When you’re taking sitagliptin-metformin for type 2 diabetes, the medication does half the work. The other half? Your plate. Many people assume pills alone will fix their blood sugar-but that’s not how it works. Sitagliptin-metformin lowers glucose by helping your body use insulin better and reducing liver sugar output. But if you’re eating a diet full of refined carbs, sugary drinks, and processed snacks, you’re fighting against your own medicine. The truth? satagliptin-metformin works best when your diet supports it-not sabotages it.
How sitagliptin-metformin actually works
Sitagliptin is a DPP-4 inhibitor. It keeps GLP-1, a natural hormone, active longer. GLP-1 tells your pancreas to release insulin when blood sugar rises-especially after meals. Metformin, on the other hand, reduces how much sugar your liver dumps into your bloodstream and helps your muscles absorb glucose better. Together, they tackle two major problems in type 2 diabetes: insulin resistance and overproduction of glucose.
But here’s the catch: these drugs don’t create insulin out of thin air. They rely on your body’s existing ability to respond. If your diet keeps spiking your blood sugar every few hours, your pancreas gets worn out. Your muscles become less sensitive. Your liver keeps pumping out sugar. No pill can fully compensate for that.
What to eat to make sitagliptin-metformin work better
Research from the American Diabetes Association shows that people on metformin who followed a low-glycemic diet lowered their HbA1c by an extra 0.7% compared to those who didn’t change their eating habits. That’s the same drop you’d see from adding a second drug. Diet isn’t just helpful-it’s powerful.
Start with these three food rules:
- Choose whole grains over white bread, pasta, and rice. Oats, quinoa, brown rice, and barley digest slowly. They cause gentle rises in blood sugar instead of spikes.
- Fill half your plate with non-starchy vegetables. Broccoli, spinach, zucchini, peppers, and cauliflower are low in carbs and high in fiber. They slow sugar absorption and help you feel full.
- Pair carbs with protein or healthy fat. Eating a banana alone can raise your blood sugar fast. Eat it with a spoon of almond butter or a boiled egg, and the rise is much slower. That gives sitagliptin more time to do its job.
Avoid sugary drinks-soda, sweet tea, juice, even flavored yogurts. A single 12-ounce soda can contain 39 grams of sugar. That’s more than most people need in a whole day. These drinks cause rapid glucose surges, forcing your pancreas to overwork. That’s the opposite of what sitagliptin is trying to help.
What to avoid: foods that fight your medication
Some foods don’t just fail to help-they actively make sitagliptin-metformin less effective.
- Refined carbs: white bread, pastries, crackers, instant oatmeal. These break down into sugar fast, overwhelming your system.
- High-fat processed meats: bacon, sausages, deli meats. These aren’t just bad for your heart-they can increase insulin resistance, making metformin work harder.
- Artificial sweeteners in large amounts: While not directly harmful, some studies suggest frequent use may alter gut bacteria in ways that reduce insulin sensitivity. Stick to small amounts, if at all.
- Alcohol: Especially on an empty stomach. It can cause unpredictable drops in blood sugar, especially when combined with metformin. If you drink, always eat something first and limit to one drink a day.
Also, skip large meals. Eating too much at once-even healthy food-can cause a blood sugar surge that your medication can’t fully handle. Smaller, balanced meals every 3-4 hours keep glucose levels steady and reduce the burden on your body.
Timing matters: when you eat vs. when you take your pills
Sitagliptin is usually taken once a day, with or without food. Metformin is often taken with meals to reduce stomach upset. But timing your meals around your medication can boost results.
Take metformin with your largest meal of the day-usually dinner. That’s when your liver tends to release the most glucose overnight. Taking it with food helps blunt that rise.
Sitagliptin works best when your body naturally releases GLP-1 after eating. So don’t skip meals. Even a small snack like Greek yogurt with berries after lunch helps trigger the hormone your medication is trying to support.
