Medication Photosensitivity Risk Checker
Check Your Medication Risk
Enter medications you're taking to assess photosensitivity risk. This tool helps identify which drugs increase sun sensitivity and shows recommended protection strategies.
Your Photosensitivity Risk Assessment
Medication Information
More than 1,000 common medications can make your skin dangerously sensitive to the sun-even on cloudy days or through windows. If you’re taking antibiotics, blood pressure pills, or even over-the-counter pain relievers, you might be at risk for a photosensitivity reaction without even knowing it. This isn’t just a bad sunburn. It’s a chemical reaction inside your skin triggered by sunlight and your medication, and it can lead to blisters, long-lasting dark spots, or even increase your risk of skin cancer.
What Exactly Is Medication-Induced Photosensitivity?
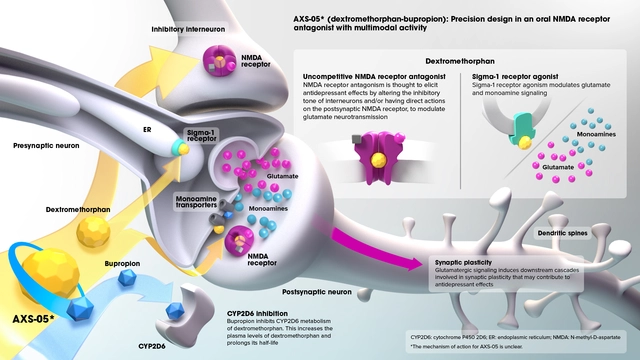
Photosensitivity from medications happens when certain drugs react with ultraviolet (UV) light, especially UVA rays (320-400 nm). These rays penetrate deeper than UVB and aren’t blocked by regular glass or most sunscreens. Once the drug absorbs the light, it creates harmful molecules that damage skin cells. There are two main types: phototoxicity and photoallergy.Phototoxicity makes up 95% of cases. It’s like your skin gets burned from the inside out. You’ll see redness, swelling, and pain within minutes to a couple of hours after sun exposure. It looks like a bad sunburn, but worse-and it only shows up where the sun hit. Think of it like a chemical burn from the drug + sunlight combo.
Photoallergy is rarer but trickier. It’s an immune response. Your body turns the drug into a foreign substance when exposed to UV light, then attacks it. This causes an itchy, eczema-like rash that can spread beyond sun-exposed areas. It shows up 1-3 days after exposure, so people often don’t connect it to their meds. You might think you’re allergic to the sun, but it’s your pill.
Which Medications Cause the Most Problems?
Some drugs are far more likely to cause photosensitivity than others. The biggest offenders include:- Tetracyclines (like doxycycline): Used for acne, Lyme disease, and infections. Up to 20% of users get phototoxic reactions-even through light clothing.
- NSAIDs (like ketoprofen, ibuprofen): Common painkillers. Ketoprofen patches are especially risky because they sit directly on the skin.
- Fluoroquinolones (like ciprofloxacin): Antibiotics for urinary and respiratory infections.
- Amiodarone: A heart medication. Up to 75% of long-term users develop blue-gray skin discoloration that lasts for years-even after stopping the drug.
- Sulfonamides and phenothiazines: Used for infections and mental health conditions. These are common causes of photoallergy.
- Diuretics (like hydrochlorothiazide): High blood pressure meds. Often overlooked, but they’re a top cause of sun-related rashes in older adults.
Antibiotics make up 40% of all photosensitivity cases. Cardiovascular drugs like amiodarone and hydrochlorothiazide account for another 25%. Women are more likely to experience photoallergic reactions-partly because they use more topical medications and cosmetics that also contain photosensitizing ingredients like oxybenzone.
Why Most Sunscreens Don’t Work
Standard SPF 30 sunscreens focus on UVB protection-the rays that cause sunburn. But phototoxic reactions are driven by UVA, which SPF ratings barely measure. Many sunscreens labeled SPF 50+ still don’t block enough UVA. In fact, only about 35% of SPF 50+ sunscreens meet the critical wavelength standard for true UVA protection, according to dermatology experts.What actually works? Look for sunscreens with:
- Zinc oxide at least 15% concentration
- Titanium dioxide as a secondary blocker
- “Broad Spectrum” on the label (but don’t rely on that alone)
Apply 1 ounce (a shot glass full) to cover your whole body. Most people use only 25-50% of the recommended amount, which cuts protection in half. Reapply every 2 hours-even if you’re not sweating or swimming. And yes, you still need to reapply indoors if you’re near windows or driving.

