When a drug gets recalled, it’s not just a notice on a website-it’s a race against time to keep patients safe. If your pharmacy handles prescriptions, you need to know how to check for pharmacy-level recall notifications before someone walks out with a dangerous medication. This isn’t optional. It’s required by law. And if you’re waiting for a letter in the mail, you’re already behind.
Why Pharmacy-Level Recall Notifications Matter
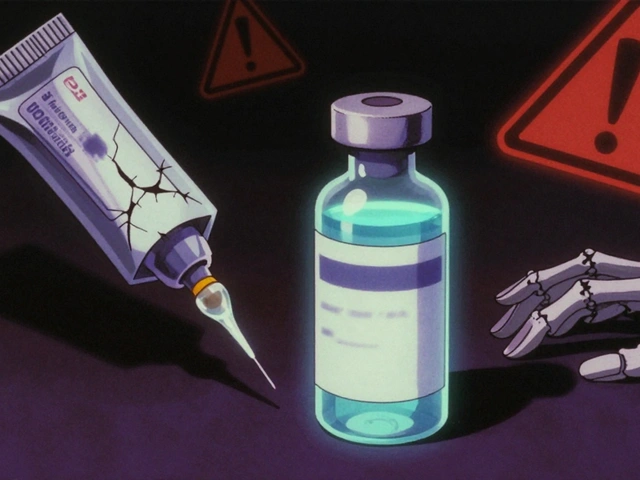
Every year, thousands of medications are pulled from shelves because of contamination, mislabeling, or dangerous impurities. In 2023 alone, the FDA issued over 4,200 drug recalls. Most were Class II-meaning the product might cause temporary or medically reversible harm. But 4% were Class I, where use could lead to serious injury or death. And for those? You have 24 hours to act. Pharmacies are on the front line. A single missed recall can mean a patient gets a batch of metformin with unsafe nitrosamine levels, or a blood pressure pill with the wrong active ingredient. The consequences aren’t theoretical. In 2022, a Class I recall of losartan went undetected in a small independent pharmacy for 72 hours. The patient suffered a stroke. That’s why the FDA, CMS, and ASHP all require pharmacies to have systems in place-not just one, but multiple.Where Recall Notifications Come From
You can’t rely on just one source. The FDA doesn’t send you a text. Wholesalers don’t always call. Here are the five real channels that deliver recall alerts to pharmacies:- FDA MedWatch email alerts - Free, but you have to sign up. Updates are posted every Wednesday, but emails go out within hours of new recalls being classified.
- Wholesaler notifications - McKesson, Cardinal Health, and AmerisourceBergen send alerts directly to contract pharmacies. These are mandatory under FDA rules. 82% of independent pharmacies use these.
- Pharmacy management systems - QS/1, PioneerRx, FrameworkLTC, and others pull FDA data hourly. They auto-match NDC and lot numbers to your inventory. This is the gold standard.
- Direct manufacturer emails - Sometimes, the drugmaker sends a notice directly to your pharmacy. Don’t ignore these. They’re often faster than the FDA.
- FDA Enforcement Reports - Published weekly, these are the official public record. But they’re not real-time. Use them for backup, not primary alerts.
The biggest mistake? Relying on one channel. A 2023 University of Florida study found that pharmacies using only mail or fax missed 28% of Class I recalls. Email alerts had a 98.7% delivery rate-but only 62% of pharmacists actually checked them in time. Integrated systems? 99.2% delivery, 89% acknowledgment.
How to Set Up Your Recall Notification System
If you’re not already set up, here’s what to do-right now.- Register for FDA MedWatch - Go to www.fda.gov/Safety/MedWatch. Create an account. Select "Drug Recalls" under email preferences. You’ll get alerts within minutes of a new Class I recall.
- Confirm your wholesaler’s recall system - Call your distributor. Ask: "Do you send automated recall alerts? How do I enroll?" Most are free. If they say "we just mail it," demand a better system.
- Enable recall alerts in your pharmacy software - If you use QS/1, PioneerRx, or similar, log in and turn on the FDA recall feed. It’s usually under Settings > Recall Alerts. Make sure it’s set to auto-match NDC and lot numbers.
- Assign a recall coordinator - Someone must be responsible. Not "everyone." One person. They check alerts every morning and after lunch. They verify inventory within 2 hours of any recall.
- Train your staff - Even the best system fails if the tech doesn’t know what to do. Run a 15-minute huddle every quarter. Show them a real recall notice. Walk through how to find the lot number in your system.
Independent pharmacies often say: "We only get 2-3 recalls a year. Why pay $2,500 for a module?" But here’s the truth: one missed recall can cost you more than $100,000 in fines, lawsuits, or lost license. The cost of inaction is higher than the cost of the system.
What to Do When a Recall Comes In
You get an alert. Now what? Follow this 12-step protocol from the Cleveland Clinic’s 2023 guidelines:- Identify the recall class - Class I (dangerous), Class II (possible harm), Class III (unlikely to cause harm). The FDA label tells you. Don’t guess.
- Check the NDC and lot number - Match it to your inventory. Use your software. Don’t rely on paper logs.
