Elavil vs Alternative Antidepressants Comparison Tool
Recommended Alternatives Based on Your Needs
Side Effect Comparison Table
| Drug | Class | Typical Daily Dose | Key Benefits | Common Side-Effects | Pros vs Elavil |
|---|---|---|---|---|---|
| Elavil | TCAs | 75-150 mg | Effective for depression & neuropathic pain | Sedation, dry mouth, weight gain, cardiac QT prolongation | Baseline - strong analgesic effect |
| Nortriptyline | TCAs | 25-100 mg | Similar efficacy, less anticholinergic load | Less drowsiness, still some dry mouth, cardiac caution | Better tolerability, especially for older adults |
| Sertraline | SSRI | 50-200 mg | Low sedation, good for anxiety comorbidity | GI upset, mild sexual dysfunction, activation | Much lower cardiotoxic risk |
| Venlafaxine | SNRI | 75-225 mg | Strong effect on both serotonin & norepinephrine | Elevated blood pressure at high doses, nausea, insomnia | Better for patients needing both mood and pain relief |
| Duloxetine | SNRI | 30-60 mg | Proven for diabetic neuropathy & fibromyalgia | Dry mouth, constipation, increased liver enzymes | Targeted pain relief with manageable side-effects |
| Fluoxetine | SSRI | 20-80 mg | Very long half-life, low sedation | Insomnia, anxiety spike early in treatment | Ideal for patients who struggle with dosing consistency |
When you’ve been prescribed Elavil (Amitriptyline) and wonder if there’s a better fit, you’re not alone. Many patients ask about Elavil alternatives because the drug can bring troublesome side effects or simply doesn’t match their lifestyle. This guide walks you through the most common substitutes, compares how they work, and helps you decide which option aligns with your health goals.
What is Elavil and How Does It Work?
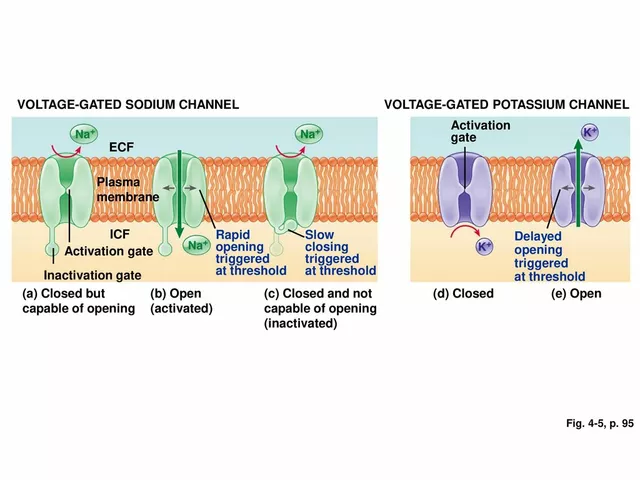
Elavil belongs to the class of tricyclic antidepressants (TCAs). It blocks the reuptake of serotonin and norepinephrine, boosting their levels in the brain. The result is mood improvement and pain relief for conditions like major depressive disorder, neuropathic pain, and migraine prophylaxis.
Typical adult dosing starts at 25mg at night, gradually increasing to 75-150mg per day, split into one or two doses. Because TCAs also affect histamine, acetylcholine, and cardiac ion channels, side effects such as drowsiness, dry mouth, weight gain, and heart rhythm changes are common.
Why Look for Alternatives?
Patients consider switching for several reasons:
- Persistent sedation or daytime drowsiness.
- Sexual dysfunction or weight gain.
- Interaction with other medications (e.g., blood thinners, antihistamines).
- Cardiac concerns, especially in older adults.
- Desire for a once‑daily pill with minimal side‑effects.
When any of these issues arise, a clinician may suggest a medication from a different class that targets the same neurotransmitters with a cleaner side‑effect profile.
Top Alternatives - Quick Overview
Below are the most frequently recommended substitutes, grouped by their pharmacological class.
- Nortriptyline - another TCA, but often better tolerated.
- Sertraline - a first‑generation selective serotonin reuptake inhibitor (SSRI).
- Venlafaxine - a serotonin‑norepinephrine reuptake inhibitor (SNRI).
- Duloxetine - another SNRI with strong evidence for chronic pain.
- Fluoxetine - an SSRI known for low sedation.

