Every year, over 1.3 million people in the U.S. suffer preventable harm because they misunderstood their medication instructions. It’s not because they’re careless. It’s because the labels don’t speak their language.
Why Medication Labels Are So Confusing
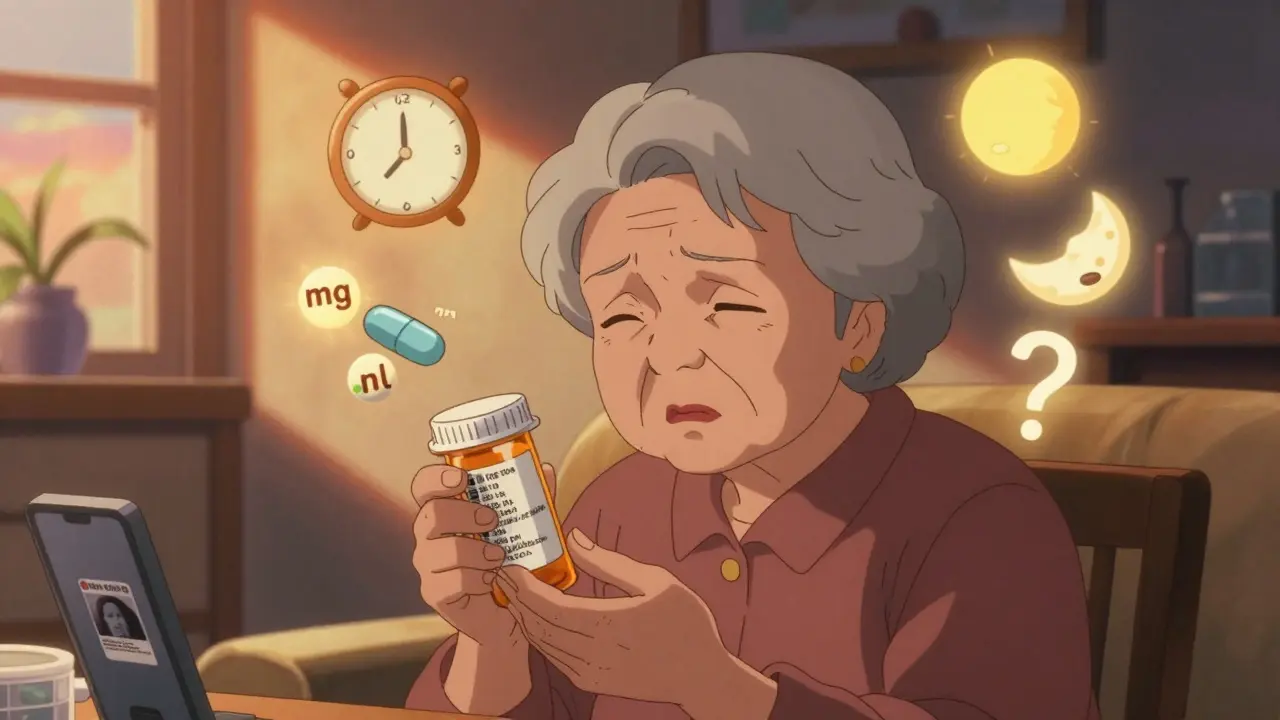
Most prescription bottles still use phrases like "Take 1 tablet by mouth twice daily" or "Take every 4-6 hours as needed." These sound simple-until you’re tired, stressed, or dealing with chronic pain. A 2009 study found that nearly half of patients misinterpreted these standard labels. Even people who read well struggled. For those with lower literacy or limited math skills, the risk skyrockets.One patient thought "take every 12 hours" meant "take twice a day," so she took both doses at breakfast and dinner-double the dose. Another confused "mg" with "ml," and gave her child five times the intended amount of liquid medicine. These aren’t rare mistakes. They’re predictable ones.
The problem isn’t just wording. It’s design. Labels often cram text into tiny spaces. They use symbols without explaining them. Some don’t even list active ingredients on the front. One review of children’s cough syrups found that 63% used confusing charts instead of clear instructions. Parents were left guessing.
