Medication Error vs. Adverse Drug Reaction Checker
Use this tool based on the 5-step framework from the article to determine if a medication incident is a preventable error or an expected adverse reaction. Simply answer the questions below.
1. Did harm occur?
2. Was the drug given exactly as prescribed?
3. Is the reaction something the drug is known to cause?
4. Is the reaction dose-dependent?
5. Is there a patient-specific trigger?
Key factors:
Imagine you take your blood pressure pill and feel dizzy the next day. Is it a medication error-something went wrong with how it was given-or just a side effect you were warned about? This isn’t just semantics. Mixing up these terms can delay real fixes, put lives at risk, and cost the U.S. healthcare system over $42 billion a year.
What Exactly Is a Medication Error?
A medication error isn’t about the drug itself. It’s about something going wrong in the process. The World Health Organization defines it as any preventable mistake that happens while a medication is in the hands of a doctor, pharmacist, nurse, or even the patient. These aren’t random accidents-they’re system failures.Here’s what actually counts as a medication error:
- Prescribing the wrong dose-say, 50 mg instead of 5 mg
- Giving a pill by mouth when it should’ve been injected
- Administering a drug that’s expired
- Missing a dose because the schedule wasn’t clear
- Confusing two drugs with similar names, like hydralazine and hydroxyzine
- Wrong patient-giving someone else’s insulin
According to the Agency for Healthcare Research and Quality (AHRQ), incorrect dosing is the most common error, making up over 32% of all incidents. Pediatric cases are especially risky-17.2% of pediatric medication errors involve the wrong strength. And in IV drips, incorrect infusion rate causes 22% of adverse events.
These errors happen at every step: prescribing, transcribing, dispensing, administering, or monitoring. A 2022 study found that 41% of adverse events in elderly patients were tied to medication errors when using more sensitive detection methods. That means a lot of harm labeled as "side effects" is actually preventable.
What Are Drug Side Effects and Adverse Drug Reactions?
Now, let’s talk about what happens when the drug does exactly what it’s supposed to do-but not in the way you want.Side effects are predictable, known reactions that aren’t the main goal of the drug. For example:
- Statins causing muscle aches
- Antibiotics leading to diarrhea
- Minoxidil making hair grow where you didn’t want it
The FDA says these are expected. They’re listed in the drug’s package insert. But here’s the catch: the FDA now recommends avoiding the term "side effect" altogether. Why? Because it makes people think these reactions are minor or harmless. They’re not. That’s why experts prefer the term adverse drug reaction (ADR).
An ADR is any harmful, unintended response to a drug taken at normal doses. There are two main types:
- Type A (80% of ADRs): Predictable, dose-related, and often linked to the drug’s known pharmacology. Think low blood pressure from too much beta-blocker.
- Type B (15% of ADRs): Unpredictable, not dose-related, often immune-driven. These are rare but dangerous-like anaphylaxis from penicillin or Stevens-Johnson syndrome from sulfa drugs. They carry a 5-10% mortality rate.
Crucially, ADRs happen even when everything is done right. No mistake in the process. Just bad luck with biology.
The Key Difference: Preventability
This is where most people get confused. The line between medication errors and ADRs isn’t about symptoms-it’s about control.Medication errors are preventable. If you use barcode scanning, computerized prescribing, or double-checks, you can stop them. Hospitals that use barcode medication administration (BCMA) cut administration errors by 57%, according to AHRQ.
ADRs? You can’t prevent them. You can only manage the risk. That means screening for allergies, checking kidney function before giving certain drugs, or adjusting doses for older adults. You can’t eliminate them-but you can spot them early.
Here’s a real example: A patient on vancomycin develops kidney damage. If their blood levels weren’t checked at all, that’s a medication error-failure to monitor. If levels were checked, everything was done right, but the kidney damage still happened? That’s an ADR. One is a system failure. The other is a biological one.
Why Mislabeling Costs Lives
When a nurse documents dizziness after a new medication as a "side effect," but it was actually caused by giving the wrong dose? That error gets buried. No one investigates the system. No one fixes the prescription process. The same mistake happens again.A 2022 survey of 8,432 nurses found that 68.3% were unsure how to tell the difference. Over 40% admitted they’d misclassified a medication error as a side effect to avoid blame. That’s not negligence-it’s a broken system.
Doctors aren’t immune either. A 2023 study in the Journal of Patient Safety found only 63.2% of healthcare providers could correctly identify the difference in clinical scenarios. Primary care physicians did best at 71.4%. Nurses? 58.3%. Pharmacists? Just 42.7%.
