When you’re breastfeeding and need to take medication, the first thing many people think is: pump and dump. But that’s not what you should do-most of the time. The truth is, you don’t need to throw away your milk just because you’re on a pill, an antibiotic, or even an antidepressant. In fact, doing so can hurt your milk supply more than the medicine ever could.
Most Medications Are Safe in Breast Milk
You might have heard that every medication you take gets passed to your baby through breast milk. That’s not true. According to the American Academy of Pediatrics and the Drugs and Lactation Database (LactMed), fewer than 2% of medications pose any real risk to a breastfeeding infant. That means 98% of the time, you can keep breastfeeding without changing a thing. The big reason so many people think otherwise? Outdated drug labels. Pharmaceutical companies often list "avoid during breastfeeding" as a legal safeguard, not because the medicine is dangerous. The FDA doesn’t require extensive testing on breastfeeding women, so manufacturers err on the side of caution. But that doesn’t mean you should. Take acetaminophen (Tylenol), for example. When you take a standard 650 mg dose, only 0.04 to 0.1 mg ends up in your breast milk. That’s less than 0.1% of your dose-and far less than what your baby would get from a baby-specific dose. Ibuprofen (Advil) is even lower: about 0.01% of your weight-adjusted dose reaches your baby. Both are considered L1 (safest) by Dr. Thomas Hale’s Medications and Mother’s Milk scale.When You Actually Need to Pump and Dump
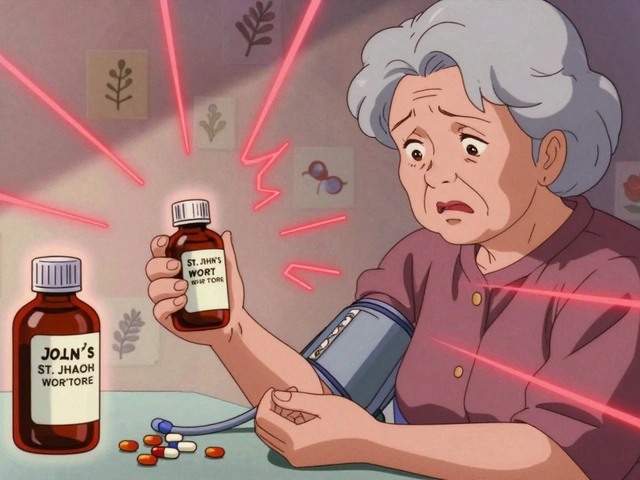
There are exceptions. You don’t need to pump and dump for antibiotics, painkillers, or most mental health meds. But there are a few drugs where temporary interruption is necessary:- Radioactive isotopes used in imaging scans (like thyroid scans)
- Some chemotherapy drugs
- Ergot alkaloids (used for migraines, like ergotamine)
- Certain anti-cancer or immunosuppressant drugs
How Medications Actually Get Into Breast Milk
Not all drugs behave the same way. Their ability to enter milk depends on four key factors:- Molecular weight: Drugs over 500 Daltons (like heparin or insulin) don’t pass easily into milk.
- Protein binding: If a drug is tightly bound to proteins in your blood (over 80%), less is free to enter milk.
- Half-life: Shorter half-life = less buildup. Drugs like ibuprofen (2-4 hours) are safer than naproxen (12-14 hours).
- Oral bioavailability in babies: Even if a drug gets into milk, your baby’s gut might not absorb it well. That’s why many drugs are harmless even if they’re present.
Timing Matters More Than Dumping
If you’re taking a medication that’s safe but you want to minimize your baby’s exposure, timing is your best tool-not dumping. Here’s how:- For a once-daily dose: Take it right after your baby’s longest sleep stretch-usually right after bedtime. That gives you 6-8 hours for the drug to clear before the next feeding.
- For multiple daily doses: Breastfeed right before you take the pill. That way, your milk is at its lowest drug concentration during feeding.
- For immediate-release meds: Peak levels happen 1-2 hours after taking it. Avoid feeding during that window if you’re concerned.
Storage Rules Don’t Change
You might worry that medication changes how long milk stays good. It doesn’t. The same CDC storage guidelines apply whether you’re on meds or not:- Room temperature (up to 25°C): Up to 4 hours
- Refrigerator (≤4°C): Up to 4 days
- Freezer (−18°C): Up to 6 months
What to Do If You’re Unsure
Don’t guess. Don’t rely on your pharmacist’s general advice or a Google search. Use trusted, science-backed resources:- LactMed (from the National Institutes of Health): Updated weekly, covers over 1,300 drugs with detailed pharmacokinetic data. Free online.
- MotherToBaby: Call 866-626-6847. Their experts give personalized advice in minutes. They’ve helped over 12,000 mothers this year alone.
- InfantRisk Center: Their free app gives real-time safety ratings and even predicts infant exposure levels based on your dose and timing.