What Works: Clear Labels That Actually Help
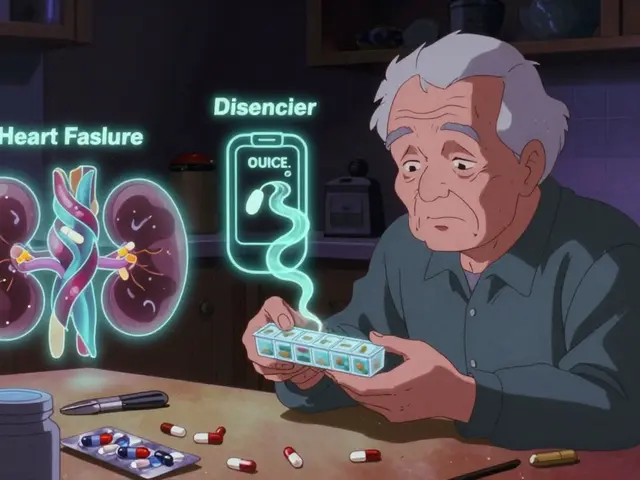
The good news? Simple changes make a huge difference. A 2013 study tested patient-centered labels that said: "Take 1 tablet in the morning and 1 tablet in the evening." That one change cut the number of people who took too much medicine in 24 hours by 32%. Not because they were smarter. Because the instructions were clearer.Another winning strategy is the Universal Medication Schedule (UMS). Instead of "twice daily," it uses four simple times: morning, noon, evening, bedtime. A Wisconsin health system that switched to UMS saw a 47% drop in dosing confusion among older adults taking five or more pills a day. One 72-year-old patient said: "I finally understood when to take my pills. Before, I was just guessing."
Visuals matter too. Adding simple pictograms-like a sun for morning, a moon for bedtime-boosted correct understanding by 28% among people with low health literacy. The U.S. Pharmacopeia now requires these visuals on all prescription labels by May 2025. That’s a big step forward.
How to Read a Label Like a Pro
You don’t need a medical degree to understand your meds. Just follow these steps:- Check the active ingredient. If you’re taking more than one medicine, make sure you’re not doubling up. Many cold and pain meds contain acetaminophen. Taking two at once can cause liver damage.
- Look for the dose amount. Is it "5 mL" or "5 mg"? mL is liquid. mg is powder or tablet. Mixing them up is dangerous.
- Understand the timing. "Take every 8 hours" means every 8 hours, not three times a day. "Take twice daily" means two times a day, not at breakfast and dinner only.
- Watch for "as needed". This doesn’t mean "take whenever you feel like it." It means only if you have the symptom, and only up to the max dose listed.
- Ask: "What does ‘take with food’ mean?" Does it mean before, during, or after? If you’re not sure, ask your pharmacist. It matters for how the drug works.
Don’t rely on memory. Write it down. Or better yet, take a photo of the label with your phone. Keep it in your notes app.

What Pharmacists Wish You Knew
Pharmacists see the same mistakes over and over. Here’s what they want you to know:- "Take as directed" isn’t helpful. Ask them to spell it out.
- "Take on an empty stomach" means no food for at least an hour before and after.
- "Take with water" doesn’t mean soda, juice, or milk. Water is best unless told otherwise.
- If you’re using a syringe or measuring cup, rinse it with water after each use. Leftover medicine can mess up your next dose.
- Never guess. If you’re unsure, call the pharmacy. They’re there to help.
One pharmacist in Manchester shared a story about a woman who drank albuterol from the plastic container because she thought it was a "syringe." The label didn’t say "do not drink," and the cap looked like a cup. That’s why standardization matters.
Teach-Back: The Simple Trick That Saves Lives
Doctors and pharmacists are starting to use something called the "teach-back" method. It’s simple: after explaining your meds, they ask you to explain it back in your own words."So, Mrs. Jones, can you tell me how you’ll take your blood pressure pill?"
