Customized medications aren’t just a niche service-they’re life-saving for thousands of patients who can’t take standard pills. Maybe it’s a child who needs a dye-free, sugar-free liquid version of a heart medication. Or an elderly patient who can’t swallow tablets and needs a transdermal gel. Or someone allergic to lactose, gluten, or artificial colors. Compounding pharmacies make these options possible. But with great personalization comes great risk. A single mistake in measurement, labeling, or mixing can lead to overdose, toxicity, or worse. In 2022, the FDA reported 27 cases of fatal fentanyl overdoses linked to mislabeled compounded prescriptions. That’s not a statistic-it’s someone’s parent, sibling, or child. Preventing these errors isn’t optional. It’s the core of responsible compounding.
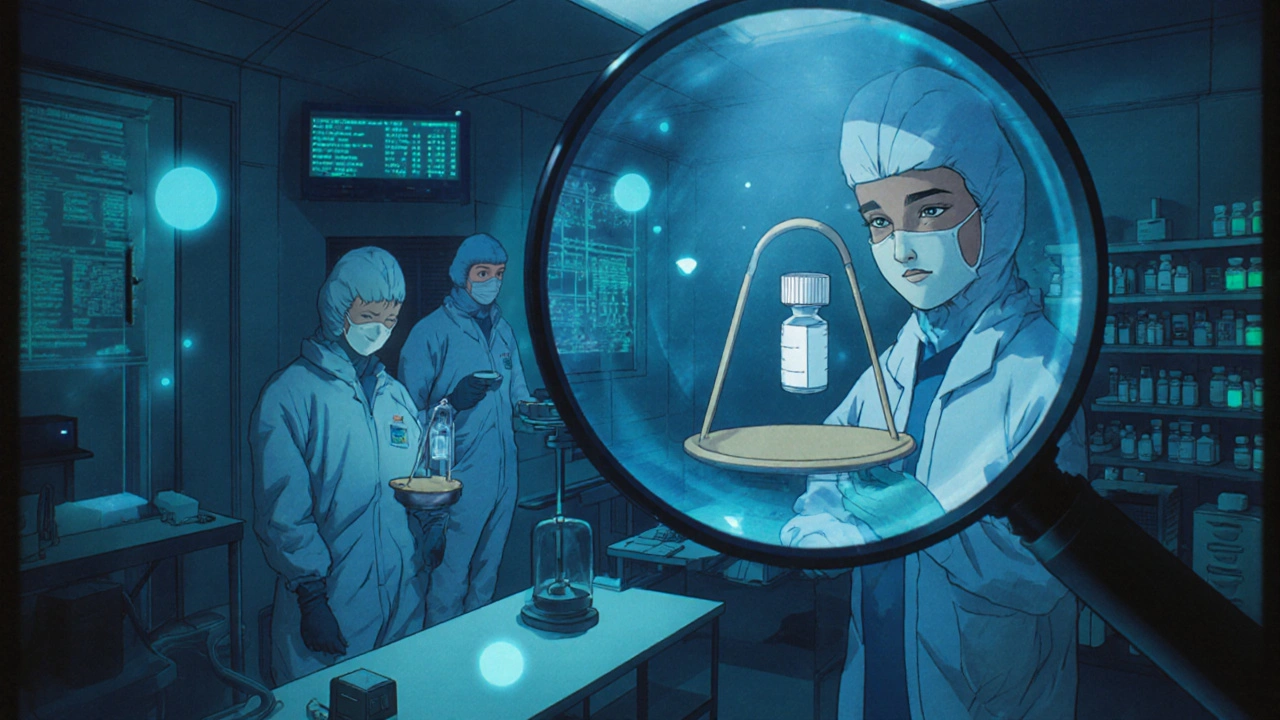
Start with the Right Environment
You can’t make sterile compounds in a cluttered kitchen. The air quality where you mix medications matters. For sterile preparations-like IV bags, injections, or eye drops-USP <797> demands an ISO Class 5 cleanroom. That means filtered air, no dust, no skin flakes, no coughs or sneezes nearby. Non-sterile mixes-like oral suspensions or topical creams-need at least ISO Class 8 air quality per USP <795>. That’s not a suggestion. It’s a legal standard in most states. Facilities that skip this step are gambling with lives. A 2023 study found that pharmacies with poor environmental controls had 3.5 times more contamination-related errors than accredited ones. If your pharmacy doesn’t have air monitors, HEPA filters, and regular surface swab tests, you’re not just cutting corners-you’re putting patients at risk.Double-Check Every Ingredient
One of the most common errors? Grabbing the wrong powder. Imagine thinking you’re weighing out 10 mg of levothyroxine, but you accidentally grab the 100 mg version. That’s a tenfold overdose. The fix? Two independent checks. The pharmacist pulls the ingredient. A second licensed pharmacist or trained technician pulls it again. They compare the label, the lot number, the expiration date, and the physical appearance. Some pharmacies use barcode scanners linked to the formula. One scan confirms the right ingredient. A second scan confirms the right amount. At the University of Tennessee Health Science Center, this system cut ingredient errors by 92% in six months. Don’t rely on memory. Don’t trust your eyes alone. Even experienced pharmacists make mistakes under pressure. That’s why dual verification isn’t just best practice-it’s the baseline.Verify Calculations Like Your Life Depends on It
Compounding often means converting a standard dose into a custom one. A 50 mg tablet becomes 2.5 mg per mL in a liquid. That’s a 1:20 dilution. One decimal point wrong, and you’ve created a deadly concentration. The American Society of Health-System Pharmacists (ASHP) says every calculation must be checked by a second person. Not just glanced at. Not just nodded at. Written down, recalculated, and signed off. Software helps-tools like Compounding.io and PharmScript flag impossible doses or unit mismatches. But software can’t replace human judgment. A 2022 study in the Journal of the American Pharmacists Association found that pharmacies using automated verification tools reduced calculation errors by 40%. But the real win? When those tools are paired with a second human check. That combo brought error rates below 1% in accredited facilities. If your pharmacy skips this step, you’re not saving time-you’re betting on luck.
