What Is Tendinopathy, Really?
Tendinopathy isn’t just a sore tendon. It’s a broken-down tendon that’s lost its normal structure and can’t handle load the way it used to. You don’t get it from one bad move-you get it from too much repetitive stress over time. Runners, basketball players, and even office workers typing all day can end up with it. The most common spots? The Achilles tendon at the back of the ankle, the patellar tendon below the kneecap, and the rotator cuff tendons in the shoulder. Pain is the main symptom, but swelling, stiffness, and weakness follow close behind. It’s not inflammation like people used to think-it’s degeneration. That’s why anti-inflammatories don’t fix it long-term.
Why Eccentric Training Works When Nothing Else Does
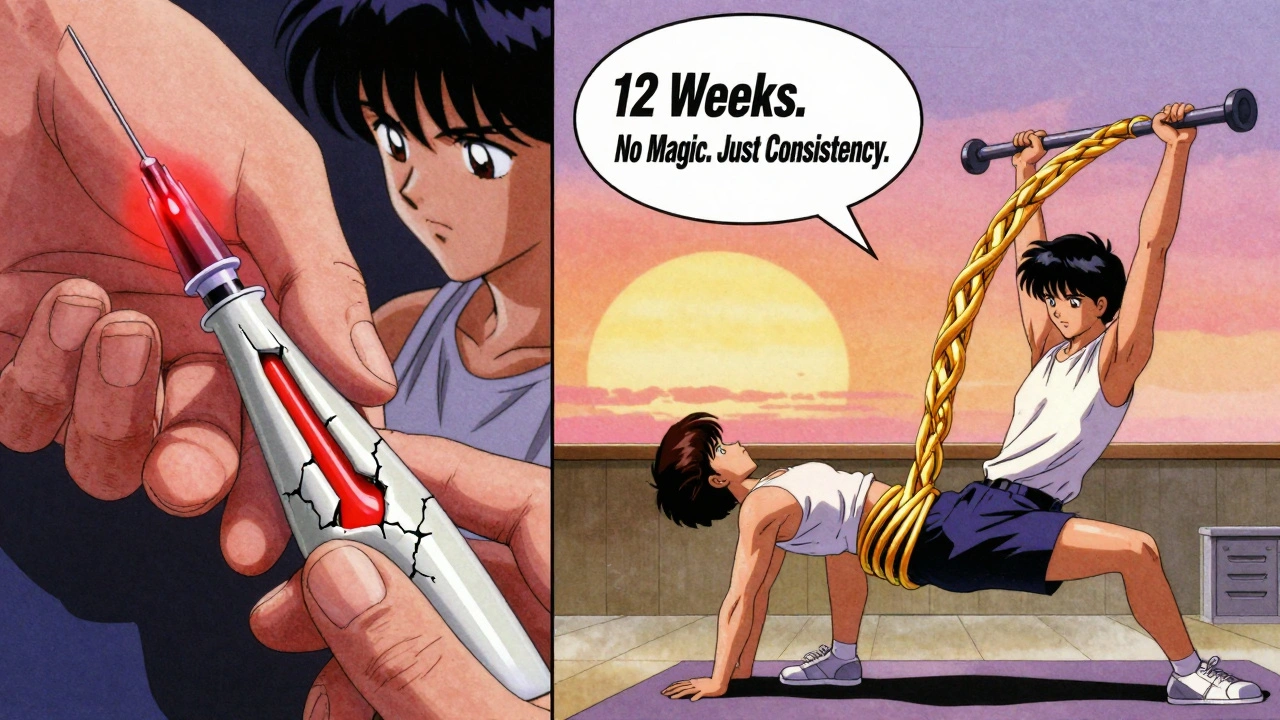
For over 25 years, eccentric training has been the gold standard for treating tendinopathy. It’s not just another exercise-it’s a targeted mechanical signal that tells your tendon to rebuild itself. Eccentric means lengthening under tension. Think of slowly lowering yourself during a heel drop or a squat. That controlled descent creates the exact kind of stress your tendon needs to start repairing. Studies show it increases collagen alignment, improves tendon stiffness by 15-20%, and reduces pain by 40-50% over 12 weeks. The key isn’t just doing the movement-it’s doing it right, with enough load and enough time.
