When you hear about tirzepatide for weight loss, you’re not just hearing about another diet pill. You’re hearing about a science breakthrough that’s changing how doctors treat obesity. Unlike older weight-loss drugs that only target one part of your body’s hunger system, tirzepatide hits two at once. It’s the first dual incretin therapy approved for chronic weight management in the U.S., and it’s working better than anything else on the market right now.
What Tirzepatide Actually Does
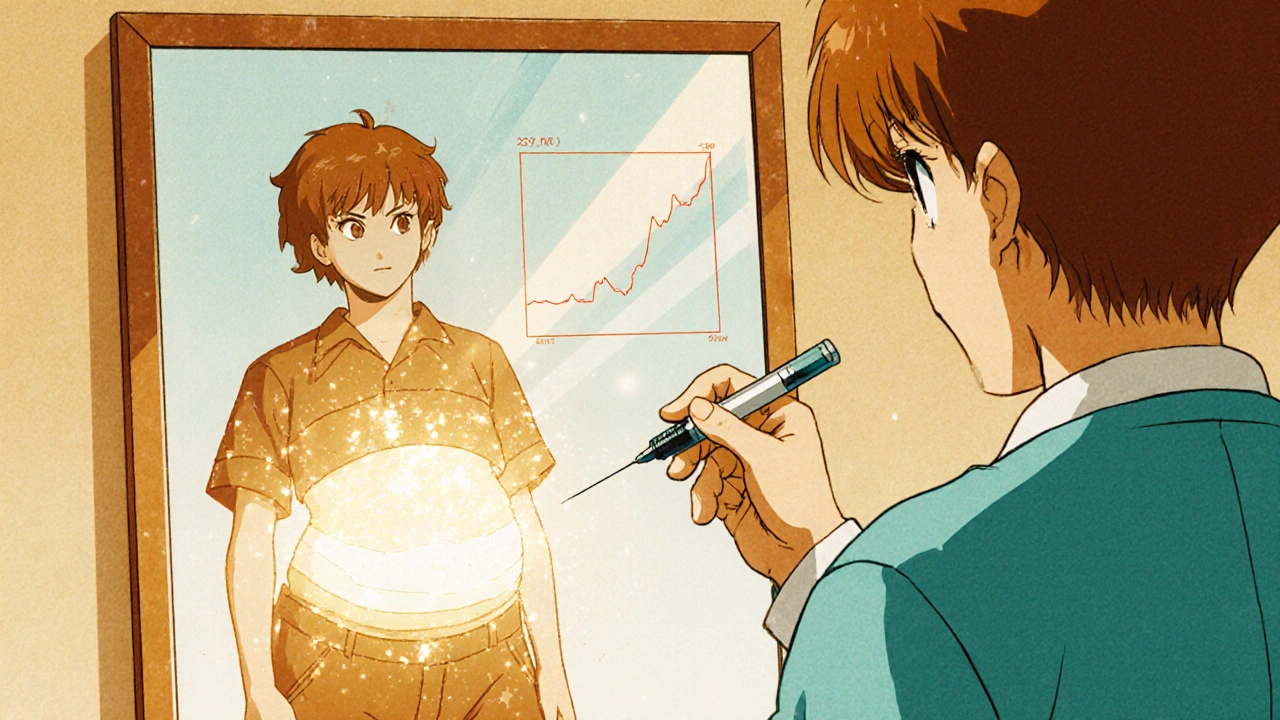
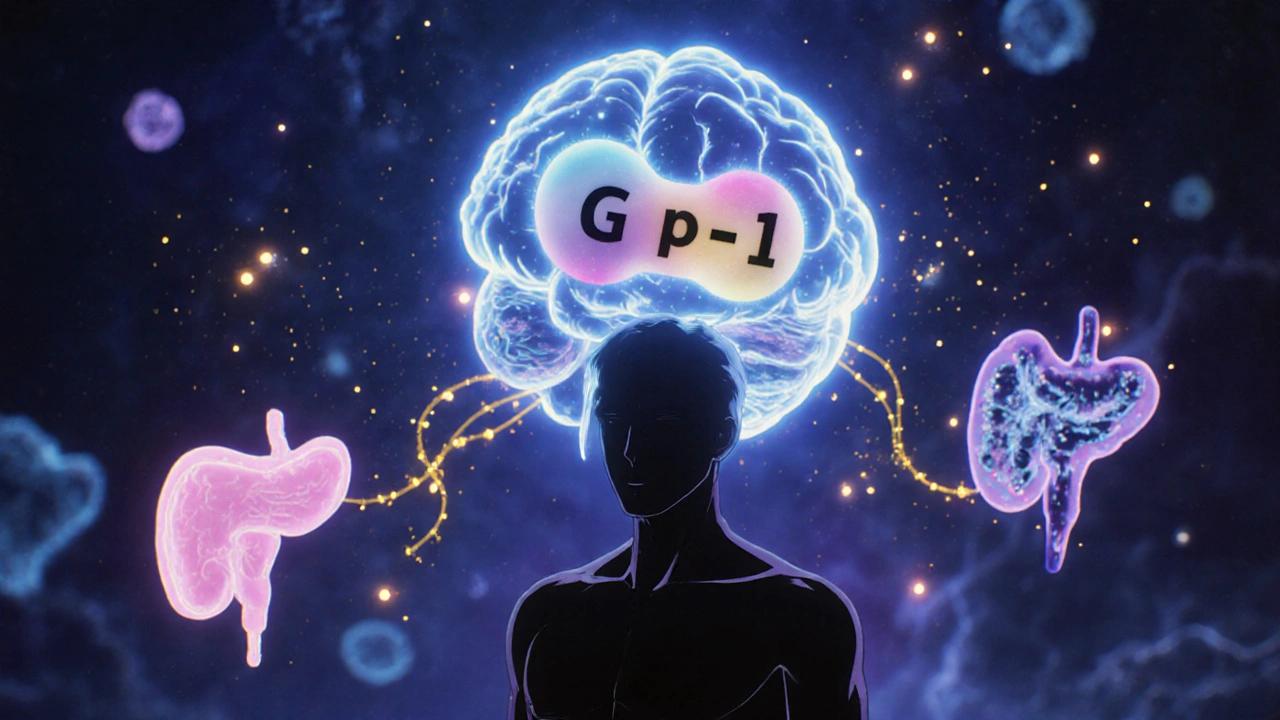
Tirzepatide is the active ingredient in Zepbound, the brand name for weight loss. It’s not a stimulant. It doesn’t block fat absorption. Instead, it mimics two natural hormones your body already makes: GLP-1 and GIP. These are called incretin hormones, and they’re released after you eat. Their job? Tell your pancreas to make insulin, slow down your stomach, and tell your brain you’re full.
Most weight-loss drugs before this only copied GLP-1 - like semaglutide (Wegovy). Tirzepatide adds GIP into the mix. That’s why it’s called a ‘twincretin.’ And that extra signal makes a huge difference. In clinical trials, people using the highest dose (15 mg weekly) lost an average of 22.4% of their body weight over 72 weeks. That’s not 20 pounds. That’s 50, 60, even 80 pounds for many people. One study showed it outperformed semaglutide by over 50% in weight loss.
How? It’s not just about appetite. Tirzepatide also improves how your body uses energy. It helps your muscles and fat cells take in more glucose. It reduces inflammation in fat tissue. It even makes your insulin-producing cells work better and live longer. This isn’t just suppression - it’s metabolic reset.
Why It Works Better Than GLP-1 Alone
At first glance, GLP-1 drugs like Wegovy and Saxenda seem similar. They all reduce hunger. But here’s the catch: people on tirzepatide lose more fat, not just weight. In the SURMOUNT-1 trial, those on tirzepatide lost nearly twice as much visceral fat - the dangerous kind around your organs - compared to those on semaglutide.
