When you pick up a prescription for metformin, lisinopril, or ibuprofen, there’s a 90% chance it’s a generic drug. These pills look different from the brand-name versions, cost far less, and yet work just the same. But how exactly are they made? It’s not just copying a pill. It’s a highly regulated, science-heavy process that takes years, millions of dollars, and strict adherence to federal rules. Here’s how generic drugs go from a chemical formula to the bottle on your shelf.
Starting with the Original: Reverse Engineering the Brand-Name Drug
The first step in making a generic drug isn’t mixing chemicals-it’s studying the original. Manufacturers don’t just guess what’s in a brand-name pill. They take the reference listed drug (RLD), the FDA-approved brand-name version, and break it down. This is called reverse engineering. They analyze the active ingredient, the exact amount, and every inactive ingredient-like fillers, binders, and coatings-that help the drug work properly in the body. This isn’t simple chemistry. It’s forensic-level analysis. Scientists use tools like high-performance liquid chromatography (HPLC) and mass spectrometry to identify every component. They test how the drug dissolves in water, how fast it releases into the bloodstream, and how stable it is under heat or humidity. All of this data becomes the blueprint for the generic version. Why does this matter? Because even small differences in inactive ingredients can change how the drug behaves. A change in the particle size of lactose, for example, can make a tablet too hard or too soft, affecting how quickly the medicine is absorbed. One pharmacist on Reddit with over a decade of experience said, “The biggest headache in generic manufacturing is excipient variability.” A supplier switch can derail months of work.Designing the Formula: Quality by Design (QbD)
Once they understand the original, manufacturers move to formulation. This isn’t trial and error. It follows the Quality by Design (QbD) framework, a global standard set by the International Council for Harmonisation (ICH). QbD means building quality into the drug from the start, not testing it in at the end. They identify three key factors:- Critical Quality Attributes (CQAs): What must the drug do? For example, it must release 85% of its active ingredient within 30 minutes.
- Critical Material Attributes (CMAs): What properties must the raw materials have? Like the flow rate of the powder or the moisture content of the starch.
- Critical Process Parameters (CPPs): What steps in manufacturing must be tightly controlled? Temperature, mixing time, compression pressure-all of these are measured and logged.
The Seven-Step Manufacturing Process
Now comes the actual production. Here’s how a generic tablet is made, step by step:- Formulation: The active pharmaceutical ingredient (API) is mixed with excipients-fillers, binders, disintegrants, lubricants. This blend is carefully weighed and mixed to ensure uniform distribution. Even a 0.1% error can affect performance.
- Mixing and Granulation: The powder blend is turned into granules. This improves flow during compression and prevents separation. Wet granulation adds a liquid binder; dry granulation uses pressure. The method chosen depends on the drug’s sensitivity to heat or moisture.
- Drying: If wet granulation was used, the granules are dried in trays or fluid-bed dryers. Moisture must be reduced to under 2% to prevent degradation during storage.
- Compression and Encapsulation: Dry granules are pressed into tablets using high-speed tablet presses. Capsules are filled with powder or pellets using automated machines. Each machine is calibrated to hit exact weight targets. For tablets under 130mg, weight variation can’t exceed ±5%. For larger ones, it’s ±7.5%.
- Coating: Tablets are coated to mask bitter tastes, protect the drug from stomach acid, or control release. A delayed-release coating might keep the drug from dissolving until it reaches the intestine. Coating thickness is monitored with laser sensors.
- Quality Control: This isn’t one test at the end-it’s built into every stage. Samples are pulled for testing: potency, dissolution rate, purity, microbial contamination, and uniformity. Dissolution testing is especially critical. The generic must release the drug at the same rate as the brand-name version, within the 80%-125% range.
- Packaging and Labeling: Tablets are sealed in blister packs or bottles with child-resistant caps. Labels must match the brand-name drug’s information exactly-dosage, warnings, usage-but can’t copy the brand’s logo or color scheme. U.S. trademark law prevents generics from looking identical to the original.