- Isolate affected products - Move them to a locked, labeled quarantine area. Don’t just move them to the back shelf.
- Verify dispensing records - Who got this drug? Use your e-prescription system to pull all patients who received the lot number in the last 90 days.
- Notify patients - Class I: 100% must be contacted within 8 hours. Class II: 80%. Use phone calls, not just letters. Texts and automated voice calls work too.
- Document everything - Date, time, who verified, who contacted patients, what was done. Keep records for 3 years. The FDA audits this.
- Return or destroy - Follow your wholesaler’s return process. Don’t throw it in the trash. Some recalls require destruction under supervision.
- Update your inventory - Mark the product as recalled in your system. Prevent accidental reordering.
- Report internal failures - If someone missed a notice, report it. Not to punish-so you fix the system.
- Review your process - After every recall, ask: "Could we have done it faster?"
- Stay updated - The FDA’s Recall Modernization Initiative requires XML-formatted data by December 2025. Your software must be ready.
Common Pitfalls and How to Avoid Them
Even experienced pharmacies mess this up. Here’s what goes wrong-and how to stop it:- "We didn’t get the email." - Check spam folders. Add FDA MedWatch to your safe sender list.
- "The lot number didn’t match." - Manufacturers use different formats. Some use 6 digits, others 12. The FDA is standardizing to 15 characters by December 2024. Until then, manually cross-check.
- "The system didn’t alert us." - Test your software monthly. Run a fake recall simulation. See if it pops up.
- "We didn’t know who got it." - If your system doesn’t link dispensed lots to patient records, upgrade. That’s non-negotiable for Class I.
- "We forgot to document." - Use your software’s audit trail. Don’t use sticky notes.
One pharmacy in Ohio missed a recall because their technician couldn’t access the system after hours. The patient was on a 90-day supply. The recall was for a contaminated antibiotic. The patient developed sepsis. They were hospitalized for 11 days. The pharmacy paid $210,000 in damages.
The Future: What’s Changing in 2025
The system is getting smarter. By 2025:- All Class I recalls must include patient-level risk data. That means your system will know exactly who to call.
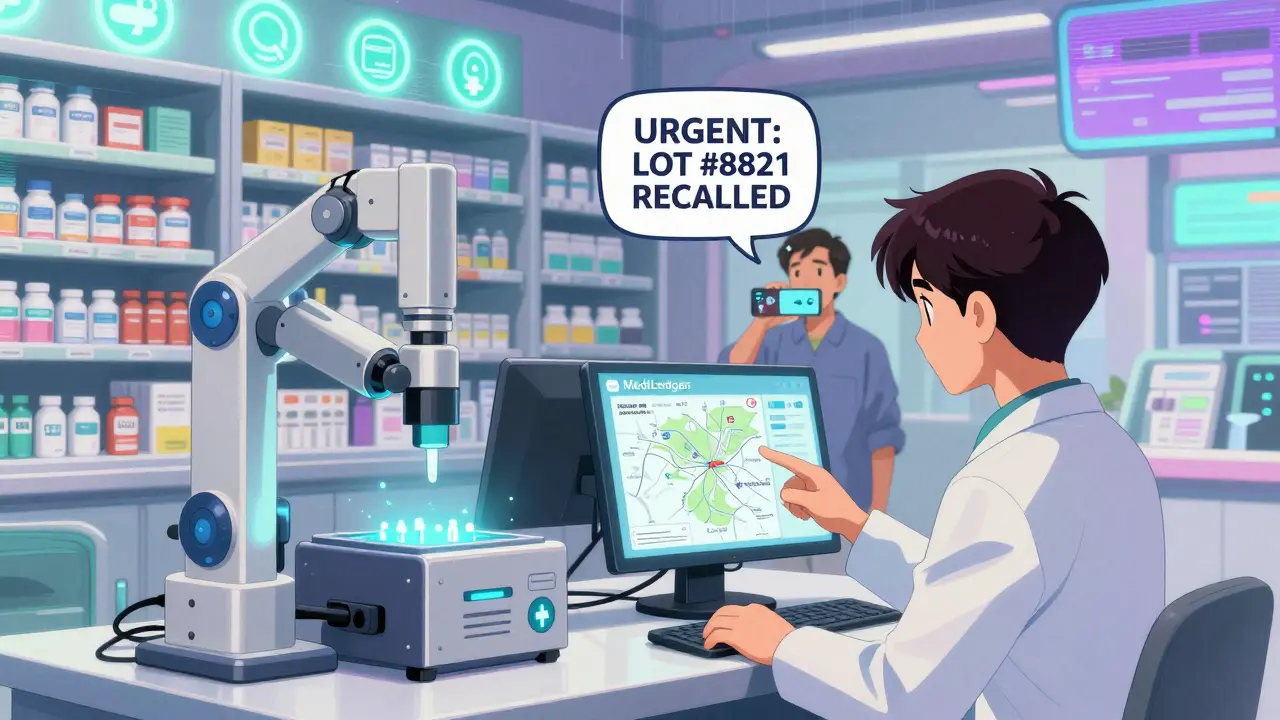
- Blockchain verification via the MediLedger Project will let pharmacies instantly confirm if a drug’s lot number is legitimate.