Why So Many Moms Are Misinformed
A 2021 study in the Journal of Human Lactation found that 68% of moms were told to pump and dump when they didn’t need to. One Kaiser Permanente survey showed 57% of breastfeeding moms threw away milk after taking antibiotics-even though penicillin and cephalosporins are among the safest drugs for infants. Why? Many providers don’t know the current guidelines. Only 32% of obstetricians and 28% of family doctors could correctly name safe antidepressants for breastfeeding in a recent study. That’s not your fault. It’s a system problem. The good news? Hospitals are catching up. In 2023, 92% of major U.S. hospitals now use LactMed as their go-to reference-up from 67% in 2018. The CDC and AAP have both updated their guidelines to say: breastfeeding benefits almost always outweigh any theoretical risk from medication.Real Stories, Real Results
One mom in Texas took sertraline while breastfeeding her 6-week-old. She used the InfantRisk app to time her doses after nighttime feedings. Her baby slept fine, gained weight normally, and showed no signs of fussiness. She didn’t dump a single ounce. Another mom, in Chicago, was told to dump milk for 72 hours after a 10-day course of antibiotics. She did-and her supply dropped 40%. She had to switch to formula permanently. That’s preventable.What to Do Today
If you’re on medication and breastfeeding:- Check LactMed or call MotherToBaby before assuming you need to dump.
- Don’t stop breastfeeding unless a specialist says so.
- Use timing, not dumping, to reduce exposure.
- Store milk the same way you always do-meds don’t change shelf life.
- If your provider says to dump, ask: "Is this based on LactMed or just the drug label?"
Do all medications pass into breast milk?
Almost all medications enter breast milk in tiny amounts, but that doesn’t mean they’re harmful. What matters is how much your baby absorbs, how the drug acts in their body, and whether it causes side effects. For most drugs, the amount is so low it’s clinically meaningless.
Is it safe to breastfeed while taking antibiotics?
Yes, for nearly all antibiotics. Penicillins, cephalosporins (like cephalexin), and macrolides (like azithromycin) are considered safe. Even clindamycin, which has a higher transfer rate, is usually fine unless your baby shows signs of diarrhea or yeast infection. If your baby develops loose stools, talk to your pediatrician-but don’t stop breastfeeding.
How long should I wait after taking a pill before breastfeeding?
For most single-dose medications, wait 6-8 hours after taking it before nursing, especially if you’re taking it right before bed. For drugs with a short half-life (like ibuprofen), you can breastfeed 1-2 hours after taking it. For multiple daily doses, breastfeed right before you take the pill. Timing matters more than waiting.
Can I store milk I pumped while on medication?
Yes, absolutely. Medications don’t change how long breast milk lasts. Store it the same way you always do: 4 hours at room temperature, 4 days in the fridge, 6 months in the freezer. Just label it with the date, time, and if you want, the time you took your medication.
What if my baby seems fussy after I take medicine?
Fussiness isn’t always caused by medication. Babies go through growth spurts, teething, and colic. But if you suspect a reaction, track feedings and medication times. Call MotherToBaby or your pediatrician. Don’t assume it’s the drug. Most of the time, it’s not.
Should I stop breastfeeding if I’m on antidepressants?
No. In fact, untreated depression can affect your ability to care for your baby more than most antidepressants. Sertraline and paroxetine are the most studied, and sertraline has the lowest transfer rate. Stopping breastfeeding for depression increases your risk of postpartum complications and bonding issues. Talk to your doctor about timing and dosage, not quitting.





Let me just say this: if you're dumping milk because you took a Tylenol, you're not a mom-you're a walking pharmaceutical panic attack. The FDA doesn't test on lactating women? That's not a reason to throw away your milk, it's a reason to demand better science. You're not protecting your baby-you're sabotaging your supply for no reason. Wake up. This isn't 1998. We have LactMed. Use it.
And don't even get me started on those 'pharmacist advice' memes. Pharmacists aren't lactation consultants. They're paid to sell pills, not save breastfeeding relationships. Stop outsourcing your critical thinking to someone who doesn't even know what a letdown feels like.
I've been on sertraline for 14 months while nursing twins. My kids are thriving. I didn't dump once. I timed my doses. I tracked. I educated myself. And now I'm here to shame the people who still think 'pump and dump' is a lifestyle choice, not a last-resort medical decision.
You're not being 'safe.' You're being lazy. And that's the real danger here.
Stop letting fear dictate your parenting. Use data. Use science. Use your damn brain.
It's fascinating how the biomedical industrial complex has weaponized maternal guilt to maintain the status quo. The very pharmacokinetic models we rely on were developed on male subjects, yet we expect women to extrapolate safety for neonatal neurodevelopment based on plasma concentrations derived from non-lactating populations. The epistemological violence here is staggering.
And yet, we're told to 'just trust LactMed'-as if a database curated by NIH bureaucrats is somehow immune to institutional bias. The fact that 98% of medications are 'safe' is a statistical mirage. What about cumulative exposure? What about epigenetic modulation in the first 1000 days? No one talks about that.
