Steroid Infection Risk Calculator
This calculator estimates your risk of serious infection based on your corticosteroid dosage and treatment duration. Use it to understand when preventive measures become critical.
Why Corticosteroids Make You More Susceptible to Infections
When you take corticosteroids like prednisone or dexamethasone for conditions like rheumatoid arthritis, lupus, or severe asthma, you’re not just calming inflammation-you’re also turning down your body’s natural defense system. These drugs mimic cortisol, the hormone your adrenal glands make to help manage stress and immune responses. But when you take them in doses higher than your body naturally produces-often 10 mg or more per day-you’re not just tweaking your immune system. You’re shutting down key parts of it.
That’s why people on long-term steroids get sick more often. Not just colds, but serious infections you’d normally never see: Pneumocystis pneumonia, reactivated tuberculosis, invasive fungal infections, and shingles. The problem isn’t that steroids make you weak. It’s that they make your immune system forget how to fight certain threats-especially viruses and fungi that hide inside cells.
How Steroids Break Down Your Immune Defenses
Corticosteroids don’t attack your whole immune system. They pick and choose. The biggest damage happens to your T cells-the soldiers that hunt down infected or cancerous cells. At high doses, steroids cause these cells to die off or stop moving around the body. Your lymphocyte count drops, sometimes below 1,000 cells per microliter. That’s a red flag: your body can’t mount a proper response to new threats.
Macrophages, the cleanup crew that swallows up bacteria and signals other immune cells, also get slowed down. They stop showing infected cells to T cells. They stop producing the alarm signals (cytokines) that tell your body to fight back. Meanwhile, neutrophils-the first responders to bacterial infections-actually increase in number, but they’re less effective at sticking to blood vessel walls and reaching infection sites.
Here’s what doesn’t get hit much: your B cells and antibody production. That means you still make antibodies against things like tetanus or measles if you’ve been vaccinated. But if a virus hides inside your lung cells or a fungus grows in your sinuses, your T cells aren’t there to find and kill it. That’s why steroid users get opportunistic infections-they’re the kind your immune system normally keeps under control, but can’t handle when T cells are silenced.
Dose and Duration Are Everything
Not every steroid user gets a serious infection. But the risk climbs fast once you cross certain thresholds. If you’re taking 20 mg of prednisone-or the equivalent in other steroids-every day for more than 3 to 4 weeks, your infection risk jumps dramatically. Each extra 10 mg per day increases your chance of a serious infection by about 32%, according to a 2022 analysis of over 100,000 patients.
That’s not theoretical. In the U.S., 1.2% of adults are on systemic steroids at any given time. Among them, about 1 in 20 will develop a serious infection within a year if they’re on high doses. Pneumocystis pneumonia, once rare, now accounts for nearly 19% of all cases in immunocompromised people. And when it’s missed, death rates hit 30-50%.
Tuberculosis is another silent threat. In countries where TB is common, people on steroids have up to a 7.7 times higher risk of reactivating a latent infection. That’s why screening before starting steroids isn’t optional-it’s life-saving.
What You Can Do to Prevent Infections
Prevention isn’t about avoiding steroids. It’s about using them smarter. Here’s what works:
- Get screened for TB before starting steroids if you’re on 15 mg or more of prednisone daily for longer than a month. A blood test (IGRA) or skin test can catch latent TB. If positive, a 9-month course of antibiotics reduces reactivation risk by 90%.
- Take PJP prophylaxis if you’re on 20 mg or more of prednisone for 4 weeks or longer. Trimethoprim-sulfamethoxazole (Bactrim) cuts the risk of Pneumocystis pneumonia from 5% to under 1%.
- Update your vaccines before starting steroids. Get pneumococcal, flu, and COVID-19 shots at least two weeks ahead of time. Once you’re on high-dose steroids, your body won’t respond well-studies show only 42% of patients on >20 mg prednisone develop protective antibodies after flu shots, compared to 78% in healthy people.
- Avoid live vaccines entirely while on steroids. That includes MMR, chickenpox, nasal flu spray, and yellow fever. These can cause infection in a suppressed immune system.