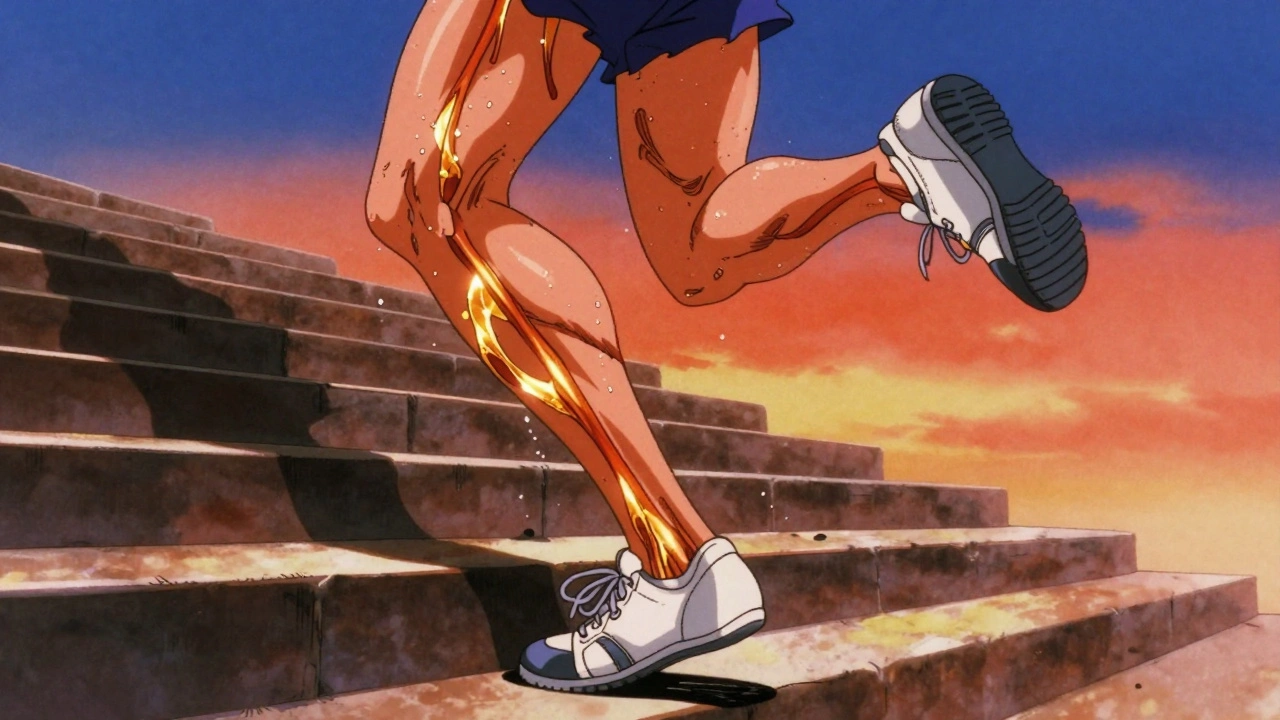
How to Do Eccentric Training for Achilles Tendinopathy
Alfredson’s protocol is the most researched method for Achilles tendinopathy. You stand on the edge of a step, lift up on both feet, then lower down slowly on just the affected leg. Do it with your knee straight to target the gastrocnemius, then bend your knee slightly to hit the soleus. Three sets of 15 reps, twice a day, seven days a week. Sounds simple? It’s not. Most people rush the lowering phase. You need to take 3-5 seconds to drop down. Pain during the exercise is normal-aim for a 5-7 out of 10. If it’s worse than that, or if pain lasts more than 24 hours, you’re pushing too hard. Stick with it for at least 12 weeks. That’s how long it takes for new collagen to form. A 2021 study found that 82% of runners who completed this protocol returned to their previous running levels.