If you say, "I take one in the morning and one at night," and they meant "one in the morning and one at bedtime," they’ll catch it right then. This method cuts misunderstandings by 33%.
You can use this yourself. Before leaving the pharmacy, say: "Just to make sure I got it right-I take this pill at [time], with [food/water], and I shouldn’t take more than [number] in a day. Is that correct?"
It takes 1-2 minutes. But it could save you from a hospital visit.
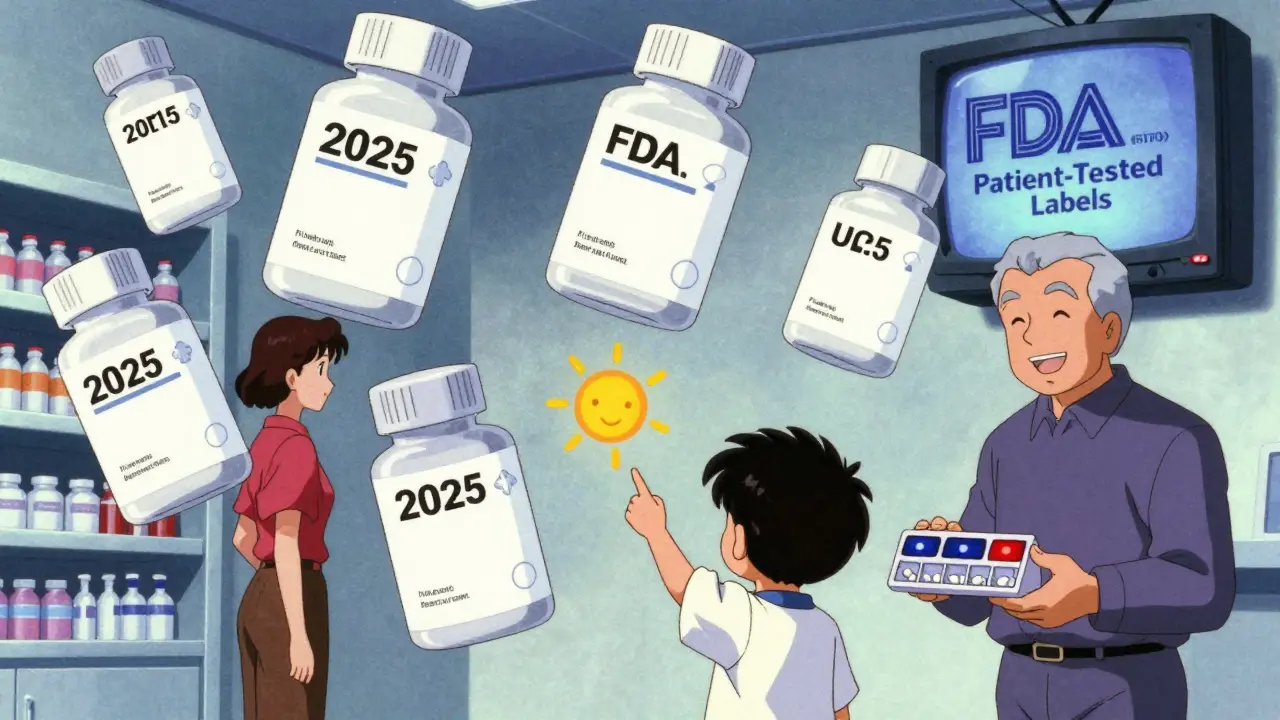
What’s Changing in 2025
The rules are finally catching up to the problem. By May 2025, all prescription labels in the U.S. must follow the USP’s new design rules: clear fonts, pictograms, plain language, and one-column layouts. The FDA is also requiring drugmakers to test labels with real patients-including those with low literacy-before they go on the market.Big hospitals and pharmacy chains are already ahead. But small clinics and rural pharmacies? Many still use old labels. That’s why your own vigilance matters.
Look for the new labels. If you see one with "morning, noon, evening, bedtime" and pictures of a sun, clock, and moon-great. That’s the new standard. If you still see "twice daily" or "q12h," ask for a plain-language version. You have the right to understand your meds.
