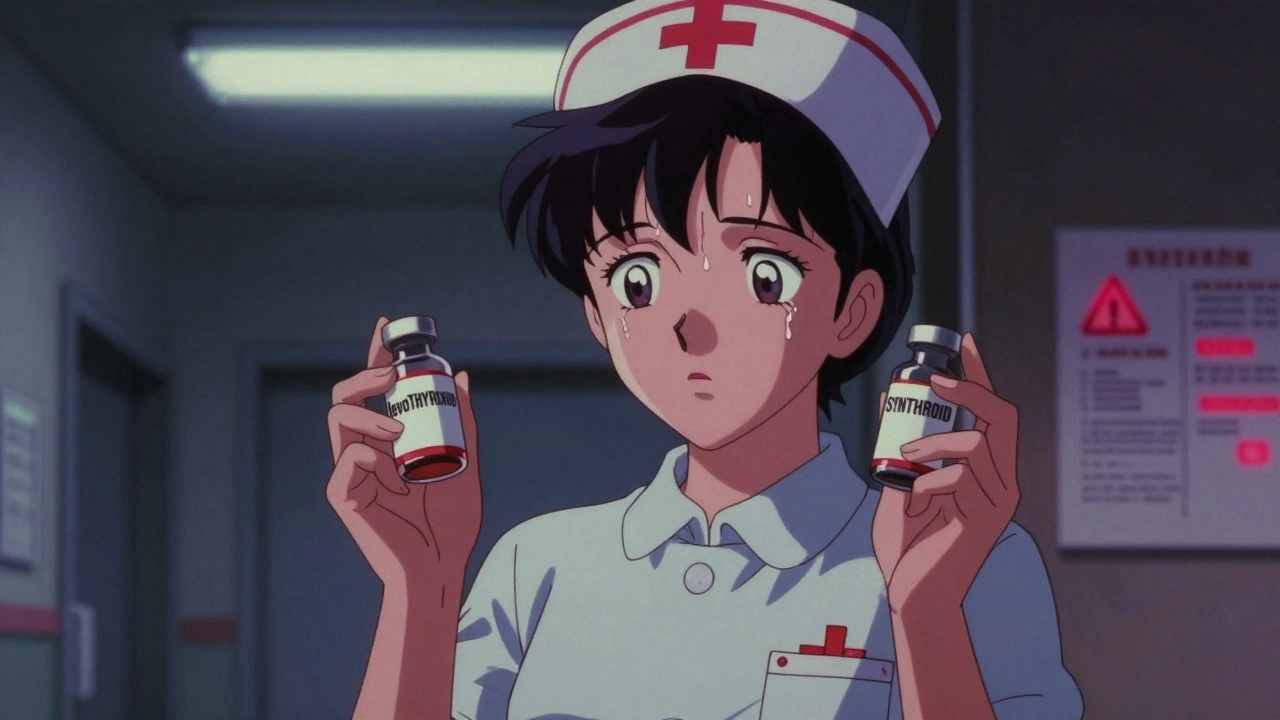
When two drugs LASA medications, look-alike and sound-alike drugs that are easily confused by patients and providers. Also known as look-alike sound-alike drugs, they cause thousands of preventable errors every year—even in top hospitals. This isn’t about rare exceptions. It’s about common pills, injections, and labels that slip through because they’re too close in spelling, pronunciation, or packaging. A patient meant to get hydralazine for high blood pressure ends up with hydroxyzine, an antihistamine. The result? A dangerous drop in blood pressure, dizziness, even hospitalization. These aren’t hypotheticals—they happen daily, and most people have no idea.
These errors don’t just happen because someone misreads a script. They’re built into the system. medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm involving LASA drugs are among the top causes of preventable harm in healthcare. Think epinephrine vs epinephrine (yes, same spelling, different concentrations). Or chlorpromazine and chlorthalidone—one treats psychosis, the other high blood pressure. Mix them up, and you’re risking coma or heart failure. Even pharmacy safety, the systems and practices designed to prevent drug errors in dispensing and administration can fail if labels aren’t clear, if staff are rushed, or if no one double-checks.
What makes LASA drugs so tricky is that they’re not outliers—they’re everywhere. You’ll find them in your medicine cabinet, your doctor’s prescription pad, and the hospital’s IV cart. The FDA and WHO both list dozens of high-risk pairs. Some are generics, some are brand names, but all share one thing: they’re easy to confuse. And when you’re tired, stressed, or in pain, your brain doesn’t catch the difference between propranolol and propafenone, or metformin and metoprolol. That’s why checking the drug name, dose, and purpose every single time matters. It’s not paranoia—it’s survival.
The good news? You don’t have to accept this risk. You can ask your pharmacist to write out the drug’s purpose on the label. You can use pill organizers with clear labels. You can bring a list of all your meds to every appointment. And if something feels off—like a pill that looks different or a side effect you’ve never had—speak up. The system isn’t perfect, but your awareness can stop an error before it starts. Below, you’ll find real stories, real cases, and real fixes from people who’ve been there. No fluff. Just what you need to stay safe.
Look-alike and sound-alike medication names cause thousands of preventable errors each year. Learn which drug pairs are most dangerous, why mistakes keep happening, and how patients and staff can stop them.