Why? Because GIP does something GLP-1 alone can’t. It boosts energy expenditure. Animal studies show it helps your body burn more calories at rest. Human trials suggest it improves how your body switches between burning sugar and fat. That’s why two people with the same appetite reduction can lose different amounts of weight. One might be burning more calories without even trying.
Experts at Duke University confirmed this in 2023. When they tested tirzepatide on human fat and muscle cells, they saw a synergy - the two hormones together activated pathways that neither could trigger alone. That’s the real secret: it’s not two drugs in one. It’s a new kind of signal your body wasn’t getting before.
How It’s Taken - And Why Timing Matters
Tirzepatide is a once-weekly injection. You give it under the skin - belly, thigh, or upper arm. It comes in pre-filled pens, like insulin. You don’t need to refrigerate it after the first use. But you do need to start low.
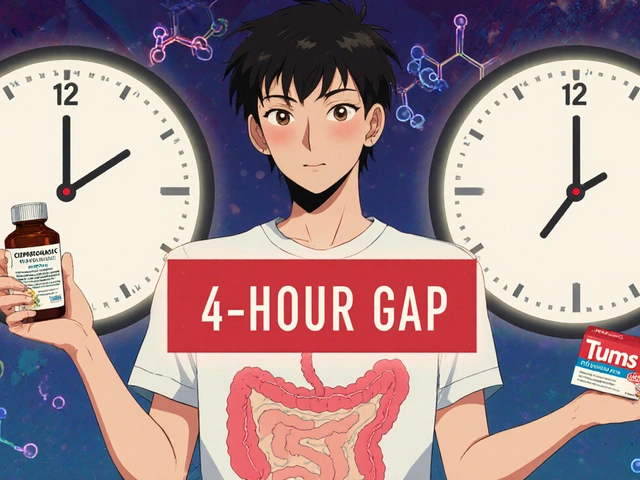
The FDA-approved dosing schedule takes 20 weeks to reach the full dose. You begin at 2.5 mg, then increase every four weeks: 5 mg, 7.5 mg, 10 mg, and finally 15 mg. Skipping steps or rushing the process is the #1 reason people quit.
Why so slow? Because the side effects hit hard if you jump in too fast. Nausea, vomiting, diarrhea - these aren’t rare. In trials, 25% of people had nausea, 10% vomited. But those numbers dropped dramatically when people stayed on the slow ramp-up. One patient on Reddit said, “I almost quit at 7.5 mg. Then I held that dose for six weeks instead of four. The nausea vanished.”
Doctors recommend eating smaller, low-fat meals during dose increases. Fatty foods slow digestion and make nausea worse. Drink water. Avoid lying down after eating. Some patients use ginger tea or OTC anti-nausea meds like dimenhydrinate during the first few weeks. Most side effects fade after the body adjusts.
Who Shouldn’t Take It
Tirzepatide isn’t for everyone. It’s absolutely not safe if you or a close family member has had medullary thyroid cancer. It’s also not recommended if you have multiple endocrine neoplasia syndrome type 2. These are rare, but serious. The FDA requires a risk evaluation program because animal studies showed thyroid tumors - though no human cases have been confirmed.
People with a history of pancreatitis should talk to their doctor. While the risk is low, it’s real. If you’ve had severe stomach issues in the past - gastroparesis, for example - tirzepatide’s slowing of digestion could make things worse.
It’s also not approved for use in pregnant women, children under 18, or people with type 1 diabetes. If you’re on insulin or other diabetes meds, your doses may need adjustment. Always tell your provider about every medication you take, including over-the-counter supplements.
Real Results - And Real Challenges
Across 1,247 patient reviews on Drugs.com, tirzepatide has an 8.2 out of 10 rating. Seventy-six percent reported losing more than 10% of their body weight. On Reddit’s r/Mounjaro community, users share weekly updates: “Lost 42 lbs in 5 months,” “My clothes fit differently,” “I can finally climb stairs without stopping.”