Watch for Silent Infections
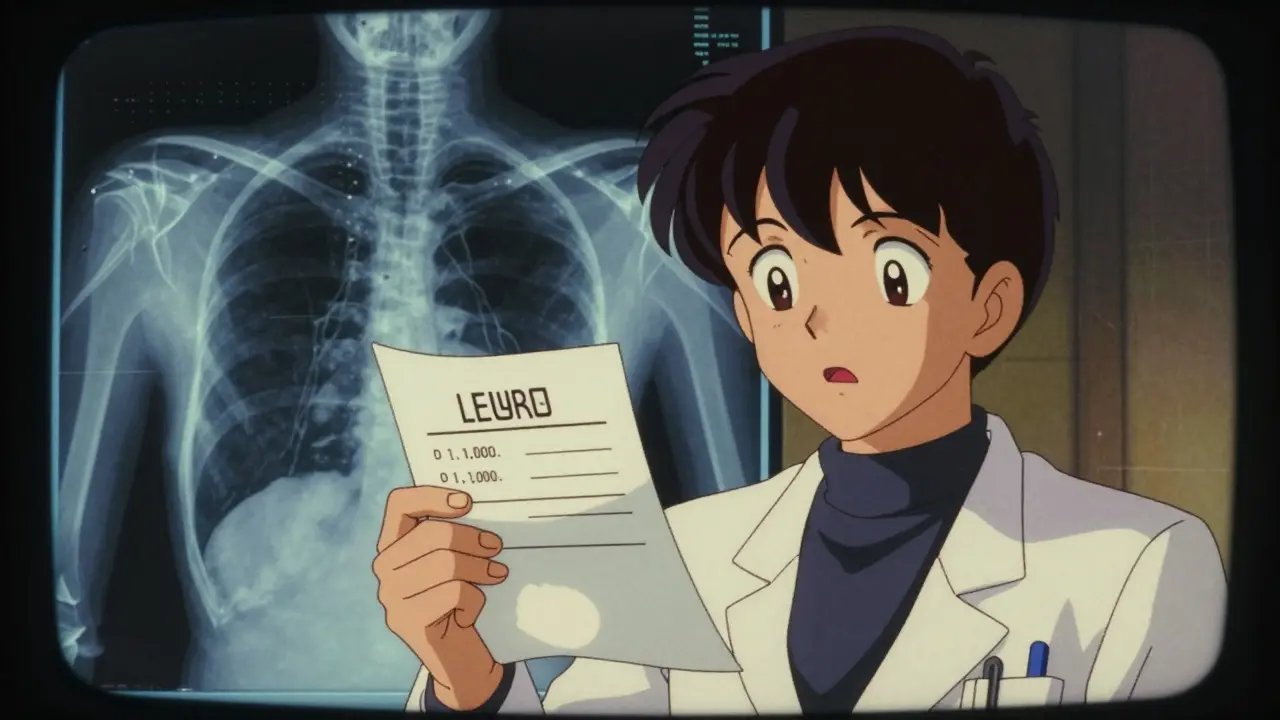
One of the scariest things about steroid use is how infections hide. Fever? Sometimes absent. Redness? Often missing. Cough? Could be nothing-or it could be PJP. Because steroids blunt inflammation, your body doesn’t give you the usual warning signs.
That’s why doctors need to think differently. If you’re on steroids and feel off-even a little-don’t wait. Get checked. A chest X-ray, blood cultures, or a CT scan might be needed. In one study, 40% of patients with serious infections on steroids didn’t have a fever. That’s not normal. It’s a red flag.
Shorter Is Better. Lower Is Safer.
The best way to avoid infection? Use the lowest dose for the shortest time possible. That’s not just advice-it’s backed by data. Rapid tapering, where doctors reduce steroids faster than traditional protocols, cuts infection risk by 37%. Some patients switch to steroid-sparing drugs like methotrexate or biologics within 4 weeks. One Reddit user shared: “My rheumatologist switched me to methotrexate after 3 months on prednisone. No flares. No colds.”
That’s the goal: control your disease without putting your life at risk. Steroids are powerful, but they’re not the only tool. Modern rheumatology now pushes for combination therapy-steroids as a bridge, not a lifetime solution.

Monitoring and Patient Education Save Lives
Doctors should check your blood count every 2-4 weeks while you’re on high-dose steroids. A lymphocyte count under 1,000 means you’re at higher risk. In TB-endemic areas, monthly chest X-rays are recommended after 3 months of therapy.
But the most powerful tool? Education. Patients who learned what symptoms to watch for-fever, night sweats, shortness of breath, unexplained fatigue-had 28% fewer hospitalizations. Knowing when to call your doctor matters more than you think.
The Future: Safer Steroids and Personalized Risk
Research is moving fast. A new type of steroid called vamorolone, tested in Duchenne muscular dystrophy, gave the same anti-inflammatory effect as prednisone but with 47% fewer infections. It’s designed to separate the good effects (reducing inflammation) from the bad (killing immune cells).
Soon, doctors may use genetic tests to predict who’s more likely to get infections on steroids. Some people naturally have weaker T-cell responses. For them, prophylaxis might start at lower doses. Others might handle steroids fine. This is the future: personalized treatment, not one-size-fits-all.
Bottom Line: Steroids Are Necessary-But Not Without Caution
Corticosteroids saved lives when they were first used in 1948. They still do. But today, we know more about how they work-and how dangerous they can be if used carelessly. The key isn’t to avoid them. It’s to use them with eyes wide open.
Screen before you start. Prophylax when needed. Vaccinate early. Taper fast. Watch for silent infections. And always, always ask: Is this the lowest dose I can get away with?