Clothing Is Your Best Defense
Regular cotton T-shirts offer only 3-20% UV protection. A white cotton shirt worn wet? That drops to 5%. That’s why dermatologists now say: if you’re on a photosensitizing drug, your clothes are your first line of defense.Look for clothing with UPF 50+ rating. This means it blocks 98% of UV radiation. Brands like Coolibar, Solbari, and Columbia’s Outdry line have been independently tested and proven effective. One patient on MyHealthTeams reported a 90% drop in reactions after switching to UPF 50+ long-sleeve shirts, wide-brimmed hats, and UV-blocking sunglasses.
Don’t assume dark colors are better-some dyes can actually make fabrics more transparent to UV. UPF-rated fabrics are engineered to reflect or absorb UV rays regardless of color. And yes, you can wear them in summer. Many are lightweight, moisture-wicking, and designed for heat.
What No One Tells You About UV Index
You don’t need to be at the beach to get burned. UV levels above 3 are enough to trigger a reaction in sensitive people. That’s common on spring and fall days-even when it’s cloudy. A UV index of 3 is equivalent to being in direct sun for 30 minutes without protection.Use apps like UVLens or the EPA’s SunWise app to check real-time UV levels. Cleveland Clinic studies show patients who avoided outdoor activity when the UV index was above 3 had 40% fewer reactions. Plan walks for early morning or late evening. Stay indoors between 10 a.m. and 4 p.m. if you’re on high-risk meds.
Why Doctors Often Miss This
Up to 70% of photosensitivity cases are misdiagnosed as “polymorphic light eruption” or just “sun allergy.” Most primary care providers don’t screen for it. A 2022 survey found 68% of patients received no sun safety advice when they were prescribed photosensitizing drugs.Even when patients report rashes after sun exposure, doctors rarely ask about medication use. But it’s simple: if you got a rash after sun exposure and you’re on a new drug, assume it’s related until proven otherwise. Bring your full med list-prescription, OTC, and supplements-to every appointment. Some supplements like St. John’s Wort and beta-carotene can also trigger reactions.
What to Do If You React
If you notice redness, burning, or blistering after sun exposure:- Get out of the sun immediately.
- Cool the area with damp cloths or a lukewarm bath.
- Use aloe vera or hydrocortisone cream (1%) for itching and inflammation.
- Take an antihistamine if it’s itchy or swollen.
- Call your doctor or dermatologist. Don’t wait for it to heal on its own.
Never ignore blisters or dark patches that don’t fade. Amiodarone can cause permanent gray-blue skin discoloration. Some reactions leave scars or increase melanoma risk. Early intervention matters.
New Tools and Hope on the Horizon
In 2023, the FDA approved Lumitrex (photoprotectin), the first medication designed specifically to reduce UV-induced skin damage. In trials, it cut reactive oxygen species by 70%. It’s not yet widely available, but it signals a shift toward treating photosensitivity as a medical condition-not just a side effect.Genetic testing is also entering the picture. Companies like 23andMe now offer a photosensitivity risk panel that checks for gene variants linked to higher reaction risk. If you’ve had unexplained sun reactions before, this test could help you avoid future problems.
And the market is catching up. The global market for sun-protective clothing hit $3.2 billion in 2022 and is growing 18% a year. The FDA now requires photosensitivity warnings on over 200 high-risk medications. Kaiser Permanente’s electronic health system now flags patients on high-risk drugs with automatic sun safety alerts-cutting reactions by 28% in the first year.
Bottom Line: Protect Yourself Like Your Skin Depends On It
Because it does. Photosensitivity isn’t a minor inconvenience. It’s a hidden risk built into everyday prescriptions. If you’re on any of the medications listed here, don’t wait for a reaction. Take action now:- Ask your doctor: “Is this drug linked to sun sensitivity?”
- Use zinc oxide sunscreen (SPF 50+, 15%+ zinc oxide) daily-even indoors.
- Wear UPF 50+ clothing, wide-brimmed hats, and UV-blocking sunglasses.
- Check the UV index every day. Avoid sun when it’s 3 or higher.
- Track your reactions. Note what meds you’re on and when sun exposure happened.
The Skin Cancer Foundation estimates better management of photosensitivity could prevent 2,000-3,000 non-melanoma skin cancers in the U.S. each year by 2025. You don’t need to give up the sun. You just need to protect yourself the right way.
Can you get photosensitivity from over-the-counter drugs?
Yes. Common OTC pain relievers like ibuprofen and naproxen can cause phototoxic reactions, especially in higher doses or with prolonged use. Topical NSAIDs like ketoprofen gel or patches are even riskier because they’re applied directly to the skin. Even some herbal supplements like St. John’s Wort or beta-carotene can trigger reactions. Always check the label or ask your pharmacist.
