Managing multiple medications isn’t just about remembering to take them-it’s about taking them at the right time, in the right order, and without clashing with each other. If you’re on five or more prescriptions, supplements, or over-the-counter drugs, you’re not alone. Nearly 40% of adults over 65 are in this boat, and for many, the risk of dangerous drug interactions is real. One wrong timing choice-like taking calcium with thyroid medicine-can cancel out the effect of one drug or spike your risk of bleeding, dizziness, or organ damage. But a well-built medication schedule can cut those risks dramatically.
Start with a Complete Medication List
Before you even think about timing, you need to know exactly what you’re taking. This isn’t just your prescriptions. It includes every supplement, herbal remedy, painkiller from the pharmacy, and even antacids you grab off the shelf. Many people forget these, but they’re often the culprits behind interactions. For example, St. John’s Wort can make blood thinners like warfarin useless, and calcium supplements can block absorption of thyroid meds. Write everything down: name, dose, why you take it, and how often. Do this in front of your medicine cabinet, not from memory. Bring this list to every doctor and pharmacist visit. Studies show that when patients bring all their meds in a brown bag to appointments, pharmacists find an average of 3.2 errors per person-things like duplicate drugs, wrong doses, or hidden interactions. Verbal lists miss nearly half of these.Use the Universal Medication Schedule (UMS)
Forget vague instructions like “take twice daily” or “with meals.” These are confusing, especially for older adults or those with low health literacy. The Universal Medication Schedule (UMS), backed by the Agency for Healthcare Research and Quality and adopted by major EHR systems like Epic, uses four clear time blocks:- Morning: 6-10 AM
- Noon: 10 AM-2 PM
- Evening: 2-6 PM
- Bedtime: 8 PM-12 AM
Group Medications by Time, Not by Pill
Don’t organize your schedule by pill bottle. Group by time of day. This is where most people get stuck. Instead of thinking, “I have to take six pills at 8 AM,” think: “What goes in the morning slot?” Start by identifying medications with strict timing needs:- Thyroid meds (like levothyroxine) must be taken on an empty stomach, at least 30-60 minutes before food or coffee.
- Statins (like atorvastatin) work best taken at night, when your liver makes the most cholesterol.
- Antibiotics like amoxicillin often need exact 8-hour spacing to stay effective.
- Calcium and iron supplements should be taken 2 hours apart from thyroid meds or antibiotics-they block absorption.
- NSAIDs like ibuprofen should never be mixed with blood thinners without a doctor’s okay-they raise bleeding risk by 60-70%.
- Morning (6-10 AM): Levothyroxine (on empty stomach), then 1 hour later: multivitamin, blood pressure pill
- Noon (10 AM-2 PM): Statin (if prescribed for daytime), aspirin, vitamin D
- Evening (2-6 PM): Diuretic (to avoid nighttime bathroom trips), calcium (if needed)