With the right precautions, you can control your disease without becoming a statistic. Millions of people do it every day. You can too.
Can I still get vaccinated while on corticosteroids?
You can get inactivated vaccines like flu, pneumonia, and COVID-19 while on steroids, but they may not work as well if you’re on high doses (20 mg prednisone or more). The best time to get them is at least 2 weeks before starting steroids. Live vaccines-like MMR, chickenpox, or nasal flu spray-are unsafe and should be avoided entirely while immunosuppressed.
How do I know if I have an infection while on steroids?
Don’t wait for fever or redness-they often don’t show up. Look for unexplained fatigue, night sweats, shortness of breath, persistent cough, new skin rashes, or worsening joint pain. Even mild symptoms can signal a serious infection. If you’re on long-term steroids and feel off, get checked immediately. Delayed diagnosis can be deadly.
Is it safe to take prednisone for more than a few months?
Long-term use increases infection risk significantly, especially above 20 mg per day. But sometimes it’s necessary. The goal isn’t to stop steroids completely-it’s to use them as a bridge. Doctors should aim to add steroid-sparing drugs like methotrexate or biologics within 4 weeks to reduce the need for ongoing high doses. Many patients successfully transition off steroids with no flare-ups.
Do I need PJP prophylaxis if I’m on 10 mg of prednisone daily?
No. Prophylaxis with trimethoprim-sulfamethoxazole is recommended only if you’re on 20 mg or more of prednisone (or equivalent) for 4 weeks or longer. At 10 mg, your risk is low unless you have other immune problems like HIV or cancer. Always discuss your personal risk with your doctor.
Can corticosteroids cause reactivation of old infections like herpes or TB?
Yes. Steroids suppress T-cell immunity, which normally keeps latent viruses and bacteria in check. Herpes zoster (shingles) reactivates 2-3 times more often in steroid users. TB can flare up even years after exposure, especially if you lived in or traveled to a high-risk area. Screening before starting steroids is essential to prevent this.






This is such a helpful breakdown. I’ve been on prednisone for 6 months and honestly didn’t realize how sneaky infections could be. No fever? Okay then I’m fine? Nope. Learned the hard way. Thanks for the clarity.
T cell suppression is the real villain here not the steroid itself. The drug doesn’t cause infection it disables the surveillance system that keeps opportunistic pathogens in check. Lymphocyte count under 1000 is the red zone. Period. No debate.
The claim that 32% increased infection risk per 10 mg is misleading. That’s from a retrospective cohort study with massive confounding. You’re comparing sicker patients on higher doses to healthier ones on low doses. Correlation isn’t causation. The real culprit is disease severity not the drug.
I got PJP prophylaxis after 6 weeks on 20mg. Still got a bad cough but I knew to push for a CT scan. Turned out to be fungal. Early detection saved me. 🙏
For anyone reading this and feeling overwhelmed: you’re not alone. Many of us are walking this tightrope. Your doctor isn’t just prescribing meds they’re trying to balance your life. Ask questions. Track symptoms. You’ve got this.
The biggest issue I see is how many patients are left in the dark until they’re hospitalized. Steroid education should be mandatory like a driver’s ed course. You get a pamphlet on side effects and then you’re on your own. That’s not care that’s negligence. We need structured patient pathways not just handouts. Every clinic should have a 15 minute steroid safety briefing before the first script is written. It’s not optional anymore.
This whole thing is Big Pharma’s trap. Steroids are cheap and profitable. They push them because they know you’ll need more drugs later to fix what they broke. Vaccines? Prophylaxis? All money grabs. You don’t need all this. Just stop the steroids. Your body knows how to heal.
I was on 40mg for 3 months. Got shingles. My doc said it was expected. I said no way I’m not getting this again. Switched to Humira. Zero flares. Zero infections. Best decision of my life. If you’re on high dose for more than 6 weeks you’re playing Russian roulette with your immune system.
They’re lying about the TB screening. The IGRA test is unreliable. I had a false negative. Got reactivated TB 8 months later. The CDC knows this. They just don’t say it. You think they care about you? They care about liability. Get a chest X-ray. Every time. Don’t trust the blood test.
The future is vamorolone. It’s not magic but it’s the first real step toward separating the good from the bad in steroids. Imagine not having to choose between controlling your disease and staying alive. We’re not far from that. Keep pushing for better science. We’re getting there.
You people are so naive. You trust doctors. You take their pills. You get your shots. You follow every rule. But who controls the guidelines? Who funds the studies? Who decides what’s safe? You’re being manipulated. Wake up.
I just got off prednisone after 18 months. Lost 30 pounds. Got pneumonia twice. My husband said I looked like a ghost. My doctor said I was lucky to be alive. Now I’m on methotrexate. Still tired. Still scared. But alive. And I’m not taking any more steroids unless I’m dying.