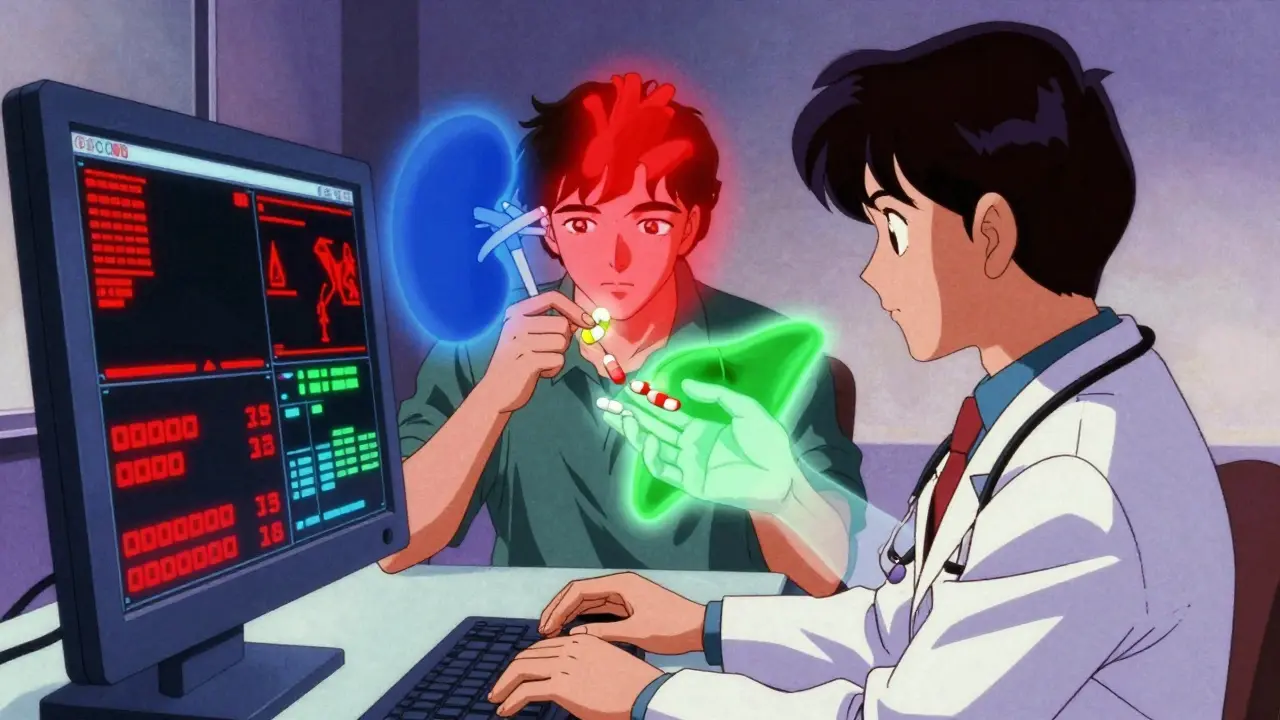
Think your medication is safe just because your doctor prescribed it? What if your other health conditions are quietly making that drug dangerous? This isn’t rare. It’s happening right now to millions of people taking pills for one thing while their other illnesses turn those same pills into hidden risks.
What Exactly Is a Drug-Disease Interaction?
A drug-disease interaction happens when a medication meant to help one condition makes another condition worse. It’s not about mixing two drugs. It’s about how your body’s existing problems change how a drug works-sometimes in deadly ways.
For example, beta-blockers like metoprolol are common for high blood pressure and heart disease. But if you also have asthma, these drugs can tighten your airways and trigger a serious attack. Or take NSAIDs like ibuprofen for joint pain. If you have heart failure, they can cause your body to hold onto salt and water, making swelling and shortness of breath worse. These aren’t side effects you read about on the label. They’re hidden traps built into your own health history.
The American Society of Health-System Pharmacists says chronic kidney disease, heart failure, liver disease, and psychiatric conditions cause nearly 80% of serious drug-disease interactions. These aren’t edge cases. They’re everyday realities for older adults and people with multiple long-term conditions.
How Do These Interactions Actually Happen?