- Bedtime (8 PM-12 AM): Sleep aid, gabapentin, second dose of antibiotic if required
Use a Pill Organizer and Calendar
A simple 7-day pill box with AM/PM compartments cuts dosing errors by 45%, according to a major meta-analysis in the Annals of Internal Medicine. Choose one with labeled compartments-some even have alarms built in. Don’t just fill it once a week. If you take meds that need exact timing (like antibiotics), use a daily organizer or a digital tracker. Pair it with a written calendar. Tape it to your fridge or bathroom mirror. Mark each dose with a checkmark or X. Include notes like “take 1 hour before breakfast” or “avoid dairy.” This visual cue is what 72% of successful users rely on. Apps like Medisafe or MyTherapy can help, but only 38% of people over 65 use them consistently. Paper still wins for reliability.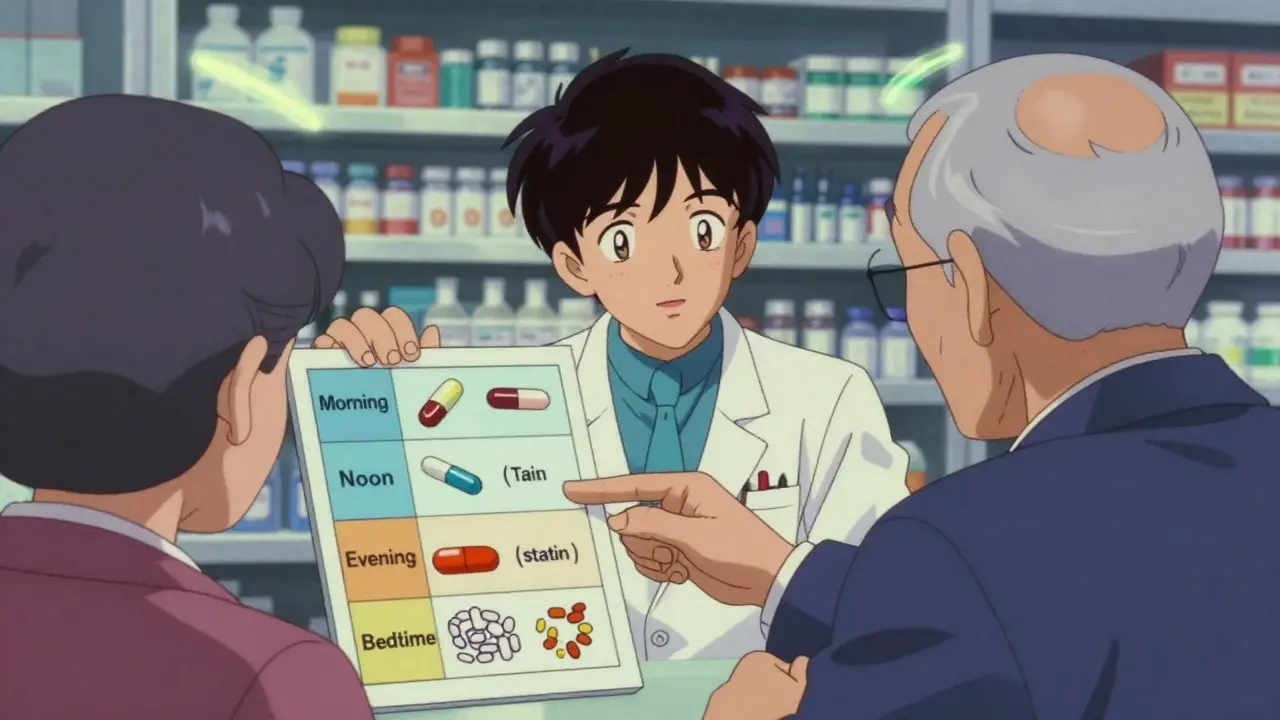
Synchronize Refills to Reduce Chaos
Having 10 different refill dates is a recipe for missed doses and last-minute pharmacy runs. The AMA’s STEPS Forward program recommends the “90 x 4” approach: get 90-day supplies and refill them four times a year-on the same day. This means one trip to the pharmacy every three months instead of 10. It saves clinicians up to two hours per day managing refills, and it cuts your stress by 80%. Ask your pharmacist to sync all your prescriptions. Most pharmacies offer this for free. If your doctor resists, say: “I want to reduce my risk of missing doses and interactions-can we switch to 90-day fills?” Many now support this under Medicare and private insurance.Know the High-Risk Combinations
The American Geriatrics Society’s Beers Criteria (updated 2023) lists 30 dangerous combinations to avoid, especially for older adults. Here are the big ones:- Blood thinners + NSAIDs: Warfarin, apixaban, or rivaroxaban with ibuprofen or naproxen = high bleeding risk.
- SSRIs + NSAIDs: Prozac or Zoloft with aspirin or Advil = increased bruising and stomach bleeding.
- Statins + grapefruit juice: Even one glass can spike drug levels and damage muscles.
- Antibiotics + dairy: Tetracycline or ciprofloxacin with milk or yogurt = reduced absorption.
- Diuretics + potassium supplements: Can cause dangerous heart rhythms if you’re also on ACE inhibitors.
Watch for Warning Signs
Even the best schedule can’t catch every interaction. Know what to watch for:- Sudden dizziness or lightheadedness
- Unusual bruising or bleeding (nosebleeds, bloody stools)
- Severe stomach pain or nausea
- Confusion, memory lapses, or slurred speech
- Swelling in hands or feet

Work With Your Pharmacist, Not Just Your Doctor
Doctors are great at prescribing, but pharmacists are the experts in how drugs interact. They see your full list, know your history, and can spot problems your doctor might miss. Ask for a free medication therapy review. Many pharmacies offer this. Bring your brown bag of meds. Ask:- “Are any of these interacting?”
- “Can any of these be combined into one pill?”
- “Is there a safer alternative for this one?”