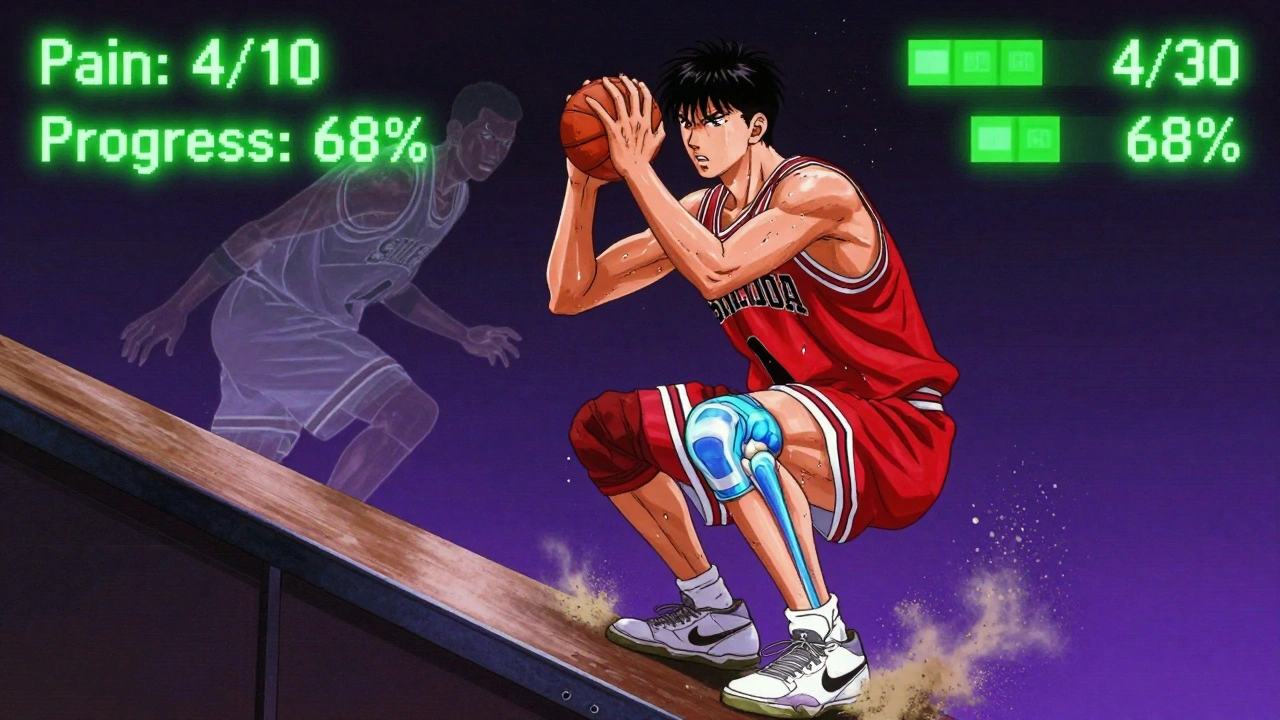
How to Do Eccentric Training for Patellar Tendinopathy
For the kneecap tendon, the go-to exercise is the single-leg decline squat. You stand on a 25-degree angled board, holding onto something for balance, and slowly lower yourself down over 3-5 seconds. Keep your knee aligned over your toes. Do three sets of 15 reps daily. The decline angle increases the load on the patellar tendon, making the exercise more effective than regular squats. Many people struggle with form-knees caving in, leaning too far forward. That’s why working with a physical therapist for the first two sessions makes a big difference. Self-managed patients make mistakes 40% more often, according to a BMC Sports Science study. Apps like Tendon Rehab with real-time feedback boost adherence from 65% to 85%.
Heavy Slow Resistance: A Strong Alternative
Heavy slow resistance (HSR) training is gaining ground as an equal-or sometimes better-option than traditional eccentric training. Instead of doing high-rep, low-load eccentric moves, you lift heavier weights slowly. For example, leg press or seated calf raises at 70% of your one-rep max, with 3 seconds up and 3 seconds down. Three times a week. Beyer et al.’s 2015 study found HSR improved Achilles tendinopathy scores just as much as eccentric training-but with better adherence. Why? Less pain at the start. Only 15% of HSR users quit due to pain, compared to 28% in eccentric groups. For people who can’t tolerate the initial burn of Alfredson’s heel drops, HSR is a viable path. It’s also easier to track progress with weights, making motivation simpler.
