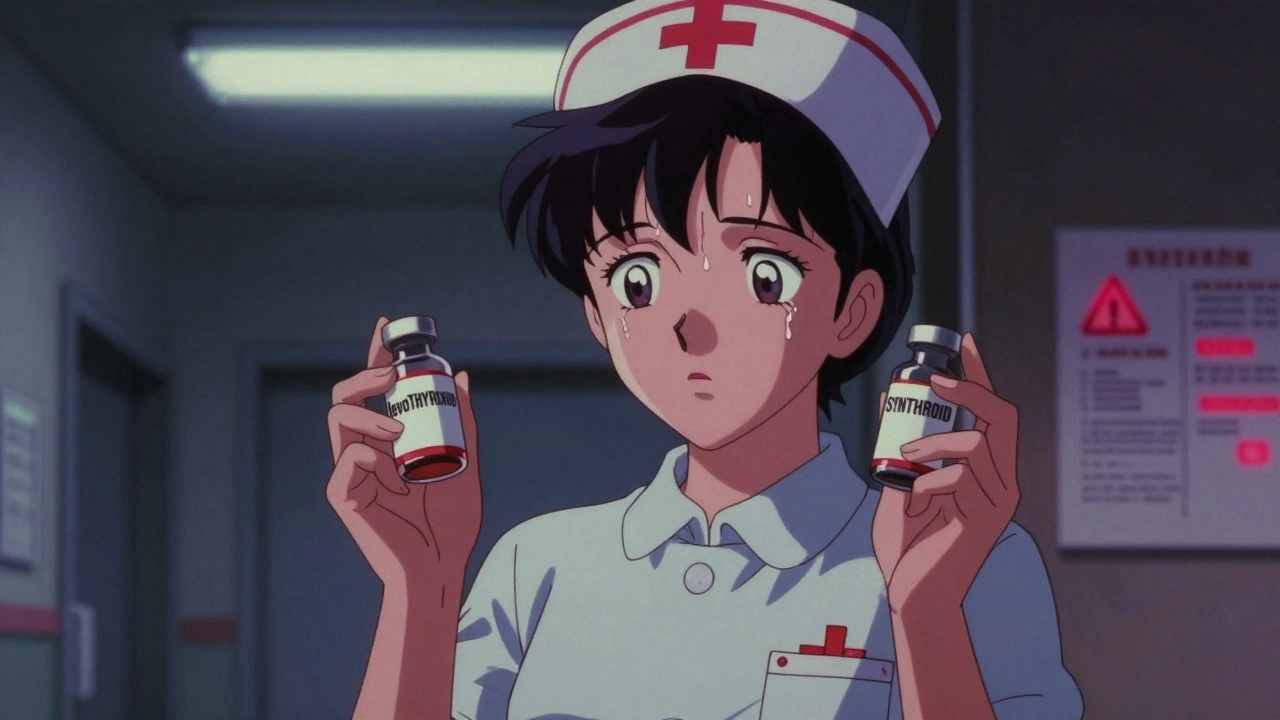
Imagine this: you’re a nurse on a late-night shift. A doctor says, "Give the patient the thyroid med." You grab the vial labeled levoTHYroxine-but it’s actually SYNTHROID. Both look identical. Both are used for hypothyroidism. You almost give it. You catch it at the last second. That’s not a rare mistake. It’s a daily risk in hospitals and pharmacies across the UK and beyond.
These aren’t just typos or slips. They’re look-alike, sound-alike (LASA) medication errors-errors caused by names, packaging, or appearance that are too similar. And they’re one of the biggest hidden dangers in healthcare today. One in four medication errors in the U.S. is linked to drug name confusion. In the UK, the NHS reports similar patterns. These aren’t hypothetical risks. They’re real, preventable mistakes that lead to overdoses, underdoses, and even death.
How LASA Errors Happen
It’s not just about spelling. LASA errors come in four forms:
- Orthographic (look-alike): Names that look too similar on paper or screen. Like HYDROmorphone and hYDROcodone. The capital letters help, but if you’re rushing, you might miss them.