What to Do If You’re Still Confused
You’re not alone. About 1 in 3 adults in the U.S. struggle to understand health information. Here’s what to do:- Ask your pharmacist to write the instructions on a sticky note.
- Use a pill organizer with labeled times.
- Set phone alarms for each dose.
- Bring a family member or friend to your next appointment.
- Call your pharmacy. No judgment. No rush. They’ve heard it all.
Don’t let pride keep you from asking. A mistake today could lead to a hospital stay tomorrow. And that’s not worth the risk.
Final Thought: You’re Not the Problem
The problem isn’t that you’re bad at reading. It’s that the system wasn’t built for you. Most labels were designed for doctors, not patients. But that’s changing. And you have power in this process.Next time you get a new prescription, pause. Read the label. Ask one question. Write it down. Use the teach-back trick. You’re not just following instructions-you’re protecting your health.
What does "take every 4-6 hours" really mean?
It means you can take the medicine anytime between 4 and 6 hours apart, not all at once. For example, if you take it at 8 a.m., your next dose can be between 12 p.m. and 2 p.m. Never take more than the maximum number of doses in 24 hours. If the label says "no more than 4 doses per day," that means you can’t take it more than four times, even if you space them out.
Can I use a kitchen spoon to measure liquid medicine?
No. A kitchen teaspoon holds about 5 mL, but it’s not accurate. A tablespoon might hold 15-20 mL. Always use the measuring cup, syringe, or dosing spoon that comes with the medicine. If you lost it, ask your pharmacy for a new one-they’ll give it to you free.
Why do some labels say "take with food" and others say "take on an empty stomach"?
Some medicines work better when your stomach has food-it helps them absorb or reduces nausea. Others need an empty stomach so food doesn’t block their effect. "With food" means eat a snack or meal around the same time. "On an empty stomach" means no food for at least 1 hour before and 2 hours after. If you’re unsure, ask your pharmacist.
What if I miss a dose?
Don’t double up. If you miss a dose and it’s almost time for the next one, skip the missed one. If you realize you missed it earlier in the day, take it right away. But if it’s been more than half the time until your next dose, skip it. Always check the label or call your pharmacist-some meds have different rules.
How do I know if my medicine is expired?
Check the expiration date on the bottle or box. It’s usually written as "EXP MM/YY" or "Expires MM/YYYY." Never use medicine past that date. Expired pills can lose strength or even become harmful. If you’re unsure, take it to your pharmacy-they’ll dispose of it safely.
Next Steps for Safer Medication Use
Start today. Grab your most recent prescription bottle. Read the label. Ask yourself: Could someone with low literacy understand this? If not, you’re not alone-and you’re not failing. The system is.Call your pharmacy. Ask for a plain-language version. Request a pill organizer. Set alarms. Write down your questions. Bring someone with you to your next appointment. These small actions add up.
Health literacy isn’t about being smart. It’s about being supported. And you deserve to understand your medicine without guessing.





So many of us have been there-staring at a pill bottle like it’s a cryptic hieroglyph. I once gave my grandma the wrong dose because I thought 'q6h' meant 'every 6 hours, so 4 times a day'-turns out it was 'every 6 hours, max 4 doses.' She ended up in the ER. No one ever explained it. We just assume labels are clear. They’re not. And it’s not our fault.
What really hits me is how little design thinking goes into this. If a coffee cup had instructions this confusing, we’d sue the company. But when it’s your heart medication? You just nod and take it. That’s broken.
I started printing out plain-language versions of my meds and taping them to the fridge. My mom does the same. We even made a little chart with suns and moons. It’s silly, but it works. Why don’t pharmacies just hand these out? They’re free. They’re simple. They save lives.
And don’t even get me started on the kitchen spoon thing. I used to eyeball liquid meds with a soup spoon. I thought 'teaspoon' meant the one you stir coffee with. Turns out, that’s not even close. Now I keep a syringe in my purse. I carry it like a weapon. Because I will not let my family die because of a measurement error.
