More than 1 in 10 people in the U.S. say they’re allergic to penicillin. But here’s the surprising truth: 9 out of 10 of them aren’t. That’s not a typo. Most people who think they have a penicillin allergy don’t actually have one. And this misunderstanding is putting lives at risk-not because of the drug itself, but because of what doctors are forced to use instead.
Why Mislabeling Penicillin Allergies Is Dangerous
When a patient says, "I’m allergic to penicillin," doctors often avoid all penicillin-related antibiotics. That sounds safe, right? Not really. It leads to the use of stronger, broader-spectrum drugs like vancomycin or clindamycin. These alternatives aren’t just more expensive-they’re less effective for many infections and increase the chance of deadly side effects like Clostridioides difficile (C. diff) infections or MRSA. A 2019 study in the Journal of Allergy and Clinical Immunology found that people labeled as penicillin-allergic had a 50% higher chance of getting MRSA and a 35% higher chance of C. diff compared to those without the label. The CDC estimates that fixing this one issue could save the U.S. healthcare system over $1.2 billion a year. In hospitals, avoiding penicillin because of a false allergy can mean longer hospital stays, more complications, and even higher death rates after surgeries.What Really Counts as a Penicillin Allergy?
Not every bad reaction is an allergy. Many people confuse side effects with allergies. If you got a stomachache, headache, or mild rash after taking penicillin, that doesn’t mean you’re allergic. True penicillin allergies involve your immune system overreacting. There are two main types:- Immediate reactions (within 1 hour): These are IgE-mediated and can be life-threatening. Symptoms include swelling of the lips, tongue, or throat; hives; trouble breathing; dizziness; or a sudden drop in blood pressure. This is anaphylaxis-and it needs epinephrine right away.
- Delayed reactions (hours to days later): These include rashes (often flat, red spots that spread), fever, joint pain, or organ damage like liver or kidney issues. Severe forms like Stevens-Johnson Syndrome (SJS) or DRESS are rare but dangerous.
- Anaphylaxis within 6 hours of taking penicillin
- Severe skin reactions like SJS or TEN
- Organ damage from a penicillin reaction (like kidney failure)
Testing for Penicillin Allergy: It’s Safer Than You Think
If you’ve been told you’re allergic, the best thing you can do is get tested. Penicillin skin testing is simple, quick, and extremely accurate. It involves a tiny prick of the skin with two forms of penicillin-major and minor determinants-followed by a small injection if the skin test is negative. If both are negative, doctors give you a full dose of amoxicillin (250 mg) and watch you for an hour. If you make it through without a reaction, your risk of anaphylaxis drops to nearly zero. That’s the same as someone who’s never claimed an allergy. This isn’t theoretical. Studies show that 90-95% of people who think they’re allergic pass this test. And here’s the kicker: even if you had a mild rash years ago, you might still be able to safely take penicillin or a related antibiotic like cefazolin. The American Academy of Allergy, Asthma & Immunology says testing can safely open up first-line antibiotics for 9 out of 10 patients.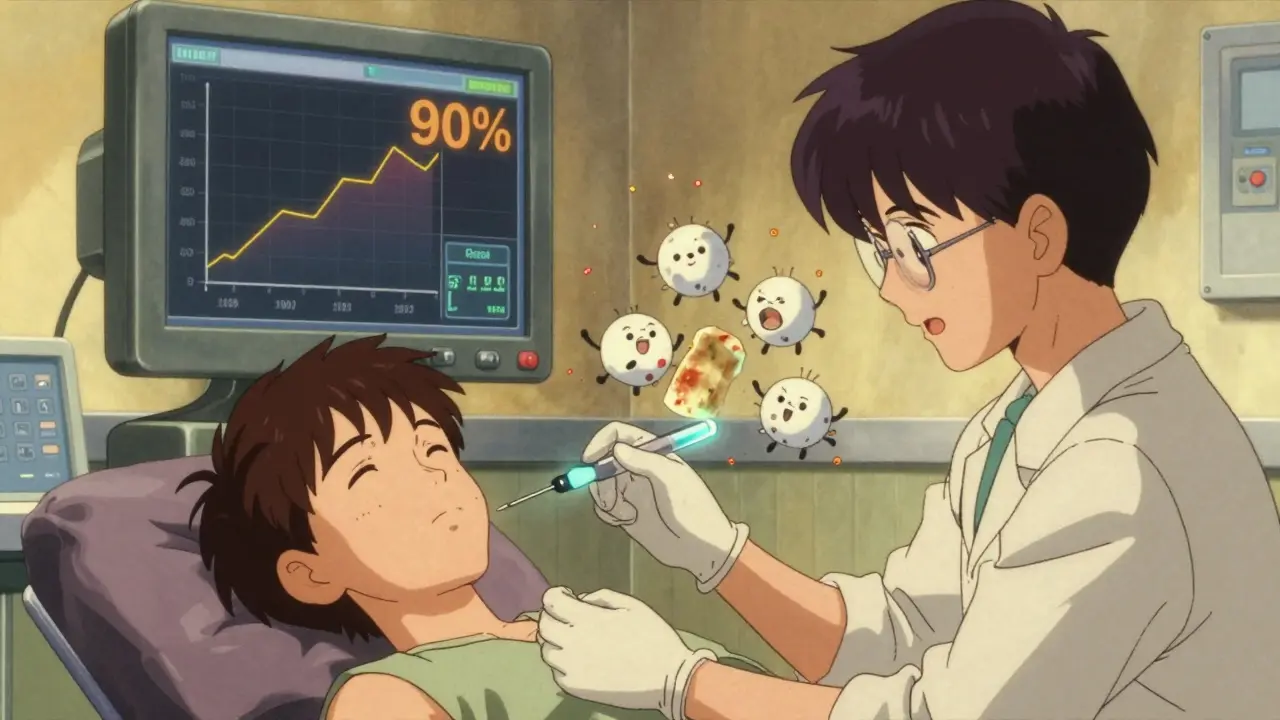