Isometric Holds: The Quick Pain Fix
Isometric exercises aren’t meant to rebuild your tendon-they’re meant to quiet the pain right now. If you need to play a game, go to work, or even just walk without limping, try holding a static contraction. For the Achilles, stand on both feet and press up into a calf raise, then hold at the top for 45 seconds. For the knee, sit with your leg straight and squeeze your quad hard for 45 seconds. Do five sets. Rio et al.’s 2015 study showed a 50% drop in pain within minutes. That’s not placebo-it’s neurological. Isometrics temporarily reduce pain signals from the tendon, giving you a window to move better. Use them before activity, not instead of eccentric training.
Injection Options: What Actually Helps?
Corticosteroid injections give fast relief-30-50% pain reduction in four weeks. But they’re a trap. They weaken the tendon long-term. A 2013 BMJ study found 65% of people who got steroid shots needed more treatment within six months. Only 35% of those who stuck with exercise did. Platelet-rich plasma (PRP) sounds fancy, but the data doesn’t back it up. A 2020 review in the American Journal of Sports Medicine showed PRP only beat placebo by 15-20% at six months. That’s not enough to justify the cost or the risk. Ultrasound-guided dry needling has shown modest benefit in some studies, but it’s not a magic bullet. Injections should never be your first choice. They’re for when exercise hasn’t worked after 12 weeks-or for people who can’t commit to rehab due to time or pain.
Why Most People Fail at Eccentric Training
It’s not the exercise. It’s the mindset. Most people expect quick results. They do it for two weeks, feel no change, and quit. But tendon remodeling takes 8-12 weeks. You won’t feel better until then. Another big mistake? Avoiding pain entirely. Tendons need stress to heal. The goal isn’t pain-free-it’s controlled pain. A 2022 survey showed only 38% of self-managed patients understood what “acceptable pain” meant (2-5/10 during exercise). Anything above 7/10 or lasting over 24 hours? That’s too much. Also, skipping warm-ups or not using proper form cuts effectiveness. A 2023 Journal of Athletic Training study found 92% of people who worked with a therapist succeeded, compared to just 68% who went it alone.
Real People, Real Results
On Reddit’s r/PhysicalTherapy, one user wrote: “I did 12 weeks of heel drops. Week 1-3? Pure torture. Week 8? I could walk without limping. Week 12? I ran a 10K.” That’s not rare. A 2021 survey of 452 runners with Achilles tendinopathy found 82% returned to their prior activity level after eccentric training. In contrast, only 58% of those who got steroid injections did. People who succeeded consistently said three things: they stuck with it, they tracked progress, and they didn’t quit when it hurt. One user on TendonTalk said: “My ultrasound showed my tendon thickened after three months. That was the moment I knew it was working.”
What’s Next for Tendinopathy Treatment?
The field is moving beyond one-size-fits-all protocols. Researchers are now testing load tolerance assessments to personalize how much stress a tendon can handle. A 2022 study showed this approach improved outcomes by 25%. There’s also growing interest in combining eccentric training with psychological support-because chronic pain isn’t just physical. Phase II trials for a new peptide called TAP-421, designed to activate tendon cells, start in early 2024. But for now, the best tool remains movement. Eccentric training, done right, is still the most proven, safest, and most cost-effective method. It doesn’t need a prescription. Just consistency.
How to Start Today
- Identify your tendon: Achilles? Patellar? Shoulder?
- Choose your protocol: Alfredson for Achilles, decline squats for patellar.
- Start with 3 sets of 15 reps, twice a day.
- Lower slowly-3 to 5 seconds.
- Keep pain between 2-5/10 during exercise.
- Do it every day for at least 12 weeks.
- Use an app like Tendon Rehab for form feedback.
- If pain spikes above 7/10 or lasts more than 24 hours, reduce load or rest one day.
- Consider isometric holds before activity for quick relief.
- Seek a physical therapist if you’re unsure about form.
Frequently Asked Questions
How long until I see results from eccentric training?
Most people start noticing less pain around week 6-8, but real structural changes take 12 weeks. Tendons heal slowly. Don’t stop early-even if you feel better at week 4, you haven’t rebuilt the tendon yet. Studies show you need at least 12 weeks of consistent training to get lasting results.
Can I still run or play sports while doing eccentric training?
Yes, but you need to manage your load. Don’t go back to full intensity right away. Reduce your mileage or training volume by 30-50% while you do the exercises. Use isometric holds before activity to reduce pain. If pain spikes during or after activity, you’re doing too much. Listen to your tendon, not your ego.
