Every year, over 350,000 preventable medication errors happen in nursing homes and senior homes across the U.S. - and many of them happen because of simple, fixable mistakes. Seniors take more medications than any other group. Nearly 90% of people over 65 are on at least one prescription, and 40% are taking five or more daily. That’s a lot of pills, a lot of schedules, and a lot of chances for something to go wrong. But it doesn’t have to. With clear, practical steps, you can dramatically reduce the risk of dangerous side effects, hospital visits, or worse. These five medication safety tips are backed by the National Institute on Aging, the FDA, and leading geriatric experts - and they work in real homes, not just clinics.
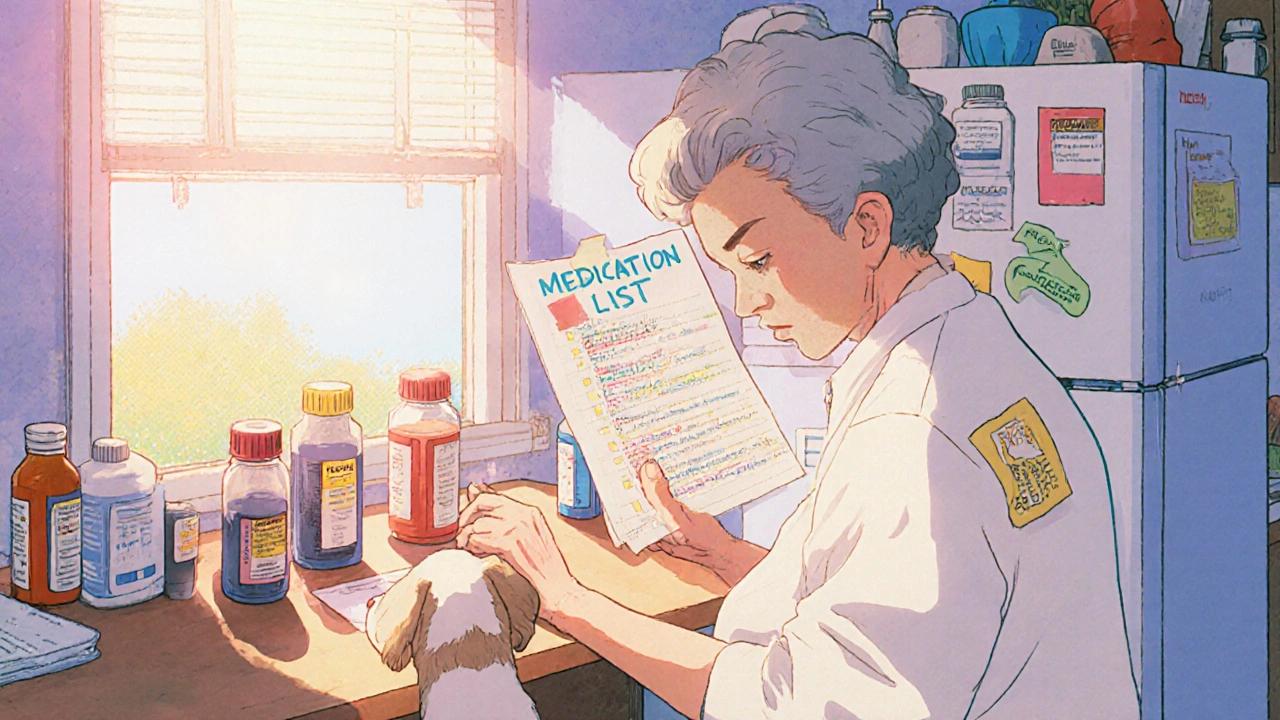
Keep a Complete, Updated Medication List
Don’t rely on memory. Don’t trust a scribbled note on a napkin. Every senior on multiple medications needs a written list that includes everything they take - prescriptions, over-the-counter painkillers, vitamins, herbal supplements, even eye drops. The list must have the full name of each medication, the exact dose (like 5 mg, not "one pill"), how often to take it (twice daily? every 8 hours?), why it’s prescribed, who wrote the prescription, and the pharmacy’s phone number. Also note start dates, expiration dates, and any known side effects. The Health in Aging Foundation says this list needs all 10 of these details to be truly useful.Update it within 24 hours of any change - whether a new drug is added, a dose is changed, or one is stopped. Bring this list to every doctor’s visit, ER trip, or pharmacy pickup. Pharmacists say 92% of dangerous drug interactions are caught just by having this list in hand. If your parent has memory issues, keep a copy taped to the fridge and another in their wallet. Some pharmacies offer free printed lists - ask for one at your next refill.