There are five main ways a disease can turn a good drug into a bad one:
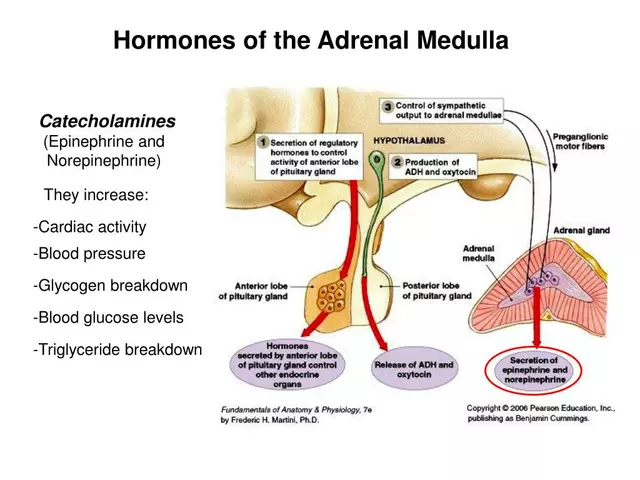
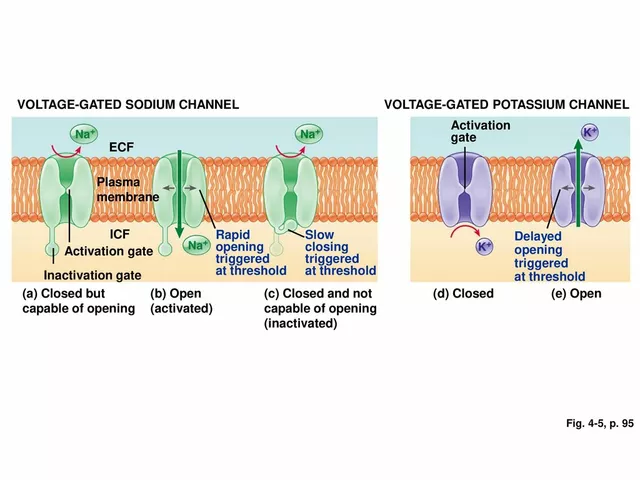
- Pharmacodynamic interference: The drug’s action directly fights your disease. Beta-blockers can hide low blood sugar symptoms in diabetics. You won’t feel shaky or sweaty-until you pass out.
- Pharmacokinetic changes: Your disease alters how your body processes the drug. Liver disease slows down how fast warfarin breaks down. That means even a normal dose can make your blood too thin, risking internal bleeding.
- Masking symptoms: The drug hides warning signs. Diuretics for high blood pressure can make you feel fine while your kidneys are failing. You won’t know something’s wrong until it’s too late.
- Exacerbating complications: The drug worsens existing damage. Metformin for type 2 diabetes can cause lactic acidosis if your kidneys are already weak. That’s not a side effect-it’s a direct result of your disease.
- Direct organ toxicity: The drug harms an organ already struggling. Lithium for bipolar disorder builds up in your body if your kidneys aren’t filtering well. Toxic levels can cause seizures or coma.
It’s not just about one drug. It’s about the combination of your health conditions and the medications you’re taking. A person with diabetes, heart failure, and depression might be on seven different pills. Each one could interact with one or more of their conditions.
Who’s at the Highest Risk?
