When you have type 2 diabetes, a condition where your body doesn’t use insulin properly, leading to high blood sugar. Also known as insulin resistance, it’s not just about sugar—it’s about how your whole body reacts to food. The good news? What you eat can turn things around. Many people lower their blood sugar, lose weight, and even reverse their diagnosis—not with pills, but with simple, everyday food choices.
Blood sugar control, the process of keeping glucose levels steady to avoid spikes and crashes isn’t about cutting out carbs entirely. It’s about choosing the right kinds. Whole grains, beans, and vegetables slow down sugar absorption. Refined carbs like white bread, sugary cereals, and soda? They spike your blood sugar fast, then crash it, leaving you hungrier and more tired. Studies show that people who swap processed carbs for fiber-rich ones drop their HbA1c (a key diabetes marker) by up to 1% in just three months. That’s like going from 7.5% to 6.5%—a big step toward reducing medication.
Insulin resistance, when your cells stop responding well to insulin, forcing your pancreas to work harder gets worse with extra weight, especially around your belly. Losing just 5% of your body weight can improve insulin sensitivity by 50%. That’s not magic—it’s science. A 200-pound person losing 10 pounds can see their fasting blood sugar drop into the normal range. And it’s not about starving. It’s about eating more protein, healthy fats, and non-starchy veggies. Eggs, salmon, nuts, spinach, broccoli—they fill you up without spiking glucose.
People with type 2 diabetes often get told to eat "balanced meals," but that’s too vague. What does balanced even mean? It means filling half your plate with non-starchy veggies, a quarter with lean protein, and a quarter with complex carbs—not rice, not pasta, not potatoes. And forget counting calories. Start counting carbs in grams, and learn how your body reacts. One person might handle a small apple fine. Another might need to skip it. Track your blood sugar after meals. That’s the real guide.
And don’t fall for the "diabetic-friendly" labels. Those snacks often have just as many carbs, just swapped out with artificial sweeteners that can still trigger cravings. Real food wins every time. A piece of grilled chicken with roasted Brussels sprouts and olive oil? That’s your power meal. A low-sugar granola bar? Probably not.
What you drink matters too. Soda, juice, sweet coffee drinks—they’re liquid sugar bombs. Water, black coffee, unsweetened tea—those are your friends. Even alcohol can mess with your liver’s ability to regulate blood sugar, especially if you’re on metformin. It’s not about never drinking—it’s about knowing how it affects you.
There’s no one-size-fits-all diet for type 2 diabetes nutrition. Some do well with low-carb. Others thrive on Mediterranean-style eating. The key is consistency, not perfection. You don’t need to be flawless. You just need to make better choices more often than not. And when you do, your energy climbs, your mood steadies, and your need for meds drops.
Below, you’ll find real, practical guides that show exactly how to eat for better blood sugar, how to lose weight without feeling deprived, and what science says about foods that help or hurt. No fluff. No trends. Just what works—for your body, your life, and your future.
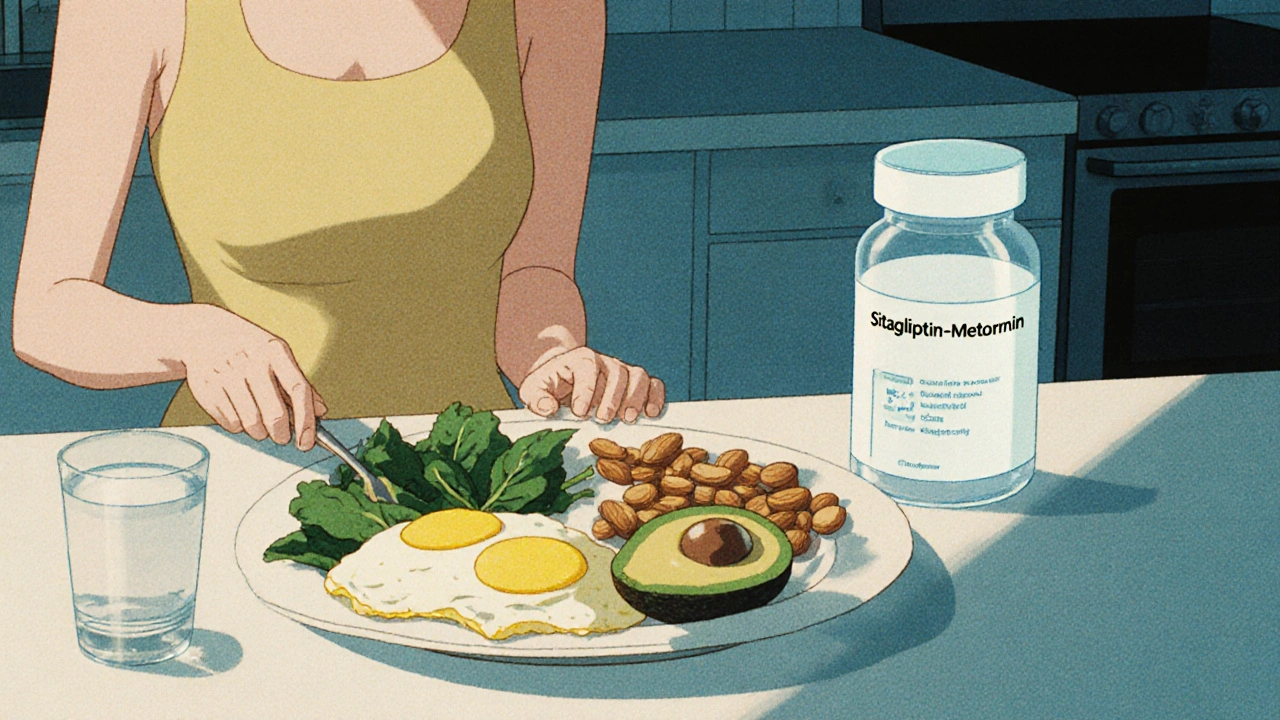
Diet plays a critical role in how well sitagliptin-metformin works for type 2 diabetes. Learn which foods boost its effectiveness, which to avoid, and how timing and portion control make a real difference in blood sugar control.