Who Can Skip Testing?
Not everyone needs testing. The CDC and other experts have created clear risk categories:- Low-risk patients: Those with only gastrointestinal symptoms (nausea, diarrhea), headaches, or a mild rash that happened more than 5 years ago. These people can often take first-generation cephalosporins like cefazolin without testing. No need to panic.
- Moderate-risk patients: Those with hives, swelling, or breathing issues within the last 5 years. These people should be referred for testing before any beta-lactam antibiotic is given.
- High-risk patients: Those with recent anaphylaxis, SJS, TEN, or organ damage. These patients should avoid all penicillin and related drugs unless evaluated by an allergist.
What You Should Do Right Now
If you’ve been told you’re allergic to penicillin:- Check your medical records. Does it say "penicillin allergy" with no details? That’s probably a mistake.
- Think back. Did you have a rash? When? Was it itchy? Did you have trouble breathing? Did you need epinephrine? If you’re not sure, it’s likely not a true allergy.
- Ask your doctor: "Can I be tested for a penicillin allergy?" Most primary care clinics and pharmacies now offer this service.
- If you’ve had a reaction in the past 5 years, ask for a referral to an allergist.
- Don’t assume you’re allergic forever. Even if you had a real reaction 15 years ago, your body may have forgotten.
What to Do in an Emergency
If you ever have symptoms like swelling of the face or throat, trouble breathing, or a sudden drop in blood pressure after taking any antibiotic, call 911 or go to the ER immediately. Don’t wait. Anaphylaxis can kill within minutes. If you’ve had a serious reaction before, wear a medical alert bracelet. Make sure your family, friends, and doctors know your history. But if you’re unsure, don’t assume-you might be safer than you think.
The Bigger Picture
This isn’t just about one drug. It’s about how we use antibiotics. Mislabeling penicillin allergies leads to overuse of broad-spectrum drugs, which fuels the rise of superbugs. Hospitals that have implemented formal penicillin allergy de-labeling programs have removed incorrect labels from 80-90% of eligible patients. In orthopedic surgery, testing just 112-124 patients with false penicillin allergies prevents one surgical infection. By 2025, half of U.S. hospitals plan to have formal penicillin allergy assessment programs. That’s progress. But it starts with you. If you’ve been told you’re allergic, don’t live with that label unless you know it’s true. Get tested. Save yourself. Save others.What Happens After Testing?
If your test is negative, your doctor should update your medical record to say "penicillin allergy ruled out" or "no true allergy." You should get a written note to keep with your records. Some clinics even give you a card to carry in your wallet. And if you need penicillin in the future-whether for a sinus infection, strep throat, or a surgical procedure-you can take it with confidence. You’re not just avoiding side effects. You’re helping fight antibiotic resistance.Can I outgrow a penicillin allergy?