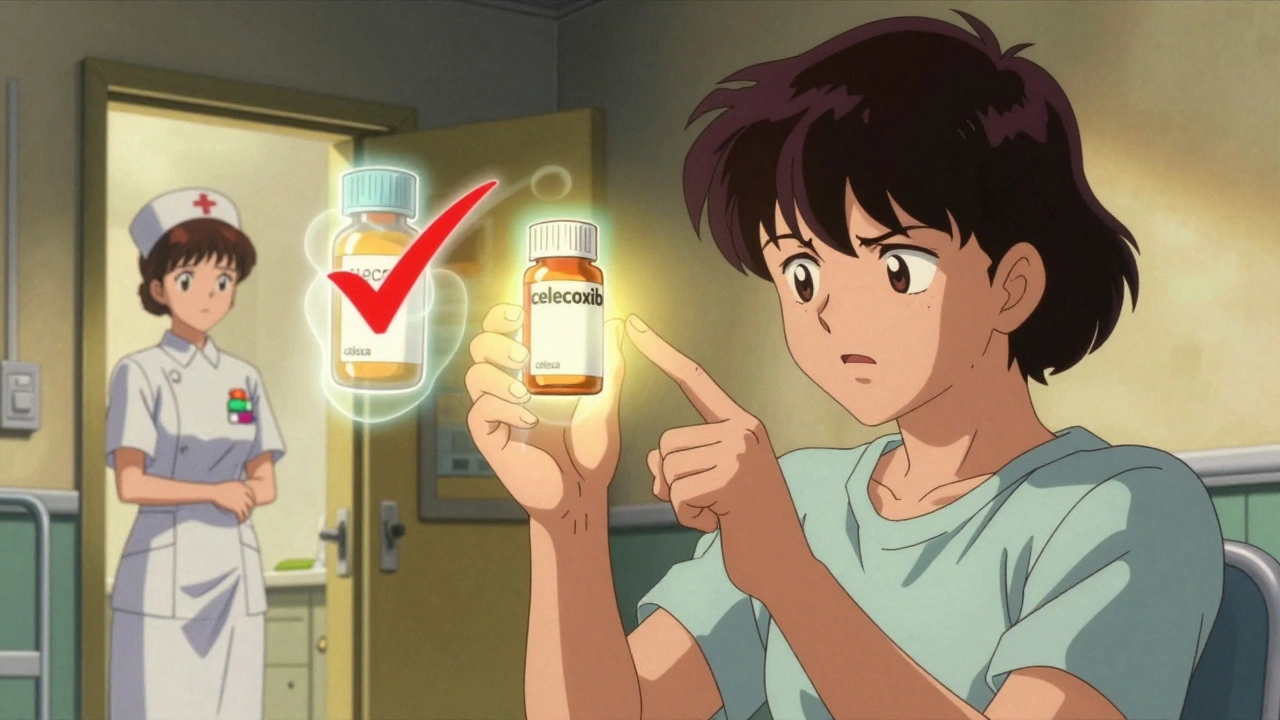
- Phonetic (sound-alike): Names that sound alike when spoken. Think velcade and velcade-wait, no, that’s the same. But velcade and velcade aren’t the issue. The real problem is celecoxib and celexa. One’s for arthritis. The other’s an antidepressant. Say them fast. They blur.
