnancy, the risks include preterm birth and low birth weight, which underscores the importance of timely care. Ultimately, understanding the condition removes some of the stigma and empowers women to seek treatment promptly. The more we talk about BV openly, the less it will dominate intimate relationships.
If you’re thinking you can skip the condom just because you’re on meds, think again – irritation will only make things worse.
I felt like my whole love life evaporated the moment the fishy smell showed up – it was heartbreaking and isolating.
Adding a daily probiotic containing Lactobacillus rhamnosus or crispatus after finishing antibiotics can significantly lower the odds of BV coming back. Also, avoid douching and scented hygiene products, as they disrupt the natural pH balance and set the stage for recurrence.
✅ Finish the full prescription – no shortcuts! ✅ Use condoms until symptoms are gone – protect both partners! ✅ Follow up with your doctor if you don’t see improvement in 3 days! 😅
Complete the prescribed regimen before resuming intercourse.
Oh, because ignoring medical advice has always led to perfect outcomes.
The historical perspective on bacterial vaginosis reveals that it has long been a silent undercurrent in women’s health, often eclipsed by more sensationalized sexually transmitted infections. Early gynecological texts described a “nonspecific vaginitis” that aligns closely with today’s definition of BV, yet it remained undervalued in clinical discourse. Modern research, however, has illuminated the intricate ecological dynamics of the vaginal flora, demonstrating that a departure from Lactobacillus dominance can precipitate a cascade of symptoms affecting intimacy. From a sociocultural standpoint, the stigma attached to genital odors has deep roots in patriarchal notions of female purity, which can exacerbate the emotional toll on those experiencing recurrent episodes. When a woman perceives herself as “unclean,” the resulting self‑consciousness may lead to avoidance of sexual encounters, thereby straining relational bonds. Moreover, the recurrence rate of BV-estimated at 30 to 50 percent within six months-places a substantial burden on both partners, who must navigate treatment decisions together. Healthcare providers increasingly recommend a holistic approach that couples antimicrobial therapy with probiotic supplementation to restore a balanced microbiome. In addition, lifestyle modifications such as avoiding intravaginal deodorants, limiting prolonged exposure to moist environments, and adopting breathable underwear contribute to long‑term stability. It is also noteworthy that certain ethnic groups exhibit differing prevalence rates, suggesting a genetic or environmental component that warrants further investigation. Public health initiatives that destigmatize conversation about BV can foster earlier presentation to medical care, reducing the risk of complications such as preterm labor. The interplay between physiological symptoms and psychological well‑being underscores the necessity of a compassionate clinical encounter. By framing BV as a manageable condition rather than an affront to femininity, clinicians can empower patients to maintain a satisfying intimate life. Consequently, the integration of evidence‑based treatment, patient education, and partner involvement represents the optimal pathway to preserving both health and intimacy. As research continues to unravel the microbiological intricacies, we anticipate more targeted therapeutics that will further diminish the impact of BV on personal relationships.
You’re right, finishing the antibiotics is crucial; it eradicates the pathogenic bacteria and gives the good flora a chance to rebound.
I’d also suggest keeping a symptom diary – noting discharge changes, odor intensity, and any itching can help you and your clinician fine‑tune the treatment plan.
👍 Great point about probiotics! 🎉 They really help restore balance after the meds.
From a microbiological standpoint, the dysbiosis characteristic of BV reflects a shift in the obligate anaerobe to facultative anaerobe ratio, which compromises mucosal immunity and predisposes to secondary infections.