Use a Pill Organizer - But Choose the Right One
A simple pill box can cut missed doses in half. But not all organizers are created equal. For seniors with mild memory problems, a 7-day organizer with separate compartments for morning, afternoon, and evening works best. Color-coding helps - blue for morning, red for night. Studies show this improves adherence by 47% in people with early dementia.But if your loved one is doubling up doses or forgetting they already took their pill, a locked organizer is safer. Some models require a code or key to open. If they’re tech-savvy, apps like Medisafe (rated 4.7 out of 5 by over 18,000 users) send phone alerts and let caregivers know if a dose is skipped. But don’t assume tech always helps. One caregiver on Reddit said her $100 app made things worse - her mom kept dismissing alerts without taking pills, and she didn’t get notified until her blood sugar crashed. Low-tech solutions like laminated photo charts - showing each pill with its name and purpose - work better for many. AARP’s 2023 survey found 55% of seniors over 75 prefer paper schedules over apps. Start simple: one compartment per day, then add times as needed. The CDC warns that 38% of seniors over 80 struggle with complex organizers. Don’t overwhelm them.

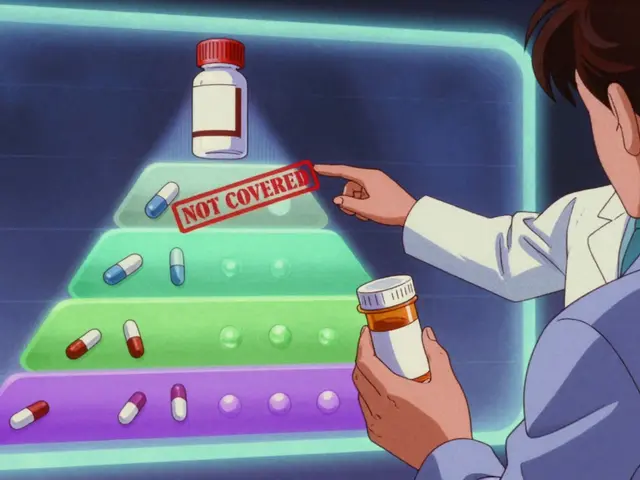
Check for Dangerous Interactions
Many seniors don’t realize that grapefruit juice can make blood pressure meds or cholesterol drugs dangerously strong. Or that mixing alcohol with sleep aids, antidepressants, or diabetes pills can cause fainting, falls, or even coma. The Beers Criteria®, updated every two years by the American Geriatrics Society, lists 138 medications that are risky for older adults - including common ones like Benadryl, sleeping pills, and certain painkillers. If a new prescription comes in, ask the pharmacist: "Is this on the Beers list?"Always check new meds against the full list of current ones. Even something as simple as ibuprofen can raise blood pressure or damage kidneys when taken with heart meds. The FDA warns that 85 commonly prescribed drugs interact with grapefruit. Alcohol interacts with over 150. If your parent drinks wine daily or eats grapefruit for breakfast, tell the doctor. And never assume a "natural" supplement is safe. St. John’s Wort, ginkgo, and garlic pills can interfere with blood thinners, antidepressants, and even chemotherapy. When in doubt, call the pharmacist. They’re trained to spot these clashes - and they won’t charge you for the advice.
