When you take a pill, you assume it’s the right one, at the right dose, at the right time. But medication mistakes, preventable errors in prescribing, dispensing, or taking drugs that cause harm. Also known as drug errors, these aren’t rare accidents—they happen every day, often silently, and can turn a simple treatment into a life-threatening event. The FDA reports that over 1.5 million people are injured each year in the U.S. because of medication errors. Most of these aren’t caused by doctors or pharmacists alone—they’re the result of a chain of small oversights that add up.
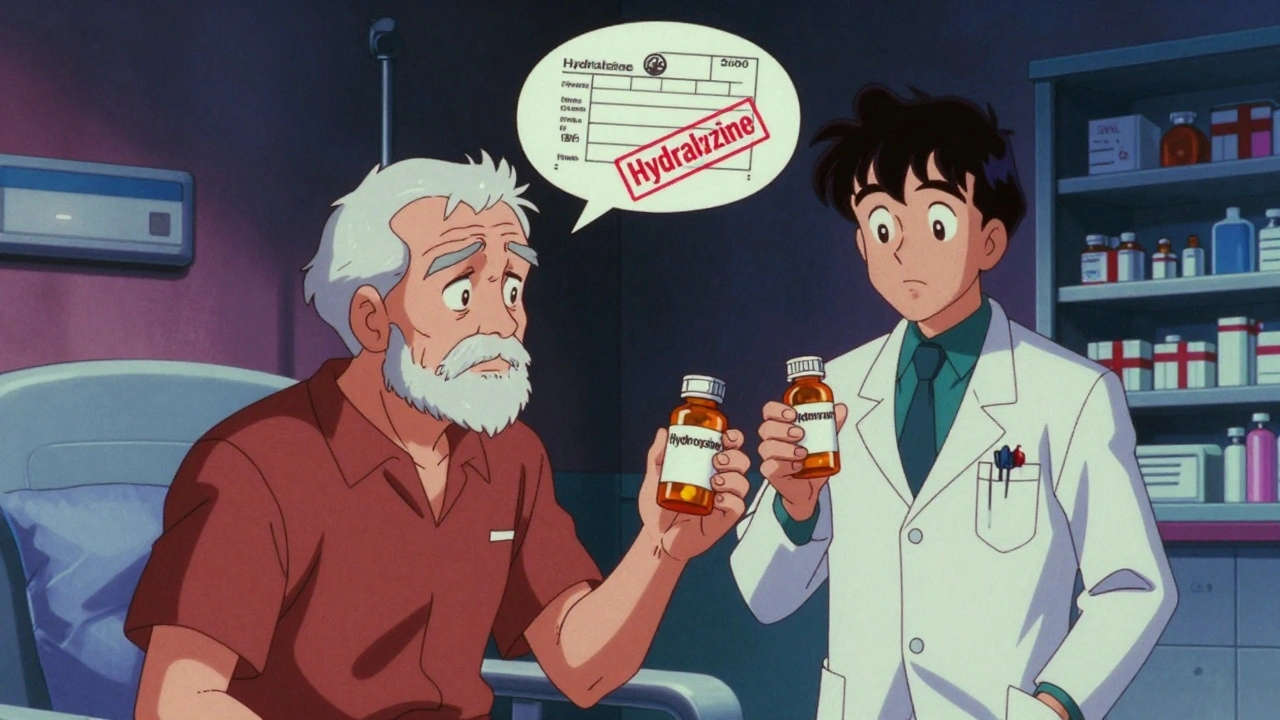
One of the biggest culprits is LASA medications, look-alike and sound-alike drug names that confuse patients and staff alike. Examples include Hydralazine and Hydroxyzine, or Celebrex and Celestone. One letter, one syllable, and suddenly you’re giving a blood pressure drug to someone who needs an antihistamine. These mix-ups are so common that hospitals now use tall-man lettering (like HYDRA-lazine) to reduce confusion. But patients need to know too: if a drug name sounds like another you’ve taken before, pause. Ask. Double-check. Then there’s drug interactions, when two or more medications react in ways that reduce effectiveness or cause dangerous side effects. For instance, taking an antacid with doxycycline can slash antibiotic absorption by up to 90%. Or mixing alcohol with sucralfate and delaying ulcer healing. These aren’t theoretical risks—they’re daily realities for millions. And when you’re on multiple meds, especially as a senior, the risk multiplies. A pill organizer might help, but if you don’t know why you’re taking each one, you’re just moving pills around.
Some mistakes are invisible until it’s too late. A patient might think their Zyrtec stopped working, when really, their symptoms changed—or they’re taking it wrong. Someone with diabetes might not realize their diet is making their metformin less effective. Or a person on warfarin might not know their genetics affect how their body processes the drug, making them prone to dangerous bleeding. These aren’t just "side effects"—they’re signals that something’s off in the system. That’s why knowing how to report an adverse drug reaction, an unexpected and harmful response to a medication taken at normal doses to the FDA matters. Your report could help stop others from making the same mistake.
You don’t need to be a pharmacist to catch these errors. You just need to ask the right questions: Why am I taking this? What happens if I miss a dose? Could this interact with my other meds or food? Is this the same as the last one I got? And if something feels wrong—like a sudden headache, unexplained bruising, or nausea after starting a new pill—don’t wait. Don’t assume it’s "normal." That’s how serious problems turn into emergencies.
Below, you’ll find real-world guides that break down exactly how these mistakes happen—and how to stop them before they hurt you or someone you care about. From confusing drug names to genetic risks, from mail-order pharmacy quality to how to get a second opinion when something doesn’t feel right—this collection gives you the tools to take control. You’re not just a patient. You’re the most important part of your own safety team.
Learn how to tell the difference between medication errors and drug side effects-why confusing them puts patients at risk and how to spot each one correctly.