Keep It Simple, Keep It Visible
The most effective schedules aren’t the most complex-they’re the ones you can follow without thinking. Reduce the number of pills where possible. Ask if combination pills exist (like a blood pressure pill that includes a diuretic). Cut supplements you don’t need. Many people take vitamins they don’t need because they “might help.” But more isn’t better-it’s riskier. Place your pill organizer, calendar, and meds where you’ll see them daily: next to your toothbrush, coffee maker, or breakfast table. Set phone alarms labeled clearly: “Levothyroxine - empty stomach.” Don’t rely on memory. Use the tools that work for you.What If You’re Still Confused?
If your schedule feels overwhelming, you’re not failing-you’re in the majority. Nearly 42% of adults over 65 report confusion with timing. That’s not your fault. It’s the system’s. Ask for help. Call your pharmacist. Ask your primary care provider for a referral to a medication therapy management program. Many insurance plans cover it. Use free resources like the AHRQ’s Medication Safety Toolkit. You don’t have to figure this out alone.Final Thought: This Is About Safety, Not Just Compliance
A medication schedule isn’t just about remembering to take your pills. It’s about making sure they work-without hurting you. Every time you space out calcium from thyroid meds, avoid grapefruit with your statin, or sync your refills, you’re lowering your risk of a hospital visit, a fall, or worse. It’s not about being perfect. It’s about being smart. Start with one change today: write down every pill you take. Bring it to your next appointment. That’s the first step to a safer, simpler routine.How do I know if my medications are interacting?
Watch for sudden symptoms like dizziness, unusual bruising, stomach pain, confusion, or swelling. These can signal a dangerous interaction. If you notice any after starting or changing a medication, contact your pharmacist or doctor right away. You can also use free online interaction checkers like Medscape’s Drug Interaction Checker or ask your pharmacist to run a scan using Lexicomp.
Can I use a smartphone app instead of a pill organizer?
Apps like Medisafe or MyTherapy can help with reminders and tracking, and they improve adherence by 20-35%. But they’re not foolproof-only 38% of people over 65 use them consistently. For reliability, pair an app with a physical pill organizer. Use the app for alerts, and the organizer as your backup. Paper calendars are still the most trusted tool for older adults.
Why do some medications need to be taken on an empty stomach?
Food can block absorption. For example, levothyroxine (for thyroid) binds to calcium, iron, or even coffee, making it less effective. Antibiotics like ciprofloxacin are absorbed poorly with dairy. Taking these on an empty stomach-30-60 minutes before eating-ensures your body gets the full dose. Always check the label or ask your pharmacist for specifics.
What’s the safest way to store my medications?
Keep them in a cool, dry place away from sunlight and moisture-bathrooms and kitchens are bad choices. Use a locked box if you have kids or visitors. Don’t mix pills in unlabeled containers. Store them near your daily routine spots (bathroom, kitchen) so you remember them. Avoid keeping expired meds-they can degrade and become unsafe.
How often should I update my medication list?
Update it every time you see a doctor, pharmacist, or start/stop a medication-even if it’s just an OTC painkiller. Keep a printed copy in your wallet and a digital version on your phone. Many hospitals and clinics now ask for it during check-in. Having an up-to-date list can prevent dangerous mistakes during emergencies.
Can I combine multiple pills into one dose?
Sometimes, yes-but never without checking with your doctor or pharmacist. Some drugs can be safely combined into one pill (like blood pressure combos), but others must be spaced apart. For example, you can’t crush a time-release pill or mix antibiotics with calcium. Always ask: “Is there a combination pill available for these?” It can reduce your daily count and lower interaction risk.







Just started using a pill organizer last month. Huge difference. No more wondering if I took my blood pressure pill or not. Also stopped taking that random calcium supplement I was told to take ‘just in case’ - turns out it was messing with my thyroid med. Simple fix, big win.
You know, this whole system reminds me of how we used to organize chaos in pre-digital times - calendars on the fridge, handwritten notes, the whole ritual. There’s something deeply human about physically checking off a box, isn’t there? It’s not just compliance, it’s a form of self-care that demands presence. We’ve outsourced so much to apps and algorithms, but when your life depends on timing, maybe analog is the only real safety net. The brain remembers action, not alerts. And when you’re 72, and your memory’s playing tricks, that checkmark is your anchor. I’ve seen too many people rely on their phone, only to have it die, or forget to turn on notifications, or worse - get confused by the app’s interface. Paper doesn’t update itself, but it doesn’t vanish either. It’s there. Always. And that’s the quiet kind of reliability we all need when our bodies are fighting so hard to stay balanced.