Labeling That Can’t Be Misread
In 2021, a geriatric patient in Ohio was admitted to the ICU after taking a compounded tramadol solution. The label said “100 mg per container.” But the patient’s caregiver assumed it was “100 mg per mL.” That’s like reading “100 mg per bottle” on a cough syrup and giving a full bottle every hour. The patient got 20 times the intended dose. The FDA has been pushing for standardized labeling since 2023: always use “mg/mL,” never “per container” or “per dose.” Include the total volume. Include the total amount of active ingredient. Include the beyond-use date. And never, ever use abbreviations like “U” for units or “mcg” without spelling out “micrograms.” The Joint Commission found that poor labeling was a root cause in 18% of all serious medication errors between 2019 and 2022. A clear label isn’t nice to have-it’s the last line of defense.Train Like Your Patients’ Lives Are on the Line
Skills in compounding aren’t learned in one weekend seminar. They’re built over months. The Pharmacy Compounding Accreditation Board (PCAB) requires 40+ hours of initial training and 8-12 hours annually. That includes hands-on practice with balances, pipettes, and laminar flow hoods. It includes mock errors-like giving a pharmacist the wrong ingredient and watching how they respond. Quarterly competency assessments are mandatory. Dr. Henry Cohen, former president of the International Academy of Compounding Pharmacists, says this is the single most effective way to reduce errors. A 2022 survey of 300 compounding pharmacists found that those working in accredited facilities were 60% less likely to make a critical error than those in non-accredited ones. Training isn’t paperwork. It’s muscle memory. It’s habit. It’s what keeps a busy pharmacy from turning into a danger zone.
Use Technology-But Don’t Trust It Blindly
AI-powered tools like CompoundingGuard AI are changing the game. In a pilot study across 15 pharmacies, the system flagged 87% of calculation errors before they reached the patient. It cross-references formulas, checks unit conversions, and alerts staff when a dose falls outside safe parameters. But here’s the catch: AI can’t replace human oversight. One pharmacy in Texas relied entirely on their software and missed a mislabeled ingredient because the barcode was smudged. The AI didn’t catch it. The human did. The best systems combine automation with human verification. Use software to catch the obvious mistakes. Use people to catch the subtle ones. And always keep paper backups. Power outages happen. Systems glitch. If you don’t have a manual backup, you’re not prepared.Accreditation Isn’t a Badge-It’s a Lifeline
PCAB accreditation costs $15,000 to $25,000 and takes over a year. It’s not easy. But it’s worth it. Accredited pharmacies have 22% fewer errors than non-accredited ones, according to the National Association of Boards of Pharmacy. They follow strict documentation rules: every batch has a record of ingredients, lot numbers, equipment used, environmental conditions, and dual verification signatures. These records are kept for at least one year past the product’s beyond-use date. Accredited pharmacies also do regular media fill tests-simulating sterile compounding with growth media to catch contamination risks. They test their air quality weekly. They train staff every quarter. They don’t just say they’re safe-they prove it. If your pharmacy isn’t accredited, ask why. And if you’re a patient, ask if your pharmacy is. It’s not about prestige. It’s about survival.What Happens When You Skip These Steps?
In 2012, the New England Compounding Center contaminated steroid injections with fungus. Over 60 people died. 14,000 were exposed. That wasn’t a fluke. It was the result of years of skipped checks, poor training, and ignored regulations. Since then, the industry has changed. But not everywhere. A 2022 study in JAMA Internal Medicine found that error rates in non-accredited compounding pharmacies ranged from 2% to 25%. That’s a 12-fold difference. The difference between safety and catastrophe. You can’t afford to be in the 25% group. If you’re a pharmacist, you owe it to your patients to do better. If you’re a patient or caregiver, ask questions. Ask for accreditation. Ask for dual verification. Ask for clear labeling. Don’t assume it’s done right. Make sure it is.What are the most common errors in compounded medications?
The top errors include incorrect dosing due to miscalculations, wrong ingredients being used (like grabbing 100 mg instead of 10 mg), improper labeling (especially using ambiguous terms like "per container"), contamination from poor air quality, and failure to verify calculations with a second person. Studies show these account for over 80% of serious compounding errors.