Side‑Effect Profiles at a Glance
| Drug | Class | Typical Daily Dose | Key Benefits | Common Side‑Effects | Pros vs Elavil |
|---|---|---|---|---|---|
| Elavil | TCAs | 75-150mg | Effective for depression & neuropathic pain | Sedation, dry mouth, weight gain, cardiac QT prolongation | Baseline - strong analgesic effect |
| Nortriptyline | TCAs | 25-100mg | Similar efficacy, less anticholinergic load | Less drowsiness, still some dry mouth, cardiac caution | Better tolerability, especially for older adults |
| Sertraline | SSRI | 50-200mg | Low sedation, good for anxiety comorbidity | GI upset, mild sexual dysfunction, activation | Much lower cardiotoxic risk |
| Venlafaxine | SNRI | 75-225mg | Strong effect on both serotonin & norepinephrine | Elevated blood pressure at high doses, nausea, insomnia | Better for patients needing both mood and pain relief |
| Duloxetine | SNRI | 30-60mg | Proven for diabetic neuropathy & fibromyalgia | Dry mouth, constipation, increased liver enzymes | Targeted pain relief with manageable side‑effects |
| Fluoxetine | SSRI | 20-80mg | Very long half‑life, low sedation | Insomnia, anxiety spike early in treatment | Ideal for patients who struggle with dosing consistency |
Decision‑Making Checklist
Use this quick list when you sit down with your doctor or pharmacist:
- Identify your primary goal: mood lifting, pain control, or both?
- Assess current side‑effects - are they sedation‑related, metabolic, or cardiac?
- Check for drug‑drug interactions (especially with anticoagulants or antihistamines).
- Consider age and cardiac health - older adults often benefit from Nortriptyline or an SSRI.
- Discuss dosing convenience - once‑daily agents like Fluoxetine simplify adherence.
- Ask about monitoring needs (e.g., blood pressure for Venlafaxine, ECG for TCAs).
Real‑World Scenarios
Case 1 - Chronic neuropathic pain with lingering drowsiness
Maria, 58, was on Elavil 100mg nightly for diabetic neuropathy. She reported daytime sleepiness that interfered with her part‑time job. Switching to Duloxetine 60mg daily reduced pain by 30% and eliminated the fog. Her doctor chose duloxetine because it has proven efficacy for nerve pain and a lower anticholinergic burden.
Case 2 - Depression with anxiety and a history of heart disease
James, 62, has mild heart failure. Elavil caused occasional palpitations. His cardiologist recommended an SSRI; his psychiatrist started Sertraline 100mg daily. Within four weeks, mood improved and anxiety subsided, without any cardiac events.
Case 3 - Need for a single‑dose regimen after travel
Lena, a 35‑year‑old consultant, travels weekly. She disliked splitting Elavil doses. Switching to Fluoxetine 40mg allowed once‑daily morning intake, and the long half‑life meant she missed a dose only once without rebound depression.

How to Transition Safely
Never stop Elavil abruptly - the drug can cause withdrawal symptoms like nausea, vivid dreams, and flu‑like aches. A typical taper looks like this:
- Reduce by 25mg every week (e.g., 150mg → 125mg → 100mg).
- Introduce the new medication at a low dose once the taper reaches 25mg.
- Monitor for overlapping side‑effects for two weeks before fully stopping the TCA.
Always coordinate with a prescriber who can perform ECGs if you stay on a TCA during the switch.
Cost Considerations (UK Context)
In 2025, most of the alternatives are available as generics on the NHS. Approximate annual costs when prescribed privately:
- Elavil - £120‑£150
- Nortriptyline - £80‑£110
- Sertraline - £70‑£100
- Venlafaxine - £90‑£130
- Duloxetine - £110‑£150 (brand) but generic versions can be £85‑£120
- Fluoxetine - £60‑£90
Check with your local pharmacy for any discount schemes or NHS prescription exemption certificates.
Final Thoughts
Choosing an Elavil substitute is a balance between therapeutic goals and tolerability. If sedation or cardiac risk is a deal‑breaker, look toward an SSRI like Sertraline or a newer SNRI such as Duloxetine. For patients who still need strong pain relief but want fewer anticholinergic effects, Nortriptyline can be a sweet spot.
Frequently Asked Questions
Can I switch from Elavil to an SSRI without a washout period?
A short washout isn’t usually required because both drugs act on serotonin pathways, but tapering Elavil by 25mg weekly reduces the risk of serotonin syndrome. Your doctor will tailor the schedule.
Is Nortriptyline safer for older adults than Elavil?
Generally, yes. Nortriptyline has a weaker anticholinergic effect, leading to less dry mouth and constipation, and it’s often started at 25mg at night for seniors.
What are the main reasons to choose Venlafaxine over Elavil?
Venlafaxine offers stronger norepinephrine boost, which can help both mood and pain. It also avoids the cardiac QT prolongation seen with TCAs, though it may raise blood pressure at higher doses.
Do any of the alternatives help with sleep?
Elavil’s sedating effect can aid sleep, but it often comes with daytime grogginess. Among alternatives, low‑dose Duloxetine may improve sleep quality in chronic pain patients, while most SSRIs are neutral to mildly activating.