Yes. About 80% of people who had an IgE-mediated penicillin allergy lose their sensitivity after 10 years without exposure. Even if you had a serious reaction as a child, you may no longer be allergic. Testing is the only way to know for sure.
Are cephalosporins safe if I’m allergic to penicillin?
For most people, yes. Third- and fourth-generation cephalosporins like ceftriaxone and cefdinir are considered safe even for those with penicillin allergies-unless they’ve had a severe IgE-mediated reaction. First-generation cephalosporins like cefazolin are also safe for low-risk patients. Testing is still recommended for moderate-risk cases.
What if I had a rash as a child but never got tested?
That’s one of the most common reasons for false allergy labels. A simple rash, especially without breathing problems or swelling, is rarely a true allergy. Most people in this situation can safely undergo skin testing and oral challenge. You’re likely not allergic anymore-or never were.
Can I take amoxicillin if I’m allergic to penicillin?
Amoxicillin is a type of penicillin. If you have a true penicillin allergy, you should avoid it. But if you’ve been mislabeled, an oral challenge with amoxicillin under medical supervision is the gold standard for testing. Most people who pass the challenge can take amoxicillin safely for life.
Is penicillin allergy testing covered by insurance?
In the U.S., most insurance plans cover penicillin allergy testing when ordered by a doctor. In the UK, it’s typically available through NHS allergy services. Ask your provider or pharmacist-they can help you find a clinic that offers the test at low or no cost.
Next Steps for Patients
If you’re unsure about your allergy status:- Review your medical records. Look for details about your reaction-not just "penicillin allergy."
- Call your doctor’s office. Ask if they offer penicillin allergy testing or can refer you to an allergist.
- Check with your local pharmacy. Some now offer supervised oral challenges.
- If you’re scheduled for surgery, ask if your allergy label can be reviewed before the procedure.
- Update your records. Once tested, make sure your allergy status is corrected in all your medical files.







Wow I had no idea most people labeled penicillin allergic aren't really allergic. My mom got a rash as a kid and we just assumed she was allergic forever. Guess we should get her tested.
People are so careless with medical labels I swear it's like they dont even care if they die from a wrong antibiotic
Testing is easy. Talk to your doctor. Do it.
Bro this is wild. I thought I was allergic because I got sick once. Turns out I just had food poisoning. My bad.
In India we dont even have access to these tests. Why should Americans get all the fancy healthcare while we struggle just to get basic meds?
OMG I just realized I’ve been living with this label since I was 5 😱 I got a rash after amoxicillin and my mom freaked out. Now I’m 34 and never tried again. I’m gonna book a test ASAP. This post changed my life lol ❤️
It’s so important to question labels we accept without thinking. Most of us don’t realize how much our assumptions affect our health. This is a quiet revolution in medicine.
MY GOD I’M ONE OF THOSE PEOPLE. I WAS TOLD I WAS ALLERGIC AT 7. I HAD A RASH. NO SWELLING. NO TROUBLE BREATHING. I’M GETTING TESTED TOMORROW. THANK YOU FOR THIS. I’M SO RELIEVED.
So what you're saying is we're being manipulated by lazy doctors who don't want to think? Classic. They just say 'allergy' and move on. I'm not surprised. The system is broken.
Just get tested if you’re unsure. Stop being dramatic.
Here’s the thing no one talks about - most people who say they’re allergic never even saw a doctor. They just stopped taking it because they felt weird. Then it becomes a ‘fact’ in their chart. We need to stop letting fear drive medical decisions.
I wonder how many people died because doctors were too scared to use penicillin. This feels like a silent epidemic. We’re so afraid of side effects we ignore the real danger.
I’m from the U.S. but my mom’s from Nigeria, and in her village, they just didn’t have the luxury of testing. People took what was available - even if it wasn’t ideal. It makes me think: maybe this problem isn’t just about ignorance, but about inequality. In places where antibiotics are scarce, mislabeling becomes a survival tool. We’re lucky here. But not everyone is. We need to push for global access to testing, not just in rich countries. This isn’t just a medical issue - it’s a justice issue.