Store Medications Correctly - Not in the Bathroom
The bathroom medicine cabinet is the worst place to keep pills. Heat and steam from showers can break down medications, making them weaker or even toxic. A 2022 University of Florida study found that 37% of common drugs lose effectiveness when stored in humid bathrooms. The right temperature? Between 68°F and 77°F - like a bedroom drawer or kitchen shelf. Keep them dry, away from sunlight, and out of reach of kids or pets. The Poison Control Center reports 60,000 accidental poisonings in children each year from unlocked medicine cabinets.If you live with grandchildren, get a locked storage box - even if your senior doesn’t seem confused. Many older adults don’t realize their own memory lapses put others at risk. Also, never crush pills unless the doctor says it’s okay. Time-release tablets, like those for high blood pressure or Parkinson’s, can become dangerous if crushed. And never keep old meds. The average senior home has $317 worth of expired or unused pills. Take them to a pharmacy drop-off box or a DEA take-back event. Don’t flush them - that pollutes water supplies.
Ask the Right Questions at Every Appointment
Doctors are busy. They won’t always ask if a medication is still needed. You have to. Prepare three simple questions before every visit:- "Is this medication still necessary?" - Many seniors stay on drugs long after the original reason is gone.
- "What interactions should I watch for?" - Especially with new meds or lifestyle changes.
- "Are there cheaper or safer alternatives?" - Some older drugs cost pennies and work just as well as expensive new ones.
- "What are the signs of a dangerous side effect?" - Dizziness? Confusion? Bruising? Nausea? Know what to call the doctor about.
The Alzheimer’s Association found that using these questions reduces medication errors by 63% in dementia patients. Even if your parent can’t speak for themselves, go with them. Bring the medication list. Take notes. Don’t be afraid to say, "I need to understand this better." If you’re overwhelmed, ask for a medication therapy management (MTM) session. Medicare Part D offers free 20- to 30-minute consultations with pharmacists for seniors on 8+ medications. They’ll review everything, flag risks, and even help you find lower-cost options. And if you’re still unsure, ask for a referral to a geriatric pharmacist - they specialize in senior meds and are now in 87% of hospital systems.
What If It Still Feels Overwhelming?
You’re not alone. Two-thirds of caregivers say managing medications is their biggest stressor. If the system feels too complex, start small. Pick one tip - maybe the pill organizer - and stick with it for a month. Build the habit. Then add the next. The National Institute on Aging says it takes 21 to 30 days for a new routine to stick. Use visual cues: a sticky note on the fridge, a daily alarm on your phone, a checklist taped to the medicine cabinet.Some families create a "medication buddy" system - one person handles refills, another checks doses, a third calls the pharmacy. That cuts errors by over 30%. And don’t forget: the NIA’s free "Medication Check-Up" program offers in-home reviews by pharmacists through 11,000 Area Agencies on Aging nationwide. Call your local agency - it’s free, no insurance needed. You’re not just preventing a bad reaction. You’re protecting independence, reducing hospital trips, and giving your loved one more good days at home.
Can I just cut pills in half to save money?
Only if the pill is scored and your doctor or pharmacist says it’s safe. Many pills - especially time-release, enteric-coated, or capsules - should never be split. Crushing or splitting them can release the full dose at once, causing dangerous side effects. Always ask before cutting any pill.
What if my parent refuses to take their meds?
Refusal often comes from side effects, confusion, or fear. Don’t force it. Talk to the doctor - maybe the dose can be lowered, or a different drug used. Sometimes the issue isn’t the pill, but the routine. Try giving meds with a favorite snack or at the same time as a daily ritual like brushing teeth. If it’s memory-related, a smart dispenser like Hero can help, but only if the person doesn’t override it. If refusal continues, ask about a geriatric psychiatrist - behavioral issues around meds are common and treatable.
Are herbal supplements safe for seniors?
Not necessarily. Many seniors think "natural" means safe, but supplements aren’t regulated like drugs. St. John’s Wort can make antidepressants and birth control useless. Ginkgo can increase bleeding risk with blood thinners. Garlic and fish oil can thin blood too. Always list every supplement on the medication list - even if you think it’s harmless. Pharmacists see more dangerous interactions from supplements than from prescriptions.