Are injections better than exercise?
No. Injections like corticosteroids give short-term relief but weaken the tendon over time. A 2013 BMJ study found 65% of people who got steroid shots needed more treatment within six months. Only 35% of those who did eccentric training did. PRP has little proven benefit over placebo. Exercise rebuilds the tendon. Injections just mask the pain.
What if eccentric training doesn’t work for me?
About 30% of people don’t respond to standard eccentric protocols. That doesn’t mean you’re broken-it means your tendon needs a different approach. Try heavy slow resistance training instead. Or combine isometrics with eccentric work. Some people benefit from shockwave therapy or dry needling. If nothing works after 16 weeks, see a specialist. There are new treatments in trials, like TAP-421 peptides, coming soon.
Do I need an ultrasound to confirm tendinopathy?
Not always. A good physical exam by a sports therapist can diagnose it accurately. But if pain doesn’t improve after 8 weeks of proper exercise, an ultrasound can show if the tendon structure has changed-like thickening or disorganized collagen. That’s useful for tracking progress and staying motivated.






Just started Alfredson heel drops last week 😅 I thought I was gonna cry every time, but week 2? My ankle actually feels less stiff in the morning. Keep going, it’s worth the sucky days.
Been doing HSR for 8 weeks now. Less pain than eccentric, way easier to track progress with weights. I went from 40kg leg press to 85kg without a single flare-up. If you hate the burn of heel drops, this is your lifeline.
People treat tendons like they’re broken glass that needs to be handled gently. Nah. Tendons are ropes. You don’t fix a rope by whispering to it. You load it. Slowly. Consistently. Until it gets stronger. Stop fearing pain. Fear stagnation.
Ugh. Why do people still believe in 'eccentric training' like it's some holy grail? I did 12 weeks of heel drops, then got PRP and now I'm pain-free. The study they cited? Funded by PT associations. 🤡
PRP is just a placebo wrapped in a fancy lab coat. They pump your blood, charge you $1500, and say 'your body heals itself!' But your body was already trying. You just didn't give it time. The real conspiracy? The medical industry profits more from injections than rehab.
There’s something deeply poetic about the idea that healing isn’t about magic bullets-it’s about showing up, day after day, with a body that feels broken. Tendons don’t care about your hustle culture. They don’t respond to willpower. They respond to repetition. To patience. To the quiet, unglamorous act of lowering yourself slowly, again and again, even when you don’t feel like it. That’s not exercise. That’s devotion.
I used to think recovery was about fixing something broken. Now I think it’s about learning to listen. To the creak. To the ache. To the silence between the reps. The tendon doesn’t scream. It whispers. And most of us are too loud to hear it.
That’s why the 82% who succeeded didn’t just follow a protocol. They changed their relationship with pain. They stopped seeing it as the enemy. They saw it as feedback. As a conversation. And that shift? That’s the real treatment.
eccentric training is just government mind control disguised as physical therapy. they want you to do 15 reps twice a day so you dont have time to think about the truth. the real cure is cold laser and magnets. the studies? paid for by big physio. also, i heard the 12 week thing is a scam. your tendon needs 18 weeks. or 24. depends on the moon phase.
I tried the decline squats. My knee felt like it was being shredded. Did it for 6 weeks. No change. Then I switched to isometrics before runs. Just 45 second holds. Pain dropped from 7/10 to 2/10 instantly. Still do it. No eccentric. Just hold. That’s it.
PRP has no statistically significant benefit over saline placebo at 6 months. The BMJ study on steroid injections showed 65% recurrence. HSR has higher adherence. Eccentric training has the most robust long-term data. Stop listening to anecdotal influencers. Stick to the evidence.
In India, we’ve been doing barefoot heel drops on stone steps for generations. No apps. No fancy gear. Just bodyweight, patience, and a cup of chai after each set. The science confirms what our grandmas knew: movement is medicine. No injection needed.
They say 'stick with it for 12 weeks.' But what if your tendon doesn't want to heal? What if it's screaming for rest? What if the real problem isn't your training-it's your soul? You can't force a tendon to rebuild when your life is falling apart. The system doesn't care. It just wants you to do more reps. But maybe... maybe you need to stop. Not because you're weak. Because you're human.