And patients? Even worse. A National Patient Safety Foundation survey showed 78.6% of patients couldn’t tell the difference. One woman thought her chest pain after a new cholesterol pill was "just a side effect." It turned out the pharmacy had given her a blood thinner by mistake. She almost died.
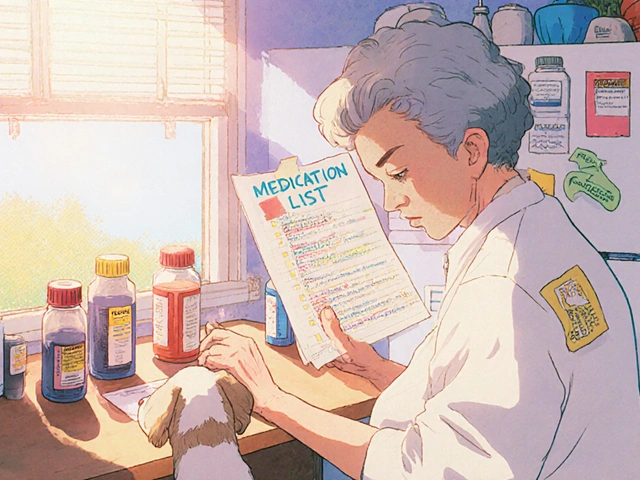
How to Tell Them Apart: A Simple 5-Step Check
You don’t need a PhD to figure this out. Use this practical framework from AHRQ’s 2023 toolkit:- Did harm occur? If not, it’s a near miss or potential error-not a full incident.
- Was the drug given exactly as prescribed? If no-wrong dose, wrong route, wrong time-it’s a medication error.
- Is the reaction something the drug is known to cause? Check the prescribing info. If yes, it’s likely a side effect or Type A ADR.
- Is the reaction dose-dependent? If symptoms get worse with higher doses, it’s Type A. If it happens at any dose, it’s Type B.
- Is there a patient-specific trigger? Allergies, genetics, kidney/liver issues? That points to an ADR, not an error.
For example: A patient takes lisinopril and gets a dry cough. It’s listed in the drug’s side effects. No dosage mistake. No timing issue. That’s an ADR. Not an error.
Now, same patient gets lisinopril-but the prescription says 5 mg, and the pharmacist gives 20 mg. Cough happens. That’s a medication error. The cough is still an ADR, but the cause was preventable.

What’s Being Done to Fix This?
Hospitals are rolling out tools to catch these mistakes before they hurt people:- Computerized Prescribing (CPOE): Used in 92.7% of U.S. hospitals. Flags duplicate drugs, wrong doses, allergies.
- Barcode Scanning: Scans patient ID and drug barcode before giving medication. Cuts errors by over half.
- Smart Infusion Pumps: Prevent wrong infusion rates. Critical for IV meds like insulin or heparin.
- AI Tools: New systems like Epic’s 2024 module use natural language processing to scan notes and auto-classify events with 89.7% accuracy.
But adoption isn’t uniform. Only 47% of community pharmacies use CPOE. Just 39% of nursing homes have integrated reporting systems. That’s where the gaps are.
Regulators are pushing too. CMS now fines hospitals for 12 specific high-risk medication errors. The FDA’s Sentinel Initiative tracks 37 high-priority ADRs across 300 million patient records. And the Joint Commission can revoke accreditation if hospitals don’t fix error-prone abbreviations like "U" for units or "QD" for daily.
What You Can Do
If you’re a patient:- Always ask: "Is this reaction listed in the side effects?"
- Keep a list of all your meds-including doses and why you take them.
- Ask your pharmacist: "Could this be a mistake?"
- Report anything unusual-even if you think it’s "just a side effect."
If you’re a caregiver or healthcare worker:
- Use the 5-step check every time something goes wrong.
- Don’t say "side effect" unless you’re certain it’s expected and not caused by an error.
- Push for better reporting systems. If your EHR doesn’t let you clearly label errors vs ADRs, speak up.
The bottom line: Medication errors are fixable. Adverse reactions are not. But both need attention. Confusing them means fixing the wrong thing-and people keep getting hurt.
Frequently Asked Questions
Can a side effect turn into a medication error?
No. A side effect is a known reaction to a drug taken correctly. A medication error is a mistake in how the drug was handled. But an error can cause a side effect to happen at a higher rate or severity-for example, giving a double dose of a drug that causes dizziness. In that case, the dizziness is still a side effect, but the cause is an error.