How do I know if a medication is expired?
Check the expiration date on the bottle or box. If it’s past that date, don’t use it - even if it looks fine. Some meds, like insulin or liquid antibiotics, become ineffective or even harmful after expiration. Others, like aspirin or antibiotics, can break down into toxic compounds. When in doubt, toss it. Many pharmacies offer free disposal bins. Never keep expired meds around - they’re a risk to everyone in the home.
Can I use a pill organizer for liquid medications?
No. Pill organizers are designed for solid tablets and capsules. Liquid meds need to be measured accurately with a syringe or dosing cup. Putting liquids in pill compartments can lead to spills, contamination, or wrong doses. Keep liquid meds in their original bottles with clear labels. Use a dosing syringe - not a kitchen spoon - for accuracy. Some pharmacies offer pre-measured liquid doses in unit-dose cups if you need help.
Medication safety isn’t about perfection - it’s about reducing risk. Even small changes - a better list, a locked organizer, one question asked at each appointment - add up. Seniors aren’t failing at managing meds. The system is often too complex. With the right tools and clear communication, most of these risks can be avoided. And that means more days at home, fewer hospital visits, and better health for the people who matter most.




Let’s be real - most of these ‘tips’ are useless if your parent’s got dementia and thinks their pills are candy. I’ve seen grandmas swallow 12 pills at once because the bottle said ‘take one’ and they took it as a challenge. The only thing that works? A locked cabinet, a nurse on speed dial, and a shotgun pointed at the medicine cabinet when they try to raid it. Seriously. I’ve seen more overdoses from ‘natural supplements’ than from actual prescriptions. St. John’s Wort? That’s just herbal Prozac with a side of suicidal ideation. And don’t get me started on grapefruit juice - it’s basically liquid betrayal.
And yes, I’ve had to call 911 twice. No, I don’t sleep much anymore. You think this is a checklist? It’s a war zone.
Oh, and ‘ask questions at appointments’? Good luck when your mom’s 89 and thinks the doctor’s a spy. She told him last week his stethoscope was a ‘government bug.’ He nodded. I cried in the parking lot.
These guidelines are fundamentally inadequate. The National Institute on Aging? The FDA? These are bureaucratic entities that operate under the assumption that patients are rational actors with access to stable healthcare infrastructure - which is a fantasy in 90% of rural America. You cannot rely on ‘pill organizers’ when the patient’s cognitive function is declining and their vision is deteriorating. The CDC’s 38% statistic is meaningless without context: most seniors lack digital literacy, transportation, and familial support. Moreover, the recommendation to ‘consult a pharmacist’ assumes that pharmacies are staffed with competent, adequately trained professionals - which is patently false in underfunded communities. The real issue? Systemic underinvestment in geriatric care. This article is a Band-Aid on a hemorrhage.
And let’s not forget: the FDA approves drugs based on clinical trials with participants under 65. The ‘Beers Criteria’ is a noble attempt - but it’s reactive, not proactive. We need mandatory geriatric pharmacology training for all prescribers. Not ‘tips.’ Structural reform. Or we’ll keep burying our elders because someone thought a laminated chart was enough.
I’ve been caring for my 92-year-old aunt for five years now, and let me tell you - this article hit me right in the heart. I used to think I was doing everything right until one day I found her holding three different bottles of ibuprofen, all half-empty, because she couldn’t remember which one she’d already taken.
We started with just one thing: a big, bright, color-coded chart taped to the fridge. I drew pictures of each pill - a little blue circle for the blood pressure one, a red heart for the cholesterol, a green leaf for the vitamin D. She’d point to them every morning and say, ‘There’s my little friends.’ It made her feel like she was in control. We didn’t need an app. We didn’t need a fancy organizer. We just needed her to feel seen.
And the pharmacist? Oh, honey. The pharmacist at our little corner store remembers her name, her dog’s name, and that she hates the taste of the liquid antibiotic. He gives her lollipops after her refill. That’s the kind of care that saves lives - not just checklists.