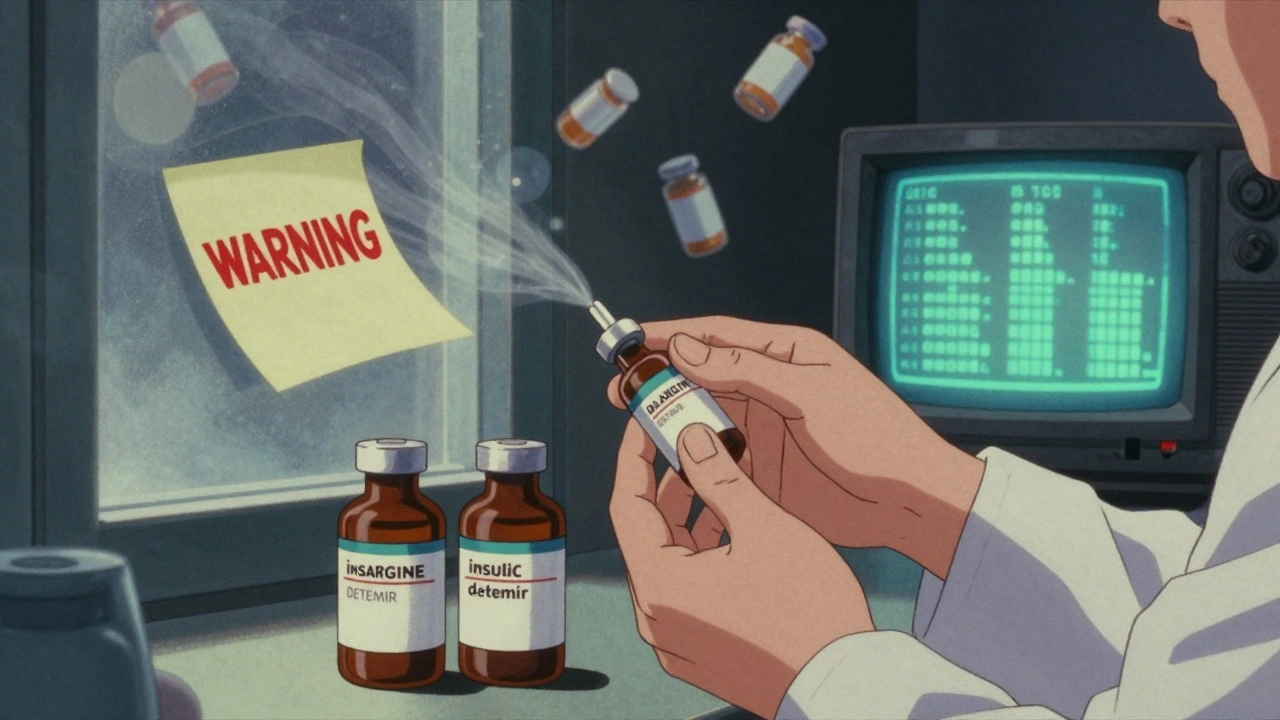
- Packaging: Two drugs in nearly identical bottles. Same color. Same font size. Same label layout. A pharmacist in Manchester told me, "I’ve pulled the wrong insulin vial three times because the labels were mirror images. I didn’t even notice until I held it up to the light."
- Physical appearance: Pills that look the same. A 10mg simvastatin tablet and a 20mg version? Identical color, shape, size. Only the number on it tells the difference. And if you’re tired? You skip reading it.
The most dangerous pairs? Chemotherapy drugs like doxorubicin and daunorubicin. One wrong dose can kill. Or insulin glargine and insulin detemir. Both are long-acting. Both look the same. But they’re not interchangeable. A 2022 study found that drug name confusion alone caused over 64% of LASA errors in hospitals.
Why This Keeps Happening
You’d think we’d have fixed this by now. We’ve had warnings for decades. The FDA started using tall man lettering in 2001-capitalizing parts of names to make them stand out. cisPLATIN vs. caraPLATIN. HYDROmorphone vs. hYDROcodone. It sounds smart. But here’s the truth: it doesn’t work as well as people think.
A 2022 review found tall man lettering creates a "quasi-placebo effect." Nurses and pharmacists know it’s supposed to help-but if they’re not trained to look for it, they don’t see it. One pharmacist in Leeds said, "I’ve been using EHRs for 12 years. I’ve seen tall man letters every day. But when I’m swamped at 3 a.m., I still glance at the name and assume it’s right."
And then there’s the system. New drugs keep getting approved with names that are too close to existing ones. In 2022, the FDA rejected 34 new drug names just because they were too similar to others. That’s up from 22 in 2018. But the process is slow. And in the meantime, dangerous pairs stay on shelves.