Don’t go more than 5-6 hours without eating. Long gaps can cause your liver to release stored sugar, leading to high fasting glucose in the morning. That’s a common problem people blame on the medication-not their eating pattern.
Weight loss and sitagliptin-metformin: the hidden synergy
Metformin is one of the few diabetes drugs that can help with modest weight loss. But it doesn’t work miracles. People who lose 5-10% of their body weight see dramatic improvements in insulin sensitivity. That means your body needs less help from the drugs.
A 2024 study in the Journal of Clinical Endocrinology & Metabolism found that patients on sitagliptin-metformin who followed a Mediterranean-style diet lost an average of 6.2% of their body weight in six months. Those on a standard low-fat diet lost only 2.1%. The difference? Healthy fats from olive oil, nuts, and fish reduced inflammation and improved how cells responded to insulin.
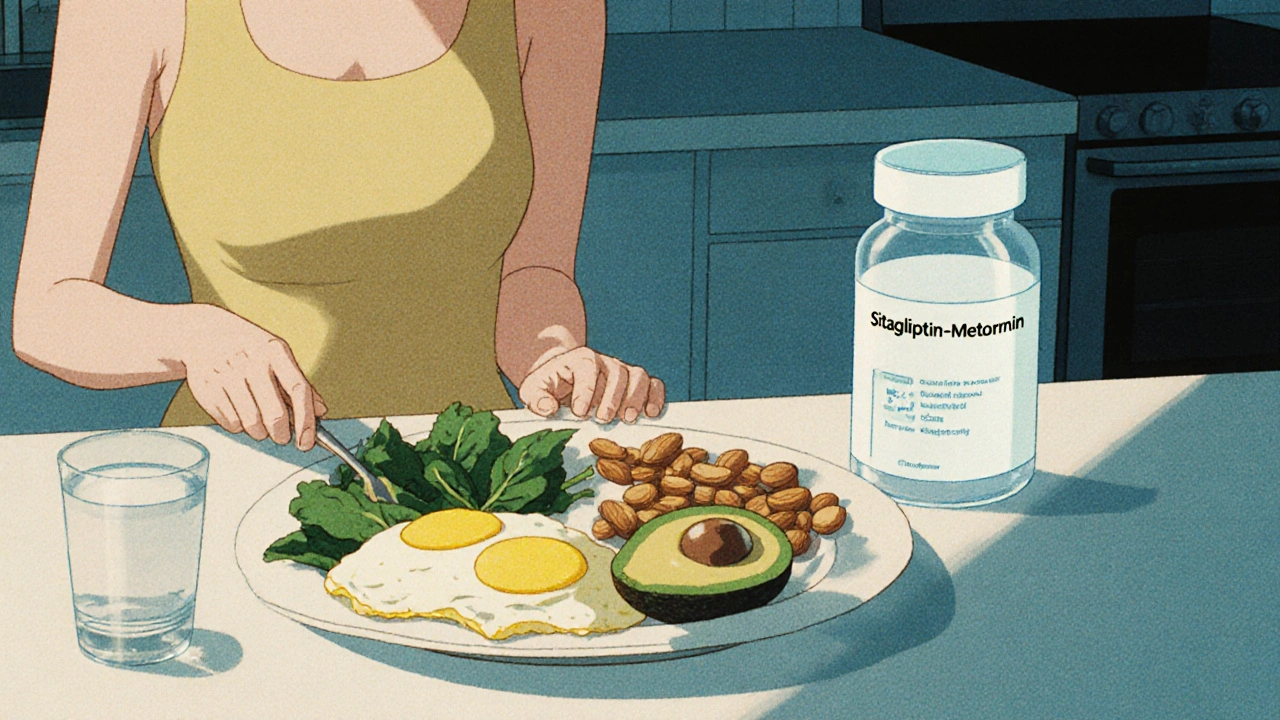
You don’t need to go keto or count calories. Focus on real food: vegetables, lean proteins, legumes, nuts, and whole grains. Cut out ultra-processed snacks. That’s enough to start seeing results.