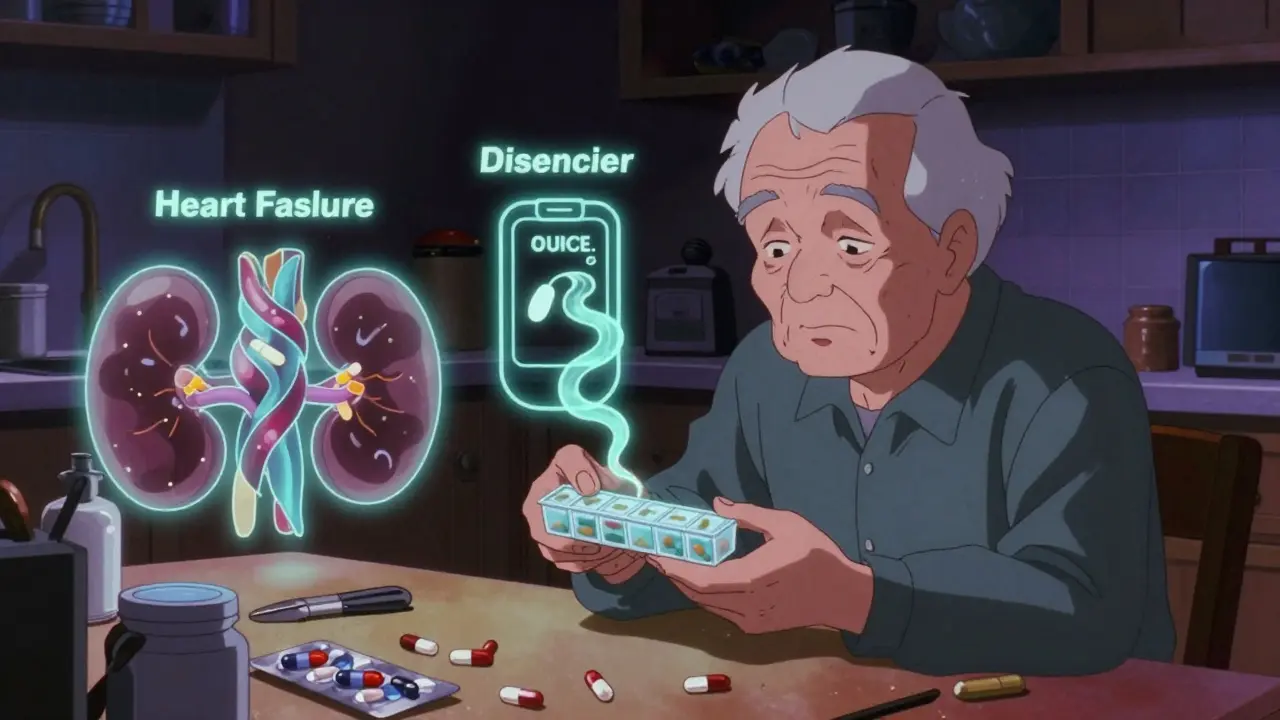
If you’re over 65, you’re at higher risk. The average older adult in the U.S. takes 5.4 medications daily and has 4.7 chronic conditions. That’s a recipe for hidden clashes.
But it’s not just age. People with:
- Chronic kidney disease (CKD): 84% of dangerous drug-disease interactions in diabetes guidelines involve CKD.
- Heart failure: NSAIDs, certain anti-inflammatories, and even some diabetes drugs can make fluid retention worse.
- Liver disease: Many drugs are broken down by the liver. If it’s damaged, those drugs build up to toxic levels.
- Depression or anxiety: SSRIs can increase bleeding risk, especially if you’re also on blood thinners or have ulcers.
- Diabetes: Drugs that lower blood sugar can hide the warning signs-making hypoglycemia silent and deadly.
And it’s not just prescription drugs. St. John’s wort, a popular herbal supplement for mood, can trigger life-threatening serotonin syndrome when mixed with antidepressants. Many people don’t even think of supplements as drugs-but they are.
Why Are These Interactions So Often Missed?
Doctors aren’t ignoring you. The system is broken.
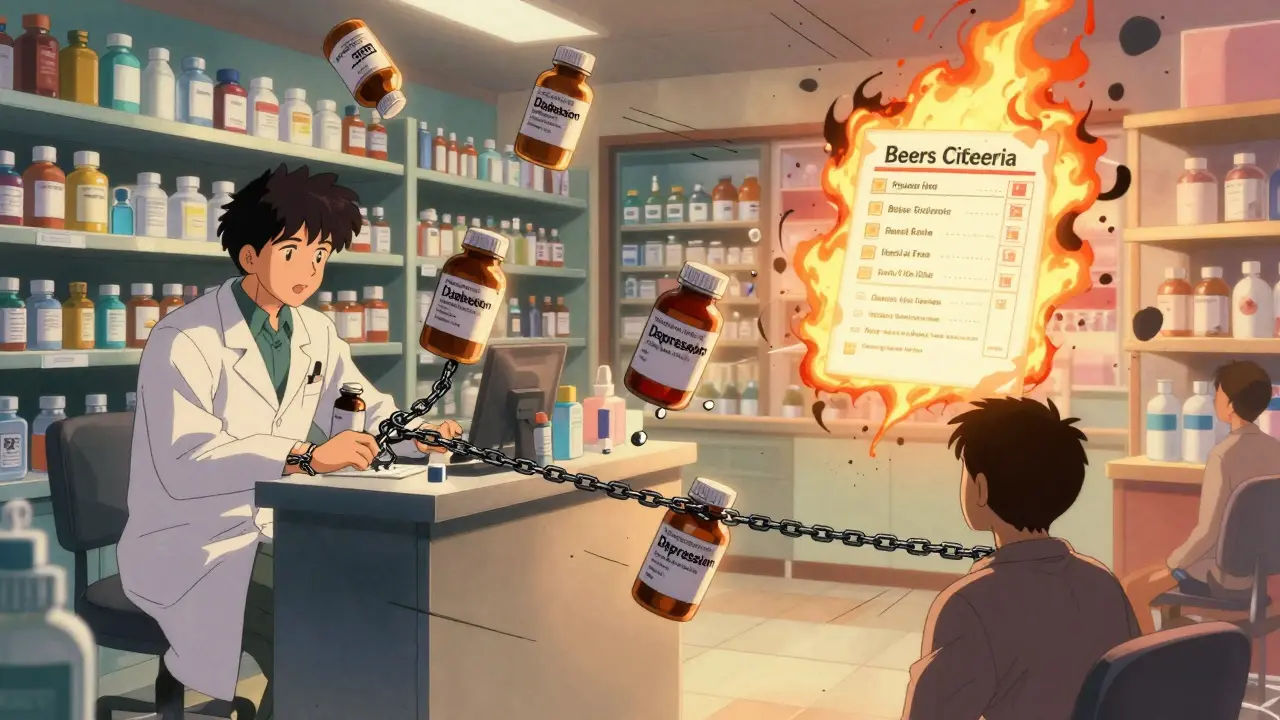
A 2020 review found that fewer than 16% of clinical guidelines for common conditions like diabetes, depression, or heart failure include clear warnings about drug-disease interactions. That means if your doctor follows the guideline exactly, they might not even know they’re putting you at risk.
