Introduction: Understanding Bisacodyl and its Effects
As a responsible individual concerned about my gut health, I often hear about various medications and supplements that claim to improve digestion and promote regular bowel movements. One of these medications, bisacodyl, is a commonly recommended over-the-counter laxative. However, I've always wondered about the long-term effects of bisacodyl on gut health. In this article, I will explore the benefits and potential risks associated with prolonged use of this popular laxative.
How Does Bisacodyl Work?
Bisacodyl is a stimulant laxative that works to alleviate constipation by increasing the movement of the intestines. This action helps to soften the stool, making it easier to pass through the digestive system. The medication is typically taken in tablet form or as a suppository, and its effects can be felt within a few hours of consumption. While bisacodyl is generally considered safe for short-term use, it's important to understand the potential long-term effects on gut health before incorporating it into a regular routine.
Benefits of Bisacodyl for Gut Health
Short-term use of bisacodyl can provide immediate relief from constipation and promote regular bowel movements. This can be especially beneficial for individuals who suffer from occasional bouts of constipation due to factors such as stress, dehydration, or changes in diet. By ensuring that the digestive system is functioning optimally, bisacodyl can help to prevent complications such as hemorrhoids and anal fissures, which can result from chronic constipation.
Potential Risks of Long-term Bisacodyl Use
While bisacodyl can be an effective solution for short-term constipation relief, long-term use can potentially lead to some negative effects on gut health. These may include:
Dependency
Regular use of bisacodyl and other stimulant laxatives can cause the muscles in the intestines to become reliant on the medication to function properly. This can lead to a decreased ability to have a bowel movement without the assistance of a laxative, which can ultimately result in a vicious cycle of dependency and worsening constipation.
Electrolyte Imbalance
Long-term use of bisacodyl can lead to an imbalance of electrolytes, such as potassium and sodium, in the body. These electrolytes play a crucial role in maintaining proper hydration levels and ensuring that the muscles and nerves function properly. An electrolyte imbalance can lead to symptoms such as muscle cramping, weakness, and irregular heartbeat, which can be potentially dangerous if left untreated.
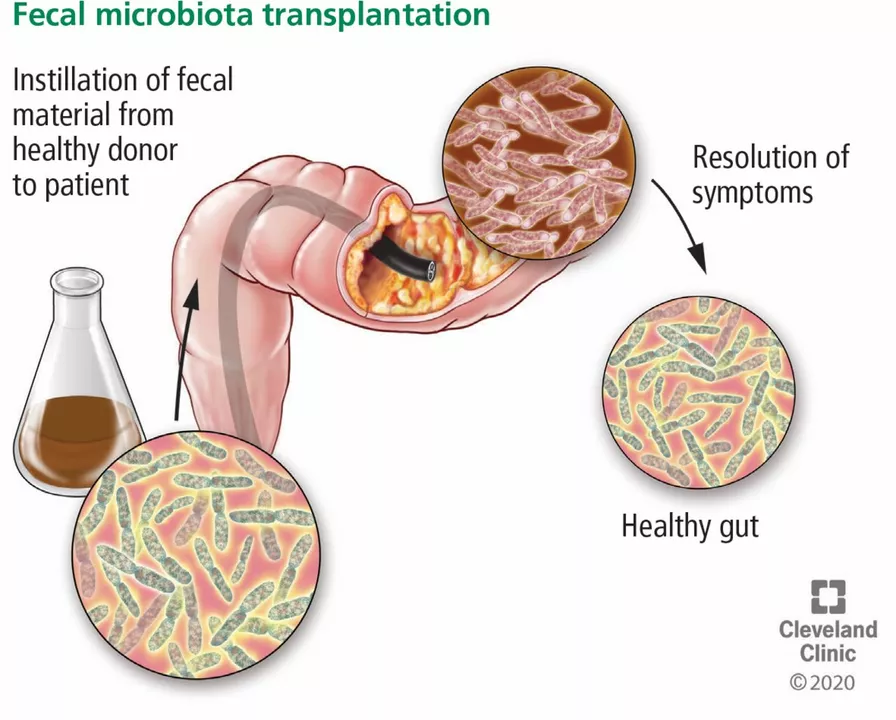
Alteration of Gut Microbiota
Emerging research suggests that long-term use of bisacodyl may negatively impact the delicate balance of bacteria in the gut. These microbes play a crucial role in maintaining overall gut health and digestion, and a disruption in their balance can lead to a variety of gastrointestinal issues, such as bloating, gas, and diarrhea.
Alternative Treatments for Constipation
Given the potential risks associated with long-term bisacodyl use, it's important to consider alternative treatments for constipation that can be more sustainable and less harmful to gut health. Some possible options include:
Dietary Changes
Incorporating more fiber-rich foods, such as fruits, vegetables, and whole grains, into the diet can help to promote regular bowel movements and prevent constipation. Additionally, staying properly hydrated by drinking plenty of water can help to soften the stool and make it easier to pass.
Physical Activity
Regular exercise is another effective way to promote healthy digestion and prevent constipation. Physical activity helps to stimulate the muscles in the intestines, which can improve their function and facilitate more regular bowel movements.
Probiotics
Probiotic supplements, which contain beneficial bacteria, can help to maintain a healthy balance of gut microbiota and promote overall gut health. These supplements can be particularly helpful for individuals who have experienced a disruption in their gut bacteria due to factors such as antibiotic use or long-term laxative dependency.