But there’s another side. About 32% of users in one analysis stopped treatment because of side effects. Nausea was the top reason - reported by 87% of those who quit. Some couldn’t tolerate even the lowest dose. Others found the cost or access barriers too high, despite co-pay programs.
One big surprise? People who’d already used GLP-1 drugs like semaglutide adapted faster. They knew what to expect. Their bodies were already used to slower digestion. They were more likely to stick with the 20-week plan. New users often need more support.
Cost and Access
The list price is around $1,023 for a 4-week supply. That sounds impossible. But here’s the reality: 89% of people with commercial insurance pay under $100 a month thanks to Eli Lilly’s co-pay assistance. The Lilly Cares Foundation helps eligible patients get it for free. Medicare Part D coverage varies - some plans cover it for weight loss, others only for diabetes.
Insurance often requires proof of obesity (BMI ≥30) and failure of diet and exercise. Some require documentation of weight-related health issues like high blood pressure or sleep apnea. That’s why endocrinologists and obesity specialists are the most common prescribers - they know how to navigate this.
Since Zepbound’s approval in November 2023, it’s become the fastest-growing weight-loss drug in history. In 2024, it generated $4.1 billion in global sales and captured 38% of the GLP-1 weight-loss market. Demand is outpacing supply in many areas.
What Happens When You Stop
This is the question no one wants to ask out loud: “If I stop, do I gain it all back?” The answer is yes - mostly.
Follow-up data from the SURMOUNT trials shows that within six months of stopping tirzepatide, people regain about 12-15% of the weight they lost. That’s not all of it, but it’s enough to be discouraging. The key is understanding: this isn’t a cure. It’s a tool. Like blood pressure medication, you take it as long as you need it.
Some patients transition to lifestyle changes and maintain results. Others stay on a lower maintenance dose. A few restart treatment after a break. There’s no shame in that. Obesity is a chronic condition. Managing it often means managing medication, just like diabetes or heart disease.
The Future: What’s Next
Tirzepatide isn’t the end - it’s the beginning. In October 2024, the FDA approved Zepbound not just for weight loss, but for treating obstructive sleep apnea in adults with obesity. That’s huge. It’s the first time a weight-loss drug got approval for a specific condition beyond just shedding pounds.
Lilly is already testing a triple agonist - retatrutide - that targets GLP-1, GIP, and glucagon. Early results show 24.2% weight loss in just 24 weeks. That’s even more than tirzepatide.
Researchers are also looking at tirzepatide for non-alcoholic fatty liver disease (NASH), heart failure, and even Alzheimer’s. The science behind dual incretin signaling is opening doors we didn’t know existed.
For now, tirzepatide is the most effective weight-loss drug we have. It works because it doesn’t just fight hunger. It reprograms your metabolism. It doesn’t just help you lose weight - it helps your body function better while you do it. But it’s not magic. It’s medicine. And like all medicine, it works best when you understand how to use it - and when you know what to expect.
Is tirzepatide the same as semaglutide?
No. Tirzepatide is a dual agonist that activates both GLP-1 and GIP receptors. Semaglutide only activates GLP-1. This difference makes tirzepatide more effective for weight loss - in head-to-head trials, people lost over 50% more weight on tirzepatide compared to semaglutide at maximum doses. They’re both injectables, taken weekly, but they work differently in the body.
How long does it take to see weight loss with tirzepatide?
Most people start seeing results within 4 to 8 weeks, but the biggest losses happen after 16 to 24 weeks. Clinical trials showed an average of 10% weight loss by 12 weeks and over 20% by 72 weeks. The full effect takes time because the dose is increased slowly to reduce side effects. Don’t expect dramatic results in the first month - patience matters.
Can you take tirzepatide if you don’t have diabetes?