High-alert medications make it worse. Insulin, opioids, anticoagulants, neuromuscular blockers-these drugs have narrow safety margins. One mistake, and you’re in the ER. Or worse. The FDA’s MAUDE database recorded 128 deaths linked to LASA errors between 2018 and 2022. That’s not a statistic. That’s 128 families who lost someone because two drug names looked too similar.
Real Stories from the Frontline
Online forums like Reddit’s r/nursing are full of near-misses. One nurse wrote: "I almost gave vecuronium instead of versed in the ICU. One’s a paralytic. The other’s a sedative. If I’d given vecuronium, the patient would’ve stopped breathing. I caught it because I double-checked the vial after the label smudged."
An oncologist in Manchester shared: "We have 17 chemo drugs that look like each other. I’ve had residents pick the wrong one three times in a month. We now put color-coded stickers on all chemo vials. It’s not perfect, but it’s helped."
And it’s not just hospitals. Community pharmacies are just as vulnerable. A 2023 survey found 78% of physicians had encountered a LASA-related near-miss in the past year. Oncologists? 92%. That’s not a fluke. That’s a system under pressure.
What’s Being Done
Some places are fighting back-with real results.
- Electronic prescribing systems like Epic’s SafeMed module now flag LASA pairs automatically. In a 12-hospital study, they cut errors by 28.7%.
- Movable signage in pharmacies-sticky notes with bold warnings placed right next to high-risk drugs. Simple. Cheap. Effective.
- AI voice recognition is being tested at Johns Hopkins. It listens to verbal orders and alerts staff if a drug name sounds too close to another. Early results? 89.3% accuracy.
- Annual LASA lists are now required by the Joint Commission. But here’s the catch: every hospital must make their own. You can’t copy a list from another facility. Your pharmacy’s formulary is unique. Your risks are unique.
Training matters too. ASHP recommends 2-4 hours of annual education for all staff. For oncology or ICU teams? Add another 1-2 hours every quarter. But not every hospital does it. Smaller clinics? Only 38% have full LASA protocols. Big hospitals? 72%. That gap kills.
What You Can Do
If you’re a patient, you’re not powerless.
- Always ask: "What is this medicine for?" If the answer is vague, dig deeper.
- Check the label. Is it the right name? Right strength? Right color? Don’t assume.
- If you’re on insulin, anticoagulants, or chemo-ask your pharmacist to show you the difference between similar drugs. Take a photo of the label.
- Speak up. If you think something’s wrong, say it. Even if you’re not sure.
If you’re a healthcare worker:
- Use the "read-back" rule. When someone gives you a verbal order, repeat it back word for word. "You said 5mg of hydromorphone? Confirm?"
- Never rely on memory. Even if you’ve given a drug 100 times, check the label every time.
- Advocate for your hospital to update its LASA list. If you see a dangerous pair on the shelf, report it.
- Use color coding. Put a red dot on high-risk vials. Make it impossible to miss.
The Future
The FDA is pushing for mandatory testing of all new drug names using algorithms based on the 1999 Lesar study-ones that predict confusion risk before a drug even hits the market. That’s huge. If adopted, it could stop new problems before they start.
The WHO wants global standards by 2030: universal design rules for drug names and packaging. No more identical bottles. No more confusing names. Just clarity.
And AI? It’s not magic. But it’s getting better. Voice recognition systems that catch errors in real time? They’re coming. And they’ll be cheaper than hiring extra staff.
But here’s the bottom line: technology won’t fix this alone. People will. The nurse who double-checks. The pharmacist who speaks up. The doctor who writes clearly. The patient who asks questions.
Look-alike, sound-alike errors aren’t going away. But they can be stopped. One label. One question. One pause. One moment of attention.
That’s how you save a life.






OMG I’ve seen this so many times in my hospital in Delhi 😭 One time I almost gave Clonidine instead of Clonazepam to a kid-both look identical, same bottle, same font. Thank god I glanced at the script again. We started using color-coded stickers after that. Now every high-risk med has a neon yellow dot. It’s stupid simple but it works. Why isn’t this mandatory everywhere??