Common mistakes people make with diet and sitagliptin-metformin
Here are the top three errors I see in clinic:
- "I’m taking medication, so I can eat whatever I want." This is the biggest mistake. Medication isn’t a license to ignore food.
- "I only worry about sugar." Fructose from fruit is fine. But hidden sugars in sauces, bread, and "healthy" granola bars add up fast. Read labels. If sugar is in the first three ingredients, avoid it.
- "I skip breakfast to lose weight." Skipping meals causes your liver to release glucose, raising fasting blood sugar. That’s when metformin should be working hardest-and you’re not giving it any help.
Also, don’t overdo fiber overnight. Suddenly eating 40 grams of fiber a day can cause bloating and gas. Increase it slowly-add a serving of beans or lentils a few times a week. Drink plenty of water. Your gut needs it.
Real-world example: Sarah’s turnaround
Sarah, 58, from Manchester, started on sitagliptin-metformin with an HbA1c of 8.4%. She was eating cereal for breakfast, a sandwich for lunch, pasta for dinner, and snacks like cookies and chips. After six months of changing her diet-swapping cereal for eggs and spinach, pasta for lentil stew, and chips for almonds-her HbA1c dropped to 6.2%. She lost 11 pounds. Her doctor reduced her metformin dose because her body was responding better.
She didn’t take supplements. She didn’t join a gym. She just ate differently. That’s the power of food.
When diet isn’t enough
Some people still struggle even with a clean diet. That’s normal. Genetics, stress, sleep, and activity levels all play roles. If your HbA1c stays above 7% after 3-6 months of good diet and medication, talk to your doctor. You might need a different combination or a GLP-1 agonist like semaglutide.
But don’t blame the medication. Blame the gaps between your plate and your pills. Fix the diet first. Then reassess.
Can I drink alcohol while taking sitagliptin-metformin?
Yes, but only in moderation and never on an empty stomach. Alcohol can cause low blood sugar, especially when combined with metformin. If you drink, have it with food, limit to one drink per day, and monitor your blood sugar closely. Avoid sugary mixers like soda or juice.
Does sitagliptin-metformin cause weight gain?
No-unlike some other diabetes drugs, sitagliptin-metformin is weight-neutral or may even help with modest weight loss. Metformin reduces appetite slightly and improves insulin sensitivity, which can help reduce fat storage. But if you’re eating too many calories-even from healthy foods-you won’t lose weight. Diet still matters.
What’s the best breakfast for someone on sitagliptin-metformin?
Avoid sugary cereals and pastries. Good options include: scrambled eggs with spinach and avocado, Greek yogurt with berries and chia seeds, or oatmeal made with water or unsweetened almond milk topped with nuts. These meals provide protein, fiber, and healthy fats to keep blood sugar steady.
Can I take metformin without food to avoid side effects?
No. Taking metformin on an empty stomach increases the risk of nausea, diarrhea, and stomach upset. Always take it with a meal. If side effects persist, talk to your doctor about switching to the extended-release version, which is gentler on the stomach.
How long does it take for diet changes to improve sitagliptin-metformin effectiveness?
You may notice less hunger and more stable energy within a week. Blood sugar readings often improve in 2-4 weeks. HbA1c, which reflects your average blood sugar over 3 months, typically drops by 0.5-1.0% after 3-6 months of consistent diet changes. Patience and consistency are key.
Your sitagliptin-metformin prescription isn’t a cure. It’s a tool. And like any tool, it works best when you use it the right way. Food isn’t the enemy-it’s your strongest ally. Start with one meal. Swap one processed snack for a handful of almonds. Add one extra vegetable to your dinner. Small steps, done daily, change everything.





This is why Africa is falling behind-people here still think pills fix everything. No diet? No change. We need education, not just medicine.