Don’t underestimate the power of kindness. Sometimes, the safest medicine is someone who shows up - every day - and says, ‘I’m here. Let’s do this together.’
Okay, I’ve got to say - this whole thing is a circus. I tried the pill organizer. My dad tried to eat it. No, seriously. He thought it was a snack box. I bought the $100 app. He kept hitting ‘snooze’ for 17 hours straight. Then he called the pharmacy and demanded a refund because the ‘robot voice’ was ‘talking too fast and sounded like a robot from a horror movie.’
So now? We have a whiteboard. I write the meds in giant marker. I put a smiley face next to the ones he likes. He gets a cookie after he takes them. Yes, it’s ridiculous. Yes, it’s working. He’s had zero ER trips in six months.
Also - grapefruit juice? I banned it. He cried. I cried. We compromised: one sip on Sundays. He calls it ‘The Devil’s Juice.’ I call it ‘The Reason I Still Have a Dad.’
And yes, I still sleep with one eye open. But hey - we’re still here. And that’s a win.
It’s funny how we treat medication like it’s a math problem when it’s really a human one. We obsess over pill boxes and expiration dates like if we just get the logistics right, everything will be fine. But the truth? The real danger isn’t the grapefruit juice or the expired aspirin - it’s the loneliness. The isolation. The fear that if you forget to take your pill, you’re a burden. That if you mess up, you’re failing.
I’ve sat with people who’ve been on the same meds for 15 years and never once asked if they still needed them. Why? Because they’re terrified of being told, ‘You’re not sick anymore.’ They’ve been told for so long that their worth is tied to their prescriptions. So they cling to them - even when they’re harmful.
That’s why the question ‘Is this still necessary?’ is revolutionary. Not because it’s a checklist item - but because it says, ‘I see you as more than your diagnosis.’
And yes, I’ve seen people cry when they finally stopped taking a drug they’d been on since 1998. They didn’t feel better right away. But they felt freer. And that’s the real safety tip: treating the person, not just the pill bottle.
EVERYTHING IN THIS ARTICLE IS A GOVERNMENT LIE. The FDA doesn’t care about seniors - they’re in bed with Big Pharma. That ‘Beers Criteria’? Made up by people who get paid by drug companies to say what’s ‘safe.’ Grapefruit juice? It’s not the juice - it’s the 5G towers in the pharmacy that interfere with the meds. The ‘pill organizers’? They’re microchipped. The apps? They track your brainwaves and sell your data to the CIA. I know because my cousin’s neighbor’s uncle got his meds hacked and his blood pressure spiked to 220 - then he vanished. They took him to a ‘geriatric pharmacy’ and he never came back.
And don’t get me started on ‘medication therapy management’ - that’s just a front for the NSA to monitor your pill intake. Why do you think they want you to ‘call your local agency’? So they can send the drones. I stopped taking all meds. Now I drink lemon water and hum Gregorian chants. My BP is 110/70. Coincidence? I think not.
They’re trying to control us. Don’t be a sheep. Burn the list. Trust your gut. And if you see a pharmacist wearing a blue shirt - RUN.
Stop putting pills in the bathroom. 🙄
It’s not rocket science. Moisture ruins meds. Basic science. Why are we even having this conversation?
Love this! 🙌 I’m from India, and here, elders often take 10+ meds without any list - just ‘this one for blood, that one for sleep, and the green one for when you feel bad.’ I showed my aunt this article, and now she has a notebook with doodles of pills and a little star for the ones she takes with chai. She says it’s her ‘medicine diary.’
Also - grapefruit juice? We use lime instead. No interactions, tastes better, and my uncle says it ‘makes his heart dance.’ 🍋❤️
And yes, I cried when I read about the whiteboard. My grandma used to draw flowers on the fridge after taking her pills. We kept it up for years. Turns out, love is the best pill organizer.
Thanks for writing this. Not just helpful - human.