Do I need to stop my medication if I get a sun reaction?
Not necessarily. Many people manage photosensitivity by changing sun habits without stopping their meds. For example, switching from doxycycline to an alternative antibiotic might help, but for chronic conditions like heart disease or acne, stopping the drug could be riskier than the reaction. Talk to your doctor about alternatives, but don’t quit cold turkey. Use stronger sun protection first.
How long does photosensitivity last after stopping the drug?
It depends on the drug. For most, the risk fades within days or weeks after stopping. But amiodarone can cause reactions for up to 20 years. Tetracyclines usually clear within a few weeks. Hydrochlorothiazide may linger for months. If you’re unsure, keep protecting your skin for at least 3 months after stopping the medication. Some discoloration or sensitivity may be permanent.
Can sunscreen cause photosensitivity?
Yes. Ironically, some chemical sunscreens contain ingredients like oxybenzone, octocrylene, and avobenzone that can themselves trigger photoallergic reactions. If you’re getting rashes even when you use sunscreen, switch to mineral formulas with zinc oxide or titanium dioxide. Avoid fragranced or “anti-aging” sunscreens-they often contain more sensitizers.
Is photosensitivity more common in older adults?
Yes. Since 1999, prescription medication use among adults over 65 has tripled. Many older adults take multiple photosensitizing drugs-like blood pressure meds, antibiotics, and painkillers-simultaneously. Their skin is also thinner and less able to repair UV damage. This makes them far more vulnerable. Yet, only 35% of primary care providers screen for it. If you’re over 65 and on multiple meds, assume you’re at risk and take extra precautions.







This post just saved my life. I thought I was allergic to the sun for years-turns out it was my damn ibuprofen. I started wearing UPF shirts and now I can actually go outside without looking like a boiled lobster. Thank you so much for laying this out like a superhero guide for skin survival.
omg i had no idea ketoprofen patches were this dangerous… i’ve been using them for my back pain for months. just threw them out. also switched to zinc oxide sunscreen. my skin hasnt broken out in weeks. ps: if u r on amiodarone… u r basically a vampire now. no sun. ever. 😭
Thank you for sharing this so clearly. I’m a nurse and I see so many elderly patients with unexplained rashes-no one ever connects it to their meds. I’m printing this out for our clinic. Also, the part about UPF clothing? Game changer. My mom’s been wearing those Coolibar shirts all summer and she finally stopped complaining about her arms burning. 🙏
What’s fascinating here is the systemic failure in medical education. Photosensitivity isn’t a side effect-it’s a pharmacokinetic interaction with environmental photobiology. The fact that 68% of patients get zero counseling speaks to a structural blind spot in primary care. We treat drugs as isolated entities, not as components in a dynamic system with sunlight, skin physiology, and epidermal metabolism. The FDA’s new labeling requirements are a start, but we need mandatory continuing ed for prescribers. And yes, 23andMe’s panel? Validated. If you’ve ever had a weird sun rash, get tested.
India has 1.4 billion people on blood pressure meds. Most don’t even own sunscreen. We need public health campaigns here-not just blog posts. My uncle got permanent discoloration from hydrochlorothiazide and no doctor ever warned him. This info needs translation, not just posting.
just switched to zinc oxide sunscreen and i feel like a new person 🌞✨ also bought a UPF hat and now i can walk my dog without panicking. also-st john’s wort is a sneaky one. i had no idea herbal = dangerous. thank you for this. i’m sharing with my mom who’s on 7 meds and thinks she’s ‘just sensitive to sunshine’
THIS IS A BIG PHARMA COVERUP. They know UVA penetrates glass. They know 95% of reactions are phototoxic. They don’t warn you because if you stop taking your meds, you stop buying them. And don’t get me started on how they market SPF 50+ while using chemical filters that cause MORE reactions. The FDA? Bought and paid for. Lumitrex? A distraction. Real solution? Stop taking pills. Go natural. Eat turmeric. Drink lemon water. They don’t want you to know that.
Highly informative, but the tone is alarmist. Photosensitivity is a manageable clinical consideration-not a doomsday scenario. The 2,000–3,000 skin cancer prevention claim is speculative. Most phototoxic reactions are self-limiting. The emphasis on UPF clothing is reasonable, but the framing implies universal peril. This reads like a marketing brochure for sun-protective apparel brands. Still, the pharmacological data is solid.
I’m not saying it’s the government but why do you think all these sunscreens have oxybenzone? They want you to keep buying more. Also I’ve been wearing a baseball cap and calling it a day since 2015 and I’m fine. Maybe you’re just weak?