It’s not about being smart. It’s about being treated like a human. And honestly? We deserve better.
Labels are designed by bureaucrats who’ve never had to take five pills a day while grieving their mom and barely sleeping
They think 'twice daily' is clear because they’re not tired or in pain or dyslexic or just plain exhausted
It’s not the patient’s job to decode medical gibberish
It’s the system’s job to speak human
I’m from South Africa and we’ve got the same problem here. Pharmacies still use tiny print and Latin abbreviations. One time my uncle took his blood pressure pill at 8am and then again at 10am because he thought 'every 4-6 hours' meant 'if you feel bad, take one.' He ended up with a scary drop in BP.
What helped was when his clinic started using pictograms-sun for morning, moon for night. Simple. No reading needed. I wish every pharmacy here had that. We don’t need fancy apps. We need pictures.
And yes, never use a kitchen spoon. I learned that the hard way. Now I keep a little plastic doser in my wallet. Like a Swiss Army knife for meds.
From a clinical pharmacology standpoint, the cognitive load imposed by non-standardized labeling is a significant contributor to non-adherence and iatrogenic harm. The prevalence of misinterpretation of temporal qualifiers such as 'q12h' versus 'twice daily' is well-documented in the literature-studies by Davis et al. (2009) and the American Medical Association’s Health Literacy Task Force corroborate these findings. The Universal Medication Schedule (UMS) represents a paradigm shift toward patient-centered communication, reducing cognitive dissonance by anchoring dosing to circadian rhythms rather than abstract temporal intervals. Furthermore, the integration of pictorial cues aligns with dual-coding theory, enhancing recall through visuospatial encoding. The FDA’s impending regulatory mandates are not merely bureaucratic overreach-they’re evidence-based interventions grounded in behavioral science. Failure to adopt these standards constitutes a systemic violation of the duty of care owed to patients with low health literacy.
OH MY GOD YES. I JUST HAD A MOMENT WHERE I THOUGHT 'TAKE EVERY 8 HOURS' MEANT THREE TIMES A DAY AND I WAS SO PROUD OF MYSELF FOR 'FIGURING IT OUT' UNTIL I REALIZED I WAS TAKING IT AT 6AM, 2PM, AND 10PM-AND THAT'S FOUR TIMES. I'M A COLLEGE GRADUATE. I CAN DO MATH. BUT I DIDN'T KNOW. NO ONE TOLD ME. WHY IS THIS SO HARD?
AND WHY DO PHARMACISTS STILL SAY 'TAKE AS DIRECTED' LIKE THAT'S A THING? IT'S NOT A THING. IT'S A COP-OUT.
I STARTED TAKING PICTURES OF MY LABELS AND PUTTING THEM IN MY NOTES APP. NOW I HAVE A 'MEDS FOLDER' AND I SHOW IT TO MY DOCTOR. SHE THINKS I'M A NUT. I SAY, 'NO, YOU'RE THE NUT. YOU'RE THE ONE WHO THINKS THIS IS CLEAR.'
WE NEED TO STOP BLAMING PEOPLE AND START FIXING THE SYSTEM. LIKE, TODAY.
As someone who’s worked in community health across three continents, I’ve seen this play out in rural clinics in Nigeria, urban pharmacies in Detroit, and even in refugee camps in Jordan. The issue isn’t language-it’s context. A label that makes sense in a high-income country with universal healthcare access might as well be written in ancient Sumerian in a place where people don’t have clocks, refrigerators, or consistent electricity.
What’s often overlooked is that health literacy isn’t just about reading-it’s about infrastructure. If you don’t have a phone to set alarms, or a fridge to store insulin, or a family member to double-check your meds, even the clearest label won’t help.
That’s why the UMS and pictograms are good, but not enough. We need community health workers. We need home visits. We need systems that meet people where they are-not where we wish they were.
And yes, I’ve seen people use kitchen spoons. I’ve seen them use bottle caps. I’ve seen them guess. We need to stop pretending this is just a 'patient education' problem. It’s a design failure. A policy failure. A moral failure.