Electronic health records (EHRs) are supposed to help. Epic’s system flags 87% of high-risk interactions-but 42% of those are false alarms. Doctors start ignoring alerts. They get alert fatigue. And when that happens, the real dangers slip through.
Pharmacists spend nearly 13 minutes per patient checking for these interactions. But in a busy pharmacy, that’s not always possible. A 2021 survey found 68% of pharmacists say they don’t have enough time to do proper screening during routine dispensing.
And patients? A survey from Village Medical showed only 22% of people with high blood pressure understood why a common cold medicine like pseudoephedrine could spike their blood pressure. They took it because it was “over-the-counter.” That’s not ignorance. It’s a lack of clear, simple education.
What Can You Do to Protect Yourself?
You don’t need to be a medical expert. But you do need to be an active participant in your care.
Here’s what works:
- Keep a full, updated list of everything you take: Prescriptions, over-the-counter meds, vitamins, supplements, and even herbal teas. Bring this list to every appointment-even if you think it’s obvious.
- Ask one simple question at every visit: “Could any of these medications make my other conditions worse?” Don’t wait for your doctor to bring it up.
- Know your kidney and liver numbers: If you have heart failure, diabetes, or high blood pressure, ask for your eGFR (kidney function) and liver enzyme tests at least once a year. These numbers change. Your meds might need to change too.
- Use the Beers Criteria: This is a trusted list of medications that are risky for older adults with certain conditions. You can look it up online. If your doctor prescribes something on it, ask why.
- Review your meds every six months: Not just when you’re sick. Ask your pharmacist or doctor: “Is everything I’m still taking still necessary?” Many people keep taking pills long after they’re needed.
Some clinics now have specialized drug-disease interaction teams. Mayo Clinic reported a 27% drop in hospital readmissions after setting one up. That’s not magic. That’s better screening.
What’s Changing in the Medical World?
The tide is turning-slowly.
The FDA now requires drug makers to test how their medications affect patients with common comorbidities. That’s new. In the past, clinical trials mostly used healthy volunteers. Now, they have to include people with kidney disease, liver problems, and heart failure.
The 2023 update to the Beers Criteria added 12 new warnings, including avoiding anticholinergics in dementia patients and opioids in people with COPD. These aren’t theoretical. These are based on real-world data from hundreds of thousands of patients.
Machine learning is getting better at predicting these interactions. A 2023 study from the University of Toronto used AI to analyze 157 clinical factors and predicted dangerous interactions with 89% accuracy-far better than old rule-based systems.
And the NIH’s All of Us program is linking genetic data with health records to predict who’s most at risk. In the next five years, your risk profile might be built into your electronic chart before your doctor even opens it.
But here’s the catch: these tools won’t help if they’re not used. Hospitals are being fined for medication errors under Medicare’s Hospital-Acquired Condition Reduction Program. That’s pushing change. But without patient involvement, technology alone won’t save lives.
It’s Not About Avoiding Medicine-It’s About Using It Wisely
Medications save lives. But they’re not harmless. Every pill you take has a double-edged nature: it helps one thing, but might hurt another.
The goal isn’t to stop taking your meds. It’s to make sure they’re working for you-not against you.