There are multiple grammatical errors in this post. ‘HYDROmorphone’ and ‘hYDROcodone’ should be capitalized consistently. Also, ‘velcade’ is repeated incorrectly-likely a copy-paste error. And ‘EHRs’ needs to be spelled out on first use. This is a serious topic; sloppy writing undermines credibility.
This whole thing is just lazy healthcare. If you can’t read a label properly, maybe you shouldn’t be handling drugs. Stop blaming the names and start training your staff. We don’t need AI voice recognition-we need people who pay attention. 128 deaths? Probably half of them were from people who didn’t bother to look.
As someone who works in pharmacovigilance in Boston, I’ve reviewed over 300 LASA incident reports in the last five years. The most insidious cases aren’t the obvious ones like insulin vs. insulin-they’re the ones where the packaging is identical, the spelling is nearly the same, and the dosing is subtly different. For example: gabapentin vs. gabapentin enacarbil. One’s for seizures. The other’s for restless legs. Same root. Same manufacturer. Same color. The only difference? A single syllable. And yes, people mix them up. Constantly. We need mandatory phonetic similarity scoring for all new drug names-like the FDA does for trademarks. It’s not rocket science.
And tall man lettering? It’s a band-aid. We’ve known since 2005 that cognitive load in high-stress environments overrides visual cues. What we need is auditory confirmation systems integrated into EHRs-where the system speaks the drug name aloud before dispensing. That’s the future. Not stickers. Not training slides. Real-time, multi-sensory verification.
Also-why is no one talking about the role of generic naming conventions? The FDA allows manufacturers to submit names that are phonetically indistinguishable from existing drugs, as long as they’re not exact matches. That’s a loophole. A dangerous one. We need a global naming authority. Not just recommendations. Enforcement.
And patients? You’re right to ask questions. But don’t just ask ‘what is this for?’ Ask ‘how is this different from the last pill I took?’ That’s the question that saves lives.
My aunt almost died because of this. She was on warfarin, got a new script for warfarin sodium-same thing, different name, same bottle. The pharmacist didn’t catch it. Neither did the nurse. She ended up in the ER with a bleeding ulcer. We had to fight for weeks to get her care covered. I’ve been pushing my local clinic to put up warning signs next to anticoagulants ever since. It’s not hard. It’s just not prioritized. We treat these errors like accidents. They’re not. They’re systemic failures. And we’re all paying for it.
Let’s be real: the real problem isn’t the names-it’s the speed. Nurses are running on fumes. Pharmacists are juggling 200 scripts an hour. Doctors are typing orders while on Zoom calls. We’ve turned healthcare into a factory, and people are the cogs. No amount of AI or color coding will fix that. We need fewer patients per nurse. More breaks. More staffing. More respect. The rest? Just bandaids on a hemorrhage.
Also-why do we still allow drugs like ‘Zyrtec’ and ‘Zyrtec-D’ to exist? One’s antihistamine. The other’s antihistamine + decongestant. The ‘D’ is tiny. I’ve seen people take both and end up in the ER with hypertension. It’s not a LASA error-it’s a branding disaster.
Love this post! I work in a rural pharmacy in Kerala, and we don’t have fancy EHRs. But we use handwritten warning tags on every high-risk med. We write ‘DANGER: CONFUSES WITH’ in big red letters. It’s old-school, but our error rate dropped by 60% in 18 months. Also, we started having a 30-second ‘med check huddle’ before shift change-everyone says out loud the top 3 high-risk meds they’re dispensing. It sounds silly, but it works. Simple fixes, big impact.
Been a nurse for 17 years. Seen it all. The system’s broken. No one’s fixing it. Just keeps getting worse.
AI voice recognition is not ready for clinical use. False positives will cause more delays than errors. Stick to human verification.
My dad’s a retired pharmacist in Ohio. He says the real solution? Ban generic names that sound like brand names. Why does ‘Lisinopril’ sound so close to ‘Lisinopril-HCTZ’? It’s not an accident. It’s marketing. And we’re the ones who pay the price. I told him he’s too old to care. He said, ‘No, honey. I’m old enough to remember when we didn’t have this problem.’ He’s right. We lost the plot.