Facilities Must Meet Strict Standards
You can’t make generic drugs in a garage. Every facility must follow Current Good Manufacturing Practices (CGMP), enforced by the FDA. These rules cover everything from air quality to employee hygiene. Manufacturing areas are cleanrooms, classified by particle count:- ISO Class 5: For sterile filling (like injectables)-like a hospital operating room.
- ISO Class 7-8: For tablet production-cleaner than a typical lab.
The Approval Pathway: The ANDA Process
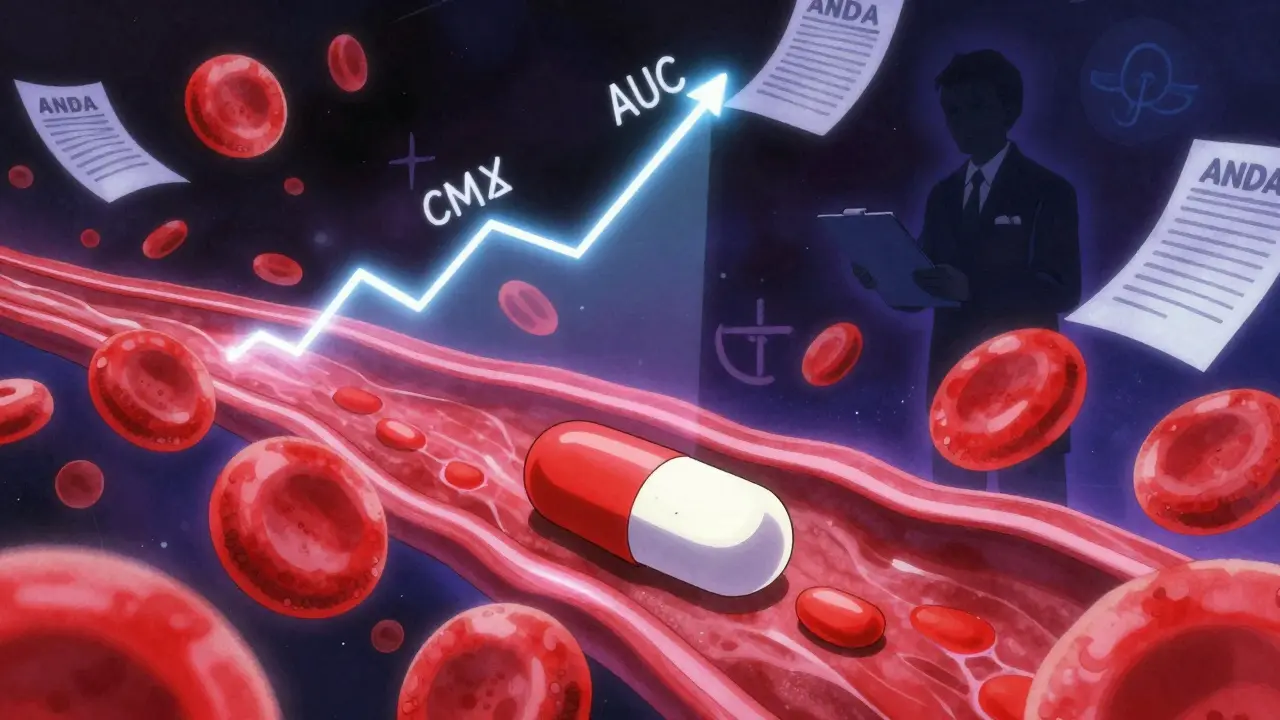
Making the drug is only half the battle. To sell it, manufacturers must get FDA approval through an Abbreviated New Drug Application (ANDA). Unlike brand-name drugs, which require 10-15 years and over $2 billion in clinical trials, generics use a shortcut. The ANDA doesn’t repeat safety and efficacy studies. Instead, it proves the generic is bioequivalent to the brand-name drug. That means:- It delivers the same amount of active ingredient into the bloodstream.
- It does so at the same speed.
- Cmax: The highest concentration in the blood.
- AUC: The total exposure over time.