In many African societies, the concept of individual medical responsibility is deeply intertwined with familial and communal roles. When a child is given medicine, it is often the grandmother, aunt, or neighbor who administers it-not the parent. The label, therefore, must speak not just to the patient, but to the entire network of caregivers.
One clinic I worked with in Lagos introduced large, color-coded cards with pictograms and local proverbs: 'Morning sun wakes the body, take your pill.' 'Night moon rests the soul, take your last dose.' The results were profound. Illiteracy rates didn’t change. But adherence did.
What we’re missing in the West is the wisdom of collective care. We treat health as a solitary act. But healing is a village project. If your label doesn’t account for that, it’s not just unclear-it’s culturally blind.
And yes, I’ve seen people use spoons. But I’ve also seen them use a hollowed-out calabash, a plastic straw, even a child’s toy cup. The problem isn’t the spoon. The problem is that no one ever asked: 'How do you measure things at home?'
Design must begin with listening. Not with assumptions.
I used to think I was just bad at remembering stuff. Then I realized I was just bad at reading labels. I’ve been on the same blood pressure med for 5 years and I still mix up 'take with food' and 'take on empty stomach.' I finally asked my pharmacist to write it on a sticky note. She didn’t even blink. She said, 'I do this for everyone.'
Now I have a whole drawer of sticky notes. I put them on my mirror, my coffee maker, my car dashboard. I even put one on my dog’s food bowl because I forget to eat sometimes.
And guess what? I haven’t missed a dose in 18 months. It’s not magic. It’s just writing it down.
Don’t be ashamed to ask. Don’t be proud. Just ask. And if they don’t write it down for you? Ask again. And again. Because your life matters more than their hurry.
My mom had a stroke last year and she’s on 12 different meds. We sat down with her pharmacist for an hour. He didn’t just hand her a bottle-he drew a chart. Sun for morning, moon for night, a little heart for the blood thinner, a little lung for the inhaler. We laminated it. She carries it in her purse.
She still forgets sometimes. But now she knows to say, 'Can you show me again?' and he doesn’t make her feel stupid.
That’s the thing no one talks about: it’s not just about the label. It’s about the person behind it. The pharmacist who takes the time. The doctor who doesn’t rush. The family member who asks, 'What does this mean?'
We need more of that. Not just better labels. Better humans.
It is imperative to underscore the ethical obligation incumbent upon pharmaceutical manufacturers, regulatory bodies, and healthcare providers to ensure that medication labeling adheres to universally accessible standards of legibility, clarity, and comprehensibility. The current state of affairs constitutes a systemic failure in the fulfillment of the principle of informed consent, as patients are not provided with information in a manner that permits autonomous decision-making. The adoption of the Universal Medication Schedule, coupled with standardized pictorial iconography and typographic hierarchy, represents not merely a best practice, but a moral imperative. To neglect such measures is to perpetuate health disparities rooted in linguistic, cognitive, and socioeconomic inequities. It is not sufficient to merely comply with regulatory mandates; one must strive for excellence in patient communication as a foundational tenet of medical ethics.
Okay but have you seen the new label on my antidepressant? It says 'take once daily' and has a little sun and a little moon and a little person sleeping with a thought bubble that says 'BEDTIME' and I just cried. Not because I’m sad. Because someone finally thought, 'maybe this person doesn’t know what 'daily' means.'
And the font? It’s HUGE. Like, I can read it without glasses. And the active ingredient? It’s on the front. Not buried under 12 other words.
I didn’t think the system could change. I thought I was just broken. Turns out, the system was broken. And now it’s fixing itself.
Thank you to whoever designed this. You saved my life.
Also, I now carry a syringe in my bra. No regrets.
Just saw a new label today. Sun. Moon. Clock. No 'twice daily.' Just 'morning, evening.' I smiled. For the first time in years, I didn’t have to call my pharmacist. I just looked. I got it.
Small thing. Big deal.