If you’re managing multiple conditions, you’re not alone. But you need to be your own advocate. Ask the questions. Know your numbers. Keep your list updated. And don’t assume your doctor knows everything about how your conditions interact with your meds.
Because in the end, your health isn’t just about what’s in the bottle. It’s about how that bottle fits into the rest of your body-and your life.



lol so now i gotta memorize every drug and every disease like its a video game cheat code? my doctor already forgets what i take and i'm supposed to be the pharmacist now? thanks for the guilt trip
I just want to say thank you for writing this. I'm 72 and on 8 meds and I didn't realize how many of them were secretly making my heart worse. I went to my pharmacist yesterday and asked the question you said to ask and she cried. She said she's seen so many people almost die because no one ever asked. You're right. We have to speak up. I'm printing this out and bringing it to my next appointment. You're a light in the dark.
this is why america is falling apart. we let the government and big pharma tell us what to take and now we're all walking chemical soups. if you want to be healthy just eat real food and stop taking pills. the system is rigged and you're just a pawn
you know what's wild? in Nigeria we don't even have half these drugs. we take one pill for high blood pressure and one for diabetes and we live. no fancy AI, no 13-minute pharmacist checks. just survival. y'all over here with 12 pills and a spreadsheet and still dying. maybe the problem isn't the interaction... it's the obsession with treating everything.
i had a stroke last year and now i take like 10 pills and i just found out that the blood thinner i take makes my diabetez worse? wait what? my doctor never said that. i thought the pills were just fixing me not making new problems. this is insane. i need to call my pharmacist now
Let me just say this: the fact that you're even considering taking a supplement like St. John’s wort without knowing its pharmacokinetic profile is a moral failure. You're not a patient. You're a liability. If you can't understand the difference between pharmacodynamic interference and pharmacokinetic changes, you shouldn't be allowed to hold a pill bottle. This isn't a blog. It's a public health emergency.
It is profoundly concerning that society has come to view medication as a panacea rather than a precisely calibrated tool. The erosion of personal responsibility in health management is not merely a clinical oversight-it is a cultural collapse. We have outsourced our bodily autonomy to algorithms and overworked clinicians who are themselves drowning in systemic neglect. The solution is not more technology. It is discipline. It is vigilance. It is the refusal to accept mediocrity in one’s own care.
This is one of those posts that makes you pause and think about how fragile our bodies really are. I used to think meds were like vitamins-you take them and they just work. But reading this? It’s like realizing your car’s engine doesn’t care what kind of gas you put in if the transmission’s already broken. I started asking my doctor the question you mentioned. She paused. Then said, 'I wish more people asked that.' Turns out, she didn’t even know my blood pressure med was making my sleep apnea worse. We’re all just guessing. But now I’m not.
Oh wow. Another self-help article telling people they’re dumb for not reading 10-page PDFs about drug interactions. Let me guess-your doctor also told you to 'drink more water' and 'get more sleep' while you were dying of liver failure? How noble. How brave. How utterly useless. The real problem? Doctors don’t care. They’re paid to prescribe, not to think. And you? You’re just here to feel better about your own guilt.
The AI predictive models mentioned are statistically significant, yes-but they’re still trained on datasets that exclude 87% of the global population. The Beers Criteria? A Western artifact. The entire framework assumes you have access to eGFR tests, a pharmacist, and an EHR that doesn’t crash every Tuesday. This isn’t medicine. It’s a luxury diagnostic service for the insured. The rest of us? We’re just collateral.
i took a nap after my 3rd pill today and woke up with my heart doing the cha-cha. turns out my anxiety med + my blood pressure med + my weird herbal tea from my auntie = my body became a war zone. i didn't even know tea could be a drug. now i'm scared to drink coffee. or breathe. thanks for the enlightenment, doc
It is imperative that patients maintain a meticulously updated medication reconciliation list, presented in triplicate, and reviewed during every clinical encounter. Failure to do so constitutes negligence on the part of the individual, regardless of systemic failures. The responsibility for therapeutic safety rests unequivocally with the patient. This is not a suggestion. It is a standard of care.
you think this is bad? in india we have 30 people in one room with 1 doctor and 1 nurse. if you take 2 pills and live? you win. if you die? at least you didn't pay for it. why are you all so soft? we don't have time for your lists and your eGFRs. we just take the pill and hope. and guess what? we're still here.
i just realized i've been taking ibuprofen for my arthritis for 12 years and i have high blood pressure. no one ever told me that could be bad. i'm gonna go check my kidney numbers tomorrow. thanks for the wake up call