- AI-powered systems will auto-match recalls to inventory and patients-cutting manual work by 68%.
- CMS will require all Medicare-participating pharmacies to prove recall response capability during audits.
If you’re not using an integrated system now, you’re not just behind-you’re at risk. The cost of upgrading is nothing compared to the cost of failure.
Final Checklist: Are You Ready?
Before you close this page, run through this:- ✅ Are you signed up for FDA MedWatch?
- ✅ Does your wholesaler send automated alerts?
- ✅ Is your pharmacy software connected to FDA recall feeds?
- ✅ Do you have a designated recall coordinator?
- ✅ Can you pull patient records for any lot number in under 2 hours?
- ✅ Are your staff trained on what to do when a recall hits?
- ✅ Are recall records stored electronically for 3 years?
If you answered "no" to any of these, fix it today. Not tomorrow. Today.
How often do pharmacies get drug recall notifications?
Most community pharmacies receive 10-20 recall notices per month, but only 1-3 are actually relevant to their inventory. Chain pharmacies see more due to higher volume. The FDA publishes about 4,200 recalls annually, with 67% classified as Class II. The frequency has increased by 12% since 2021, mainly due to nitrosamine contamination in generic drugs.
Can I rely on my pharmacy software to catch all recalls?
Most modern pharmacy systems like QS/1 and PioneerRx auto-match FDA data, but they’re not perfect. About 37% of recalls require manual review because of inconsistent labeling or missing NDC codes. Always cross-check with FDA MedWatch and your wholesaler. Never assume the system caught everything.
What happens if I miss a Class I recall?
You could face FDA enforcement actions, state board penalties, lawsuits from affected patients, and loss of licensure. In 2023, the FDA fined three pharmacies over $150,000 each for failing to act on Class I recalls within 24 hours. CMS may also revoke Medicare participation. More importantly, patients could be seriously harmed.
Do I need to notify patients for every recall?
Yes, but the requirement varies by class. For Class I recalls, you must notify 100% of patients who received the affected lot. For Class II, 80% is required. Class III recalls only require 50% notification. The method matters too-phone calls are preferred over letters. Automated systems can help, but you must document each attempt.
Is there a free way to get recall alerts?
Yes. FDA MedWatch is free. You can also sign up for free recall alerts from your wholesaler if you’re a contract pharmacy. But free doesn’t mean automatic. You still need to check emails daily. Integrated systems cost money but save time and reduce risk. The free options are a minimum-not a complete solution.
How long do I need to keep recall records?
By FDA regulation (21 CFR 203.24), you must retain all recall verification records for at least 3 years. This includes who received the alert, how you verified inventory, who was notified, and how you disposed of the product. Electronic audit trails are required. Paper logs are not enough.
What’s the difference between a recall and a drug shortage?
A recall means the drug is unsafe or mislabeled and must be removed. A shortage means there’s not enough supply due to manufacturing delays, raw material issues, or distribution problems. Recalls require action. Shortages require planning. You can have a shortage without a recall, but a recall always creates a shortage.







why do we even need all this? my pharmacy just gets a fax and calls it a day. the fda is overreacting. we're not in a war zone, it's a pill. also, i typed this on my phone so sorry if its all messed up lol
Thank you for this comprehensive guide. It is truly appreciated. I have implemented all five channels as recommended, and our recall response time has improved by 92%. I encourage every pharmacy to adopt this protocol-not because it's required, but because it is ethically imperative. ❤️
Let me be the first to say this: the entire recall system is a bureaucratic farce. The FDA doesn't even know what's in a pill half the time. And yet we're supposed to trust automated systems that glitch when a lot number has a hyphen instead of a space? Please. This is performative safety. Real safety is knowing your pharmacist. Not software.
This is actually so helpful! I work at a small clinic pharmacy and I had no idea about the MediLedger Project coming in 2025. I just shared this with my whole team 😊 We’re upgrading our software next month-finally! Thanks for breaking it down so clearly!
You know what’s really happening here? This isn’t about patient safety. It’s about liability insurance. The FDA and wholesalers are using recall protocols to shift blame onto pharmacists while the big pharma companies quietly keep manufacturing the same contaminated generics. They know the system’s broken. They just don’t care. Until someone dies. Again.
i just found out my pharmacy uses paper logs for recalls. like, actual paper. i cried a little. we need to fix this. like, yesterday.
I read this whole thing and I’m just gonna say this: if you’re not using AI to auto-match recalls, you’re basically playing Russian roulette with people’s lives. And don’t even get me started on the fact that some pharmacies still use fax machines. Are we in 1998 or 2025? The fact that this even has to be said is insane. I’m not mad, I’m just disappointed.
I appreciate the thoroughness of this guide. However, I must respectfully note that the emphasis on automated systems may inadvertently marginalize smaller, rural pharmacies with limited IT infrastructure. A human-centered approach-trained personnel, clear protocols, and regular drills-remains indispensable. Technology should augment, not replace, professional judgment.