When you take sitagliptin, a prescription medication used to lower blood sugar in adults with type 2 diabetes by helping the body release more insulin after meals. It’s not a magic pill—it works best when your diet supports its action. Many people think taking sitagliptin means they can eat normally, but that’s not true. This drug helps your pancreas make more insulin when you eat carbs, so what you eat directly affects how well it works.
Type 2 diabetes, a condition where your body doesn’t use insulin properly, leading to high blood sugar isn’t just about medication. It’s about timing, portion size, and food quality. Sitagliptin lowers blood sugar by blocking an enzyme called DPP-4, which breaks down natural hormones that stimulate insulin. But if you eat a huge plate of white rice or a sugary smoothie, your body still floods your bloodstream with glucose—and sitagliptin can’t keep up. That’s why diet isn’t just helpful, it’s essential.
Think of sitagliptin as your body’s helper, not its savior. Pair it with meals that are high in fiber, low in refined sugar, and balanced with lean protein. A study published in the Journal of Clinical Endocrinology & Metabolism found that people on sitagliptin who ate consistent, moderate-carb meals saw 20% better blood sugar control than those who skipped meals or ate large portions irregularly. You don’t need to go keto or count every gram of carbs, but you do need to avoid sugar spikes. Swap white bread for whole grain, pick berries over juice, and eat vegetables first at meals to slow glucose absorption.
Blood sugar control, the goal of managing diabetes through medication, diet, and lifestyle isn’t just about numbers on a meter. It’s about energy, mood, and long-term health. When your blood sugar swings wildly, you get tired, hungry again fast, and more likely to crave sugar. That cycle is hard to break—unless you eat steady, smart meals. Sitagliptin helps smooth those spikes, but only if you give it stable fuel. Skipping breakfast? That can make your afternoon sugar crash worse. Eating late at night? Your liver keeps releasing glucose, and sitagliptin can’t fully counter it.
There’s no one-size-fits-all diet for sitagliptin users, but there are clear patterns in what works. People who track their meals and match them with their medication schedule report fewer highs and lows. You don’t need to be perfect—just consistent. Try eating three balanced meals a day, with snacks only if you’re truly hungry. Avoid liquid calories like soda, sweet tea, or flavored coffee drinks—they spike blood sugar faster than solid food. And don’t forget water. Dehydration can make blood sugar readings look higher than they are.
Some people think they can skip diet changes because they’re on medication. That’s a mistake. Sitagliptin works better when your body isn’t fighting constant sugar overload. The real power comes from combining the drug with habits that reduce insulin resistance—like eating more vegetables, walking after meals, and avoiding processed snacks. You’re not just taking a pill—you’re rebuilding how your body handles food.
Below, you’ll find real advice from people who’ve learned how to eat with sitagliptin—not just for weight loss, but for steady energy, better sleep, and fewer diabetes complications. These aren’t generic tips. They’re the strategies that actually work when you’re trying to control blood sugar day after day.
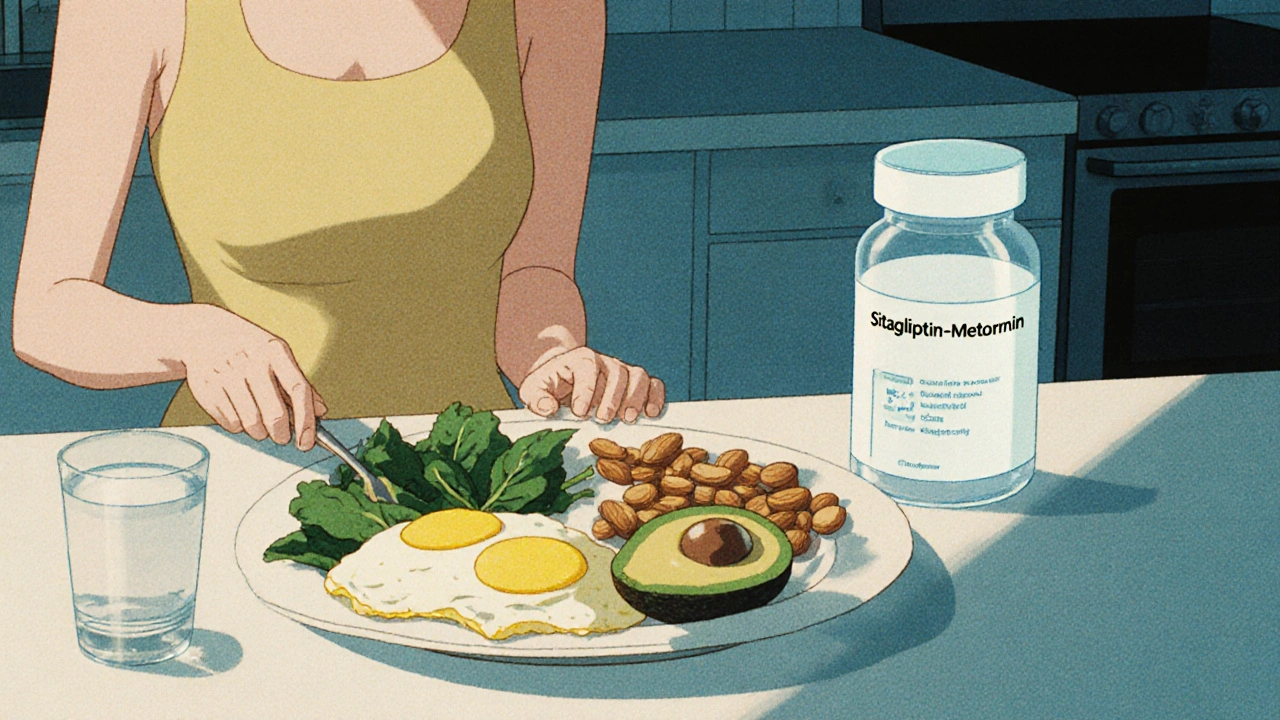
Diet plays a critical role in how well sitagliptin-metformin works for type 2 diabetes. Learn which foods boost its effectiveness, which to avoid, and how timing and portion control make a real difference in blood sugar control.