Yes. Tirzepatide is approved under the brand name Zepbound specifically for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition. You don’t need to have diabetes to qualify. In fact, most people using it for weight loss don’t have diabetes.
What are the most common side effects of tirzepatide?
The most common side effects are gastrointestinal: nausea (20-25%), diarrhea (15-18%), vomiting (7-10%), constipation, and stomach pain. These usually improve after a few weeks as your body adjusts. Taking the dose slowly and eating smaller, low-fat meals helps reduce them. Serious side effects like pancreatitis or gallbladder disease are rare but possible.
Do you have to stay on tirzepatide forever?
You don’t have to, but if you stop, you’ll likely regain some weight - about 12-15% within six months. Tirzepatide doesn’t cure obesity; it manages it. Many people stay on it long-term, like they would for high blood pressure. Some switch to lower doses or combine it with lifestyle changes to maintain results. The decision depends on your goals, health, and tolerance for side effects.
How much does tirzepatide cost with insurance?
With commercial insurance, most people pay between $45 and $75 per month thanks to Eli Lilly’s co-pay assistance program. Without insurance, the list price is over $1,000 per month. Medicare coverage varies - some plans cover it for weight loss, others only for diabetes. The Lilly Cares Foundation offers free medication to eligible low-income patients.





This is LIFE-CHANGING stuff 😍 I lost 47 lbs in 6 months and I swear I feel like a new person. No more noon naps, no more panting up stairs - just pure joy. 🎉
While the clinical data is undeniably compelling, one must not overlook the profound ethical implications of pharmacologically altering human metabolism as a first-line intervention for a condition that is, at its core, a manifestation of systemic societal failure.
The 22.4% weight loss figure is statistically significant, but the attrition rate due to GI side effects is 32%. That’s a 1:3 ratio of benefit to dropout. Not sustainable at scale. Also, the long-term metabolic rebound data is alarming.
Let’s be real - this isn’t medicine. It’s a luxury biotech product for the overprivileged who can’t be bothered to eat a salad. Meanwhile, the rest of us are stuck with kale and guilt. 🤡
They’re calling it a breakthrough - but have you seen the patent filings? This was designed to replace insulin for diabetics first. Now they’re repackaging it as a weight-loss drug to exploit the ‘obesity epidemic’ narrative. Big Pharma’s next trillion-dollar scam.
Bro, I tried this for 3 weeks. Nausea hit me like a truck. 😵💫 Then I remembered my grandpa ate rice and curry and lived to 92. Maybe we don’t need fancy injections. Maybe we just need to stop eating processed junk.
So we’ve replaced the American dream of ‘work hard, lose weight’ with ‘pay $1000/month and pray your stomach doesn’t revolt’. Truly, we’ve reached peak capitalism. 🤖💸
The science here is beautiful. The body has its own language - GLP-1 and GIP are just two words in that sentence. Tirzepatide listens. Most treatments shout. There’s wisdom in that.
The dual incretin agonism activates PI3K-AKT and AMPK pathways synergistically, enhancing mitochondrial biogenesis in adipose tissue while suppressing hypothalamic NPY/AgRP signaling. This isn’t appetite suppression - it’s metabolic reprogramming at the transcriptional level.
If you’re thinking about this, just start low and go slow. I was terrified at 5mg - held it for 6 weeks, drank ginger tea, ate like a bird. Now I’m at 15mg and feel amazing. You got this 💪
I mean… it’s just a glorified appetite suppressant wrapped in a lab coat and a $1000 price tag. We’re not curing obesity. We’re just outsourcing willpower to a pharmaceutical corporation. Deep.
This isn’t a drug - it’s a weapon against laziness and bad choices. If you’re too weak to eat clean and move your body, fine, take it. But don’t act like it’s a miracle. It’s not. It’s just better than the junk they sold us before.
i started at 2.5mg and just kept going slow and now im at 15mg and lost 50lbs!! i dont even know how to cook but i eat veggies and drink water and it just works!!