People think generics are just knockoffs but nah it's way more science than you think
They reverse engineer like detectives with HPLC machines and lab coats
You think it's just chemistry but it's forensic pharmaco-forensics
One wrong particle size and your blood pressure med turns into a paperweight
And don't even get me started on excipients
Pharmacies switch suppliers all the time and boom entire batches get tossed
This isn't Walmart knockoff stuff this is precision medicine at scale
It's fascinating how much rigor goes into something so seemingly simple-each tablet is essentially a miniature engineering marvel.
From the moisture content of the starch, to the exact compression pressure, to the laser-monitored coating thickness-every variable is controlled with near-obsessive precision.
And yet, the public often assumes it's just 'the same drug, cheaper.'
It's not just bioequivalence-it's bioconsistency, batch after batch, year after year.
Pharmacists know this better than anyone, and yet, the stigma persists.
Thank you for highlighting the QbD framework-it's the unsung hero of modern pharma.
Wait so if a generic has to match the brand-name drug's dissolution rate within 80-125% that means technically one could be 25% slower to kick in?
Like if I take a generic lisinopril, could it take longer to lower my BP than the brand?
And if so, why do doctors still say they're 'the same'?
Also-how do they even test this? Do people swallow pills and then get poked with needles every 15 minutes for hours??
Also also-what happens if someone has a bad reaction to one generic but not another??
Also also also-why do they look so different??
So many people think medicine is magic
But it's just molecules and math
They don't know how hard it is to copy a pill
It's not like baking a cake where you swap sugar for honey
One wrong powder and your body doesn't absorb it
And the factories? Clean rooms like space labs
Workers look like astronauts
And the FDA? They check everything
Even if you drop one tablet, the whole batch is trash
That's why generics are cheap but not easy
It's science with soul
I love how this post breaks it down without jargon overload
Also-can we talk about how insane it is that a $84k hepatitis C drug dropped to $28k just because generics came in?
That’s not just savings-that’s life or death
And yet, some people still think generics are ‘inferior’
My grandma takes three generics and she’s doing better than most people her age with brand-name meds
It’s not magic, it’s math-and it’s saving millions
Let’s stop stigmatizing affordability
Also-can we make a meme about this??
Oh so now we're glorifying Big Pharma's knockoff factory workers like they're saints?
Let me guess-next you'll say the FDA is a benevolent guardian
Wake up
Most generics are made in India and China where labor is cheap and inspections are bribes
And don't even get me started on the 2021 Teva recall-14 drugs pulled because they didn't even test their own pills properly
And you think this is 'science'? No-it's profit with a lab coat
And you people act like it's a miracle when a pill works
It's not a miracle-it's a gamble
And someone's kid is paying for it with their liver
So the coating thickness is monitored with lasers
And the tablet weight has to be within 5% for small ones
And the air in the room has to be filtered like a hospital
But the pill looks different from the brand so it's not the same
Wait what
Why does it matter what it looks like if it works the same
And why do we even care what color it is
Also why do we call them generics if they're all different from each other
Also why do some people say they feel different on one vs another
Is that placebo or real
Also why can't we just make them all look the same
Also also also
OMG I didn’t know this was so complex 😱🤯
So a pill is basically a tiny science experiment with a label??
And they use lasers to check coatings??
And the FDA checks every single batch??
I thought generics were just cheaper versions of the same thing
But now I feel like I’m watching a Netflix documentary on pharmaceutical espionage 🕵️♀️💊
Also-can we make a TikTok about this??
Someone needs to film a factory tour with chill lofi beats and this info overlaid 🎧
Let's be real-this whole 'generic drug' narrative is corporate PR
You think this is about patient access?
No-it's about patent cliffs and market monopolies
The FDA approval process is a rubber stamp for companies that outsource to the cheapest lab in Hyderabad
And the bioequivalence range? 80-125%? That's not science-that's a loophole
People die from inconsistent absorption in narrow-therapeutic-index drugs
And you call this 'affordable medicine'?
No-you call it risk redistribution
And you're celebrating it like it's a win
It's not a win-it's a compromise
And someone's kidney is paying the price