This is GOLD!! 🙌 I just shared this with my mom and she’s already syncing her refills! She used to have 11 different pickup days - now it’s ONE. She’s crying happy tears 😭 Thank you for writing this like a human who actually gets it. My pharmacist even said this is the best advice she’s heard in months!! 💪
UMS is a band-aid solution for a systemic failure in pharmacoeconomic design. The real issue is polypharmacy driven by fee-for-service incentives, not patient education. The 34% misinterpretation rate? That’s not a literacy problem - it’s a failure of clinical decision support integration. You’re treating symptoms, not root causes. A properly configured CDS system with AI-driven interaction alerts embedded in EHRs would render UMS obsolete. But then again, who wants to pay for real innovation when a laminated chart costs $0.50?
Interesting how this post assumes everyone lives in the U.S. and has a pharmacist who gives a damn. In my town, the pharmacy is a Walmart with a guy behind the counter who’s never heard of Lexicomp. And don’t get me started on ‘90-day fills’ - try getting that approved when you’re on Medicaid and your doctor’s office won’t call in the request until the 27th of the month. This feels like advice from someone who’s never had to fight the system just to get their meds.
Let’s be precise: the UMS is a heuristic, not a protocol. It’s statistically significant in reducing ambiguity, yes - but it lacks granularity for circadian pharmacokinetics. For instance, levothyroxine’s half-life is 7 days, yet absorption is time-dependent on gastric pH, which fluctuates with circadian cortisol peaks. Therefore, 6–10 AM is a proxy, not a precision. Furthermore, statins’ efficacy correlates with HMG-CoA reductase activity, which peaks at 2 AM - so a 10 PM dose is more optimal than 8 PM. The ‘bedtime’ block is too broad. And where’s the data on food matrix effects on calcium absorption? You mention dairy, but what about fiber? Oxalates? Phytates? The article is well-intentioned, but it’s a superficial gloss on a complex pharmacodynamic landscape.
Great breakdown! I work as a pharmacist in India and see this daily - people mixing antibiotics with milk, taking painkillers with blood pressure meds, forgetting supplements. The UMS system works even here. We’ve started printing simple color-coded charts for elderly patients: green for morning, blue for noon, etc. No reading needed. Also, always ask: ‘Is this pill really necessary?’ So many take vitamins just because their friend does. Less is more. And yes - paper calendars still win. Phones die. Memory fades. But a sticky note on the mirror? That stays.
Wow. Another feel-good article from someone who’s never had to manage 12 meds while on Medicare Part D with a $500 deductible. You think a pill organizer fixes the fact that half your prescriptions cost more than your rent? Or that your ‘pharmacist’ is a guy who can’t pronounce your drug names? This is content designed for people with time, money, and access - not the 60% of seniors who skip doses because they can’t afford them. Congratulations on turning a structural crisis into a productivity hack.
THIS. This is the kind of post that saves lives. I’m a nurse and I’ve watched too many patients end up in the ER because they mixed ibuprofen with warfarin. Please - if you’re reading this, do one thing today: write down every single thing you take. Even that gummy vitamin. Even that antacid you take after pizza. Bring it to your next appointment. Don’t be shy. Your life is worth that piece of paper. You’re not being a burden - you’re being smart.
Simple and smart. I gave this to my uncle in Punjab - he’s 78, takes 6 meds, no smartphone. Printed it out, drew boxes with pen, stuck it on his wall. He says now he doesn’t forget. No apps. No confusion. Just pen and paper. Sometimes the oldest ways are the best.
lol i just realized i’ve been taking my thyroid med with coffee for 3 years 😅 thanks for this. i thought it was just me being tired all the time. also i had no idea grapefruit was a drug villain. now i’m paranoid about every fruit. also why is my pharmacist so nice? i think he likes me. maybe i should bring him cookies next time.
You got this. Seriously. One step at a time. Write down your meds. Talk to your pharmacist. Don’t wait for a crisis. You’re not alone - thousands of people are doing this right now, and you can be one of them. Start today. You’re stronger than you think. 💪❤️
While your recommendations are superficially commendable, they reflect a troubling capitulation to the commodification of healthcare. The notion that a laminated chart or a pill organizer constitutes a viable solution to systemic pharmaceutical mismanagement is not merely naive - it is ethically irresponsible. True patient safety requires regulatory overhaul, not behavioral band-aids. I urge you to consider the broader sociopolitical context before offering such reductive guidance to vulnerable populations.