When it comes to senior medication safety, the practice of ensuring older adults use drugs correctly without harmful side effects or interactions. Also known as elderly drug safety, it’s not just about taking pills on time—it’s about understanding how your body changes after 65 and why the same dose that worked at 40 can turn dangerous at 75. About 40% of seniors take five or more prescription drugs daily, a situation called polypharmacy, the use of multiple medications simultaneously, often leading to unintended interactions. This isn’t rare—it’s normal. But it’s also where things go wrong. A simple painkiller mixed with a blood pressure med can drop your blood pressure too low. A sleep aid combined with an antidepressant might cause confusion or falls. These aren’t hypothetical risks. They’re daily realities in ERs across the country.
Many seniors don’t realize their pharmacist isn’t always told about every supplement or over-the-counter drug they’re using. Things like melatonin, ginkgo, or even high-dose vitamin E can interfere with warfarin, statins, or diabetes meds. The FDA drug guidelines, official recommendations for safe prescribing and monitoring of medications in older populations. These aren’t just suggestions—they’re based on real-world data from thousands of elderly patients who suffered avoidable harm. The FDA now pushes for clearer labeling, mandatory reviews of drug combinations in seniors, and better communication between doctors, pharmacists, and patients. But you still have to be the one asking the questions: "Is this still necessary?", "Could this be causing my dizziness?", "What happens if I skip this one?"
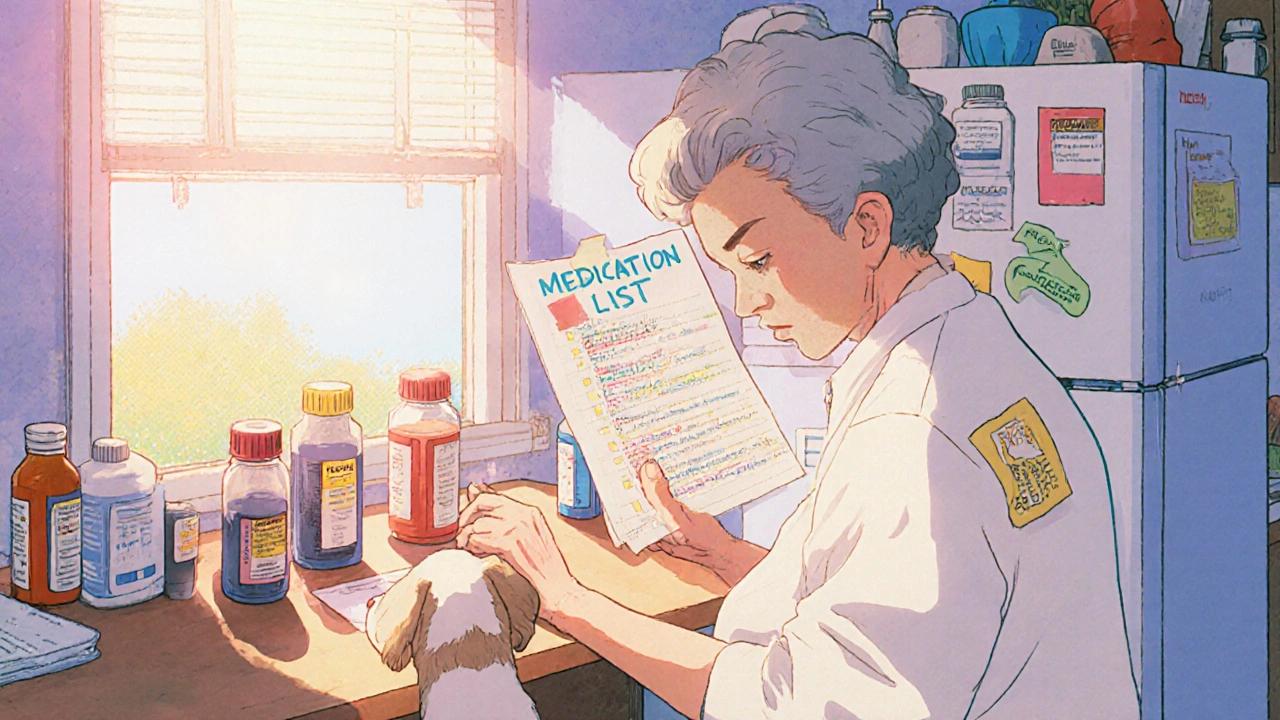
Five practical, evidence-based medication safety tips for seniors and caregivers to prevent dangerous drug interactions, missed doses, and hospitalizations. Backed by the FDA and geriatric experts.