How does cost compare for NHS patients?
All listed alternatives are listed on the NHS drug tariff. When prescribed, the patient pays the standard prescription charge (£9.35 in England as of 2025) regardless of the brand, so cost differences mainly affect private purchases.





Whoa-have you ever considered that the pharma giants are secretly engineering Elavil to keep us glued to their profit pipelines?!? Every time you read about "alternatives" it's just a marketing smokescreen, a glittering distraction from the real agenda!!! They sprinkle a little serotonin here, a dash of norepinephrine there, and call it "therapy" while they siphon off your wages and your sanity!!!
While the exhaustive table provides a commendable overview, one must ponder the philosophical underpinnings of medication substitution-does altering chemical pathways truly resolve the existential malaise? 🤔 Nevertheless, the data is meticulously presented, and the inclusion of emojis adds a modern touch. 😊
Hey folks! 😊 I’m happy to dive a bit deeper into the nuances of switching from Elavil to its alternatives. First, remember that any taper should be gradual; dropping 25 mg per week is a commonly accepted schedule. 📉 Second, the choice of replacement often hinges on your primary therapeutic goal-whether it's mood stabilization, pain control, or both. 🌟 For patients plagued by daytime sedation, an SSRI like Sertraline or Fluoxetine usually offers a lighter side‑effect burden. 🙌 If chronic neuropathic pain is the dominant complaint, Duloxetine or Venlafaxine can provide comparable analgesia with a more favorable cardiac profile than TCAs. 🦶 Moreover, older adults frequently benefit from Nortriptyline because it retains efficacy while reducing anticholinergic load. 🚀 Keep in mind drug‑drug interactions: avoid combining serotonergic agents with MAO‑inhibitors or certain analgesics without careful monitoring. 💊 Finally, monitor blood pressure when on Venlafaxine, especially above 150 mg, as hypertensive spikes have been reported. 📈 In summary, weigh your symptom priorities, side‑effect tolerances, and any comorbid conditions before deciding. Feel free to reach out if you need a personalized taper plan! 🌈
i read the table and honestly idk why anyone would ditch elavil when u can just take a lil less dose?? it works fine for me tbh. plus all these other drugs r just a fad.
Hey there! I totally get how confusing it can be to navigate all these options. If you’re leaning toward something with less drowsiness, Sertraline is a solid pick and many find it easier on the stomach. On the other hand, if pain relief is your main goal, Duloxetine has strong evidence for neuropathic issues. Either way, a gentle taper off Elavil while starting low on the new med is the safest route. Feel free to ask if you need more specifics!
The author of this post seems to have missed several crucial grammatical nuances. For instance, "cardiac QT prolongation" should be capitalized as "QT”. Moreover, the repeated use of "and" at the start of clauses is unnecessary. While I am not inclined to overtly criticize, it is evident that a thorough editorial review is required, especially given the importance of medical information.
Nice summary. If you’re looking for less anticholinergic effect, Nortriptyline stands out. For anxiety comorbidity, Sertraline works well. Duloxetine covers both mood and pain with manageable side‑effects.
It’s intriguing how the article paints these alternatives as unequivocal upgrades, yet overlooks the fact that many patients experience a trade‑off between efficacy and tolerability. While Elavil’s analgesic properties are well‑documented, the newer agents, especially the newer SNRI formulations, sometimes fall short in severe neuropathic pain scenarios. Moreover, the cost considerations for private patients cannot be dismissed; generic versions do aid, but brand‑name pricing still influences prescribing habits. One could argue that the decision matrix is far more nuanced than a simple “switch if you have side‑effects” heuristic.
Honestly, the whole “look for alternatives” narrative is a bit overblown. Everyone’s quick to demonize Elavil for its side‑effects, yet they forget how robust its analgesic action is. If you’re not willing to endure a bit of dry mouth for real pain relief, you might as well stick with it. The newer SSRIs and SNRIs? Sure, they’re “cleaner,” but they often lack the gritty potency you need for chronic pain. Bottom line: don’t be swayed by hype; weigh your personal pain threshold against the mild inconveniences.
Great helpfull info, thx!
From a pharmacodynamic perspective, the transition from a tricyclic such as amitriptyline to a selective serotonin reuptake inhibitor necessitates a meticulous titration protocol to mitigate serotonergic excess. The cited literature substantiates a stepwise decrement of 25 mg per week concomitant with initiation of the SSRI at a sub‑therapeutic dose. Moreover, the risk stratification matrix embedded within the table underscores the imperative of cardiac monitoring due to QT interval elongation inherent to TCAs.
I think it’s good to see simple options. If you want less side effects, try sertraline or duloxetine. Talk to your doctor and see what fits your life.