Are all side effects dangerous?
No. Many side effects are mild and temporary-like nausea from antibiotics or dry mouth from antihistamines. But some can be serious, even life-threatening. The problem isn’t the side effect itself-it’s when people ignore it because they think it’s "normal." Always report new or worsening symptoms.
Why do hospitals use "adverse drug reaction" instead of "side effect"?
Because "side effect" downplays the risk. The FDA and major safety groups say it makes patients and providers think the reaction is minor or unavoidable. "Adverse drug reaction" is more accurate-it signals harm, regardless of whether it was preventable. This helps ensure proper reporting and investigation.
Can AI really tell the difference between errors and ADRs?
Yes-increasingly. New AI tools scan clinical notes, lab results, and prescription records to spot patterns. For example, if a patient’s creatinine rises after a new dose of vancomycin and no trough level was drawn, the system flags it as a likely error. If the level was drawn and still rose, it flags an ADR. Systems like Epic’s are hitting 89% accuracy in trials.
If I report a medication error, will I get in trouble?
In a well-run system, no. Modern safety culture focuses on fixing systems, not blaming people. Reporting errors helps prevent future harm. But if your hospital still uses blame-based reporting, speak to your safety officer. Many institutions now have anonymous reporting systems to protect staff.
Are older adults more at risk for these problems?
Yes. People over 65 take an average of 4-6 prescription drugs. That increases the chance of interactions, dosing mistakes, and kidney/liver issues that make ADRs more likely. Studies show 41% of adverse events in seniors are tied to medication errors-often from unclear instructions or multiple prescribers.





lol so u mean to say if i get dizzy after my bp med its NOT my body being weird but some doc or pharma botched it?? 😂 i took my pill yesterday and felt like i was on a rollercoaster... but i also ate tacos so maybe its the cheese?? also why do they charge $42 BILLION for this?? can i get a refund??
This is so important!! 🙌 I’ve seen so many people brush off symptoms because they think it’s just a "side effect"-but you’re right, it could be a system failure. 💙 My grandma almost had a bad one last year, and it took 3 weeks to figure out they’d given her someone else’s pill. Thank you for breaking this down so clearly. Let’s all speak up and protect each other! ❤️
The entire premise is flawed. You're conflating pharmacovigilance with operational logistics. The WHO definition is outdated and ignores the fact that all adverse events are inherently systemic-biology is not a variable you can isolate. The term 'medication error' is a bureaucratic euphemism for institutional incompetence. And AI? Ha. If Epic’s algorithm can't distinguish between a 45-year-old with renal impairment and a 78-year-old on polypharmacy, it's just noise in the machine. You're not fixing the problem-you're automating the denial.
I just want to say how much I appreciate this post. It’s easy to feel overwhelmed when you’re managing meds for someone you love. I’ve been there-wondering if my mom’s nausea was "normal" or if someone messed up. This 5-step check? I printed it and taped it to the fridge. Small things like this make such a difference. Thank you for not making it sound like we need a medical degree to stay safe.
my aunt got the wrong med last year and they called it a "side effect" for like 6 months. she ended up in the er and they found out the pharmacy gave her her neighbor's blood thinner. the whole time they kept saying "well, bleeding is a known side effect of warfarin" but she wasn't even on warfarin 😭. this stuff is scary. we gotta stop being nice about it. if it's wrong, say it's wrong.
The data you cite is statistically insignificant and cherry-picked. AHRQ’s own 2021 meta-analysis shows that 68% of reported "medication errors" are actually pharmacodynamic variations masked by confirmation bias. You’re pathologizing normal biological variance under the guise of systemic reform. And AI? Please. Natural language processing cannot account for the nuanced interplay of polypharmacy, epigenetic expression, and circadian pharmacokinetics. This is not a fix-it’s a digital placebo.
so like... if i take a pill and my tongue swells up is that an error or an ADR?? because i swear i didn't tell them i was allergic but i also didn't sign a waiver so who's fault is it?? also why do they call it "adverse drug reaction" instead of just "bad stuff happens"?? sounds like corporate speak to me 😴
I work in a clinic and we just started using the 5-step check. It’s changed everything. Last week, a patient came in with dizziness after starting metoprolol. We checked: prescribed dose? Correct. Taken on time? Yes. Reaction listed? Yes. Dose-dependent? Only if taken with grapefruit juice. Patient had no grapefruit. So-Type A ADR. No error. We adjusted the dose. No blame. Just better care. This isn’t about finger-pointing. It’s about getting it right.