How do I know if my pharmacy is safe for compounding?
Ask if they’re accredited by the Pharmacy Compounding Accreditation Board (PCAB). Check if they use dual verification for all calculations and ingredients. Ask if they have a cleanroom with air monitoring and if they perform regular environmental testing. Look for clear labeling with concentration in mg/mL. If they can’t answer these questions confidently, find another pharmacy.
Are compounded medications FDA-approved?
No. Unlike mass-produced drugs, compounded medications don’t go through FDA clinical trials. They’re made for individual patients under specific exemptions. That’s why the safety of the pharmacy matters more than ever. The FDA only steps in when there’s a clear pattern of harm, like the 2012 outbreak. You’re trusting the pharmacy to do the safety work the FDA doesn’t do for them.
Why is dual verification so important?
Human error is unavoidable. Even the most experienced pharmacist can misread a label, miscalculate a decimal, or grab the wrong bottle under stress. Dual verification means two trained professionals independently confirm every step. This simple practice cuts errors by 50-70%, according to ASHP and USP studies. It’s not about distrust-it’s about design. Systems that assume humans are perfect are the ones that fail.
Can I trust a compounding pharmacy that’s not accredited?
Some are fine, but you can’t know without asking. Accreditation is voluntary, and many pharmacies operate without it. But non-accredited facilities have error rates up to 12 times higher than accredited ones. If a pharmacy won’t show you their protocols, their training records, or their environmental logs, you’re taking a risk. For critical medications-like hormones, chemotherapy, or pediatric doses-don’t settle for less than accredited.
What should I do if I suspect a compounded medication is wrong?
Stop taking it immediately. Contact your pharmacist and ask for the batch record, ingredient lot numbers, and verification signatures. Compare the label to your prescription. If something doesn’t match, contact your doctor and report it to your state board of pharmacy. You can also report it directly to the FDA’s MedWatch program. Don’t wait for symptoms. Early detection saves lives.



Let me just say this: if your pharmacy doesn’t have an ISO Class 5 cleanroom for sterile compounding, you’re not a pharmacy-you’re a biohazard waiting to happen. I’ve seen facilities where the techs wear the same lab coat for three days, sneeze into their gloves, and call it ‘good enough.’ And then we wonder why kids end up in PICU. This isn’t about perfection-it’s about basic human decency. The FDA’s 27 fentanyl deaths? That’s not an accident. That’s negligence dressed up as ‘cost-cutting.’
Wow. This post reads like someone took a textbook, drank three espressos, and wrote it in a single sitting. 😅 But honestly? Every word matters. I work in a non-accredited compounding shop-we’re small, underfunded, and overworked. We do dual checks, we have HEPA filters (even if they’re secondhand), and we label everything like our lives depend on it. Because they do. Maybe we’re not PCAB-certified… but we’re trying. And that counts.
Thank you for writing this with such care. 💙 I’m a caregiver for my mom, who gets a custom hormone gel every month. I didn’t know any of this-until she had a reaction last winter. Now I ask for batch records, I check the labels like a hawk, and I always ask if they do dual verification. It’s scary how little patients know. You’ve given me the words to ask the right questions. Please keep sharing this.
Just wanted to add-my cousin works at a PCAB-accredited pharmacy in Oregon. They do media fill tests every week, and the staff rotates through ‘error simulation’ drills. One time, someone was handed the wrong powder and had to stop the whole batch. No shame, no yelling-just a quiet debrief and a new training module. That culture? That’s what saves lives. Not the fancy machines. The people.
Dual verification. Cleanroom. Labeling in mg/mL. No abbreviations. Training. Accreditation. These aren’t suggestions. They’re non-negotiables. Skip one, and you’re gambling. Skip two, and you’re reckless. Skip three, and you’re a liability. End of story.
AI tools are awesome 🤖 but they can’t smell a contaminated hood or notice a technician’s shaky hands. My buddy’s pharmacy got burned because they trusted the scanner too much-barcode was smudged, AI said ‘all good,’ and boom-wrong dose. Human eyes still matter. Always. Also, please use ‘micrograms’ instead of ‘mcg.’ I’m not mad… I’m just disappointed 😔
If you’re running a compounding pharmacy and you’re not accredited, you’re not just cutting corners-you’re putting children, cancer patients, and elderly folks at risk. There’s no ‘maybe’ here. No ‘we’re working on it.’ You either meet the standard or you stop. Period. If you can’t afford accreditation, get funding. Get a grant. Partner. But don’t keep risking lives because you’re ‘too busy.’ Your patients aren’t busy. They’re dying.
Ah, the tragedy of modern medicine-where the sacred art of healing has been reduced to a checklist of ISO classifications, barcode scanners, and sterile hoods. But tell me, dear reader, when did we forget that compounding was once a poetic act? A pharmacist, kneeling before a mortar and pestle, whispering intentions into the powder, blending not just molecules but hope? Now we have algorithms and audits, and the soul of pharmacy has been buried under a mountain of compliance forms. Is safety worth the death of reverence? Or have we, in our quest to prevent error, lost the very humanity that makes healing possible?