Let me be brutally honest-most people on this medication are just using it as a permission slip to keep eating garbage. They think if they take their pills, the universe owes them a free pass to pizza and soda. The truth? Your pancreas is screaming for mercy. Your liver is sobbing in the corner. And your doctor? They’re tired of watching you self-sabotage. This isn’t about willpower. It’s about respect-for your body, for your future, for the fact that you’re still breathing today because your cells haven’t given up on you yet. But if you keep treating your meds like a magic wand, you’re not just wasting your time. You’re disrespecting every scientist who spent decades making this work.
Excellent breakdown. The synergy between diet and pharmacology here is underappreciated. The 0.7% HbA1c reduction from dietary change alone is clinically significant-equivalent to adding a second drug without additional side effects. Consistency in meal timing, especially aligning metformin with the largest meal, optimizes hepatic glucose suppression. Also, the warning about artificial sweeteners is nuanced but valid; emerging gut microbiome research suggests chronic use may blunt GLP-1 response. Small, sustainable shifts matter more than perfection.
My grandma did this without knowing any of this science. She ate beans, greens, and cornbread-no fancy labels, no counting carbs. Just real food, slow cooked, shared with family. She lived to 92 with type 2. Maybe the answer isn’t in the pill bottle… it’s in the kitchen with someone who loves you enough to cook right.
Thank you for this 🙏 I started swapping soda for sparkling water with lemon last week and my afternoon crashes are gone. Small change, huge difference. 💪
If you’re still eating white bread, you deserve your HbA1c. No excuses.
Bro. Metformin is just a sugar blocker. You don’t need to eat kale. Just don’t eat sugar. That’s it. Stop overcomplicating it.
Who wrote this? Some pharmaceutical shill trying to sell you on the illusion of control? You think diet fixes diabetes? It’s a metabolic disorder caused by industrial food systems, corporate greed, and systemic neglect. Blaming the patient is the oldest trick in the book. Fix the food industry, not the plate.
It is not merely a matter of nutritional input but rather a complex interplay between pharmacokinetic modulation and the body's endogenous regulatory mechanisms. The pharmacodynamic efficacy of sitagliptin is contingent upon the presence of intact enteroendocrine signaling pathways which are, in turn, profoundly influenced by dietary macronutrient composition. The absence of refined carbohydrates permits sustained GLP-1 activity thereby augmenting insulinotropic effects. Metformin's hepatic gluconeogenesis suppression is rendered more efficacious under conditions of low glycemic load. Thus, dietary intervention is not ancillary-it is constitutive to therapeutic success. The notion that medication alone suffices is a profound misconception rooted in the commodification of health.
So if I eat rice and beans, I’m a hero? Cool. What if I can’t afford almonds or quinoa? Tell that to the guy working two jobs.
I tried this for two weeks and my blood sugar went up. So screw diet. I’ll just take more pills.
Thank you for writing this. I’ve been on this med for 3 years and never realized how much my breakfast cereal was hurting me. I switched to eggs and now I don’t feel like a zombie by 10am. Also-can we talk about how no one tells you that skipping meals makes your sugar spike? I thought fasting was healthy. Turns out it was making my diabetes worse. 🤦♀️
People act like this is some new revelation but my grandpa was doing this in the 50s. No meds, just food. Beans, greens, fish, no sugar. He lived to 98. We forgot how to eat. Now we’ve got a whole industry telling us what to eat while the real solution was in our grandparents’ kitchens the whole time.
Interesting how this article assumes everyone has access to fresh produce and the time to meal prep. Meanwhile, I’m eating microwaved meals because I work 12-hour shifts. Your advice is privileged. And your tone? Condescending.
Thank you for this thoughtful, well-researched piece. I’ve been struggling with my HbA1c for years, and this finally gave me clarity. I started with one change-swapping my afternoon cookie for a handful of walnuts-and after three months, my numbers dropped 1.2%. It’s not magic. It’s discipline. And it’s worth it. 💛