Consulting a Healthcare Professional
While it's important to be proactive in maintaining gut health, it's also crucial to consult a healthcare professional before making any significant changes to one's routine or incorporating new medications or supplements. A healthcare provider can help to identify the underlying cause of constipation and recommend the most appropriate treatment plan, which may include a combination of lifestyle changes, dietary modifications, and, if necessary, the short-term use of laxatives such as bisacodyl.
Conclusion
Ultimately, while bisacodyl can be an effective short-term solution for constipation relief, it's important to be aware of the potential long-term effects on gut health. By exploring alternative treatments and working closely with a healthcare professional, individuals can find a more sustainable and healthy approach to maintaining regular bowel movements and promoting overall gut health.







I've been using bisacodyl for years because I have IBS-C. It's the only thing that works consistently. I know it's not ideal, but switching to fiber and water hasn't helped much. I just hope my colon doesn't give out one day.
Bisacodyl? Oh, the old-school stimulant laxative-like a tiny, chemical firework in your sigmoid colon. It’s effective, yes-but prolonged use? That’s like training your intestines to need a referee to even consider moving. The gut isn’t a lazy teenager; it’s a finely tuned orchestra. And when you keep forcing the violins to play with a megaphone, eventually, they stop playing altogether. Electrolyte imbalance? Gut dysbiosis? Welcome to the collateral damage of convenience.
I’ve seen my mother rely on this for decades. She never talks about it, but I know. She’s always careful with her diet now, but still keeps a bottle in the cabinet. I think she’s scared to stop.
I get why people use it. Constipation sucks. But there’s a difference between helping your body and hijacking it. I used to take it weekly. Then I started walking after dinner, drinking more water, and eating prunes. Took a month, but now I don’t need it. My gut feels… quieter. In a good way.
Oh sweet mercy, another ‘I’m so responsible’ post about laxatives. Next you’ll be writing a 10-page essay on why you ‘carefully’ use Tums. Congrats, you’ve discovered that drugs have side effects. Who knew?
This is why America is collapsing. You people treat your guts like they’re disposable. In my country, we don’t medicate away natural bodily functions-we eat right, move, and endure. You think fiber is ‘alternative’? It’s called evolution. You’re not sick-you’re lazy.
You must understand, my dear, that the human gut is not a simple plumbing system-it is a sacred ecosystem, a microcosm of cosmic balance, and to tamper with it through chemical stimulation is akin to burning the Vedas to light a candle. The ancients knew this. They used flaxseed, warm water, and yoga. Not chemicals. Not modernity. Not bisacodyl. You are not healing-you are betraying your lineage.
It is imperative that individuals recognize the physiological consequences of prolonged stimulant laxative use. The colon's intrinsic peristaltic activity may become attenuated, leading to a condition known as lazy bowel syndrome. This is not a trivial matter. Medical literature consistently advises against dependency-inducing interventions without concurrent behavioral modification.
Prunes work. Try them.
i used bisacodyl for like 3 years straight bc i was too lazy to eat veggies. then one day my butt just said ‘nope’ and refused to cooperate even with the meds. now i eat oatmeal every morning and drink water like a responsible adult. it’s boring but it works. also i miss the feeling of instant relief tho lol
I’ve been reading about gut health for years now, and what’s fascinating is how many people treat constipation like a problem to be solved with a pill, when it’s often a symptom of something deeper-stress, lack of movement, dehydration, even emotional suppression. I think bisacodyl gives a false sense of control. It doesn’t fix the root. It just mutes the alarm.
The microbiome disruption is the most underdiscussed consequence. Bisacodyl doesn’t just stimulate peristalsis-it alters the mucus layer, reduces microbial diversity, and increases zonulin expression, which compromises intestinal barrier integrity. You’re not just ‘going to the bathroom’-you’re triggering a cascade of inflammatory signaling that may contribute to systemic issues. This isn’t anecdotal-it’s in the Journal of Gastroenterology, 2021.
lol u think ur so smart writing this whole essay. i used bisacodyl for 10 yrs and my gut is fine. ur just scared of meds. also prunes taste like dirt. go drink your kombucha and cry
I’ve seen this in clinical practice-patients come in with ‘lazy colon’ after years of laxatives. The worst part? They’re ashamed. They think it’s their fault. But it’s not. It’s a system failure. We overprescribe quick fixes and underinvest in lifestyle support. The solution isn’t just ‘eat more fiber’-it’s better access to nutritionists, physical activity programs, mental health care. Gut health is holistic.
In India, our grandmothers used to give us a spoon of ghee with warm milk before bed. No chemicals. No panic. Just gentle nourishment. I tried bisacodyl once after a long flight-it worked, yes. But I felt guilty. Like I cheated my body. Now I drink warm water with lemon, walk after meals, and sleep on my left side. My digestion is better than ever. Nature knows best.
Oh wow. You wrote an entire article about how bisacodyl isn’t a magic bullet. Groundbreaking. Next you’ll reveal that smoking causes lung cancer. Maybe next time, just say ‘don’t abuse laxatives’ and save us all the PowerPoint.
Your article exhibits a profoundly naive, Western-centric bias toward ‘natural’ alternatives as inherently superior. The notion that fiber, prunes, and yoga constitute a scientifically validated therapeutic regimen is not only reductive but statistically unsupported in populations with low dietary fiber intake. Bisacodyl, while not without risk, is a pharmacologically precise intervention. To demonize it is to reject evidence-based medicine in favor of folk remedies. This is not wellness-it is pseudoscientific romanticism.