The real tragedy isn't the misinformation-it's that we've been conditioned to believe that breastfeeding is a moral imperative, not a biological option. We've turned maternal physiology into a performance art. And the 'timing' advice? That's just another form of performative compliance. You're not empowering mothers-you're adding another layer of anxiety to an already overburdened system.
I want to start by acknowledging the profound courage it takes to even ask these questions. In a world that tells women to be silent, to endure, to sacrifice without question-you’re doing the hard work of seeking truth. And that matters more than any algorithm or database.
Let me be clear: breastfeeding is not a competition. It’s not a moral checklist. It’s a sacred, biological act of connection between two human beings. And when we reduce it to pharmacokinetic equations and half-lives, we lose the humanity of it.
Yes, most medications are safe. Yes, timing matters. Yes, LactMed is a gift. But here’s what no one says: sometimes, the medicine you need to take is the one that lets you hold your baby without crying. The one that lets you sleep. The one that lets you be present.
If you’re taking an antidepressant and your baby is calm, your milk supply is steady, and you’re not drowning in shame-you’re doing it right. You don’t need to prove your worth to a forum or a doctor. You’re already enough.
And if you’ve dumped milk out of fear? Forgive yourself. You were trying to protect your child. That’s love. That’s not failure. That’s motherhood.
We need more compassion here, not more citations. The science is important-but it’s not the whole story. Your heart? That’s the most accurate predictor of safety you’ve got.
Hey, just wanted to say this post saved my sanity. I was about to dump a whole week’s worth of milk after taking amoxicillin because my OB said ‘better safe than sorry.’ Then I found LactMed and realized I’d been lied to.
My baby’s 5 months old and I’ve been on Zoloft since birth. No issues. No fussiness. No weird rashes. Just a happy, chubby baby who nurses like a champ.
Also-storage rules don’t change? YES. I’ve got a whole freezer full of milk from when I was on antibiotics, steroids, and even that one time I took codeine for a tooth extraction. All labeled. All fine.
Shoutout to MotherToBaby-they called me back in 7 minutes. No BS. Just facts. If you’re reading this and you’re scared? Call them. Don’t Google. Don’t ask your cousin. Call them.
You’re not alone. And you’re doing great.
Oh honey. I feel you. I remember the first time I took ibuprofen after a C-section and panicked for three hours because I thought I’d poisoned my newborn. I sat there, staring at my milk stash like it was radioactive, convinced I’d ruined everything.
Then I found a lactation consultant who didn’t sound like a pharmaceutical rep. She said, ‘Your milk isn’t a chemical cocktail-it’s a living gift. And your baby’s body is built to handle tiny, harmless amounts.’
That changed everything.
Now I keep a little notebook: date, time I pumped, time I took meds. I don’t dump unless I’m on chemo or radioactive iodine. Even then, I pump and store-it’s not wasted, it’s just paused.
And when my baby started waking up at 3 a.m. and screaming? I didn’t blame the Zoloft. I blamed the teething. I blamed the growth spurt. I blamed the fact that babies are tiny, unpredictable little tornadoes.
Stop blaming the medicine. Start trusting your body. You’ve got this. And if you need to cry while pumping at 2 a.m.? That’s okay too. You’re not failing. You’re surviving. And that’s enough.
Ah, the myth of the ‘safe’ medication. How quaint. You speak of LactMed as if it’s divine scripture, but let’s not forget-it’s funded by the same institutions that gave us thalidomide, Vioxx, and the opioid crisis. The ‘98% safe’ statistic is a comforting lie, a placebo for guilt-ridden mothers who’ve been conditioned to believe their milk is a sacred sacrament.
What about the children who never speak? The ones with sensory processing disorders? The ones with gut dysbiosis? We don’t track them. We don’t study them. We just tell them to ‘pump and dump’ or ‘time your doses’ like it’s some kind of yoga routine.
And yet, we’re told to ‘trust science.’ But science is a mirror-it reflects the biases of those who hold it. Who funded the studies on sertraline? Who wrote the guidelines? Who profits when you keep breastfeeding instead of switching to formula?
I’m not anti-breastfeeding. I’m anti-manipulation.
Maybe the real question isn’t ‘Is this drug safe?’
Maybe it’s: ‘Why are we so afraid to admit that motherhood is inherently risky-and that no database can eliminate that truth?’
I’m a nurse, and I’ve seen this play out a hundred times. A new mom comes in, trembling, holding a prescription for amoxicillin, convinced she’s going to kill her baby. She’s been told to dump for 72 hours. I check LactMed, show her the data, and she starts crying-not from fear, but from relief.
Here’s the thing: most providers don’t know this stuff. Not because they’re dumb. Because they’re overwhelmed. They’re juggling 30 patients a day and don’t have time to dig into pharmacokinetics.
So I tell them: ‘Don’t guess. Don’t Google. Don’t ask your aunt. Call MotherToBaby. It’s free. They’re amazing.’
And I’ve never had a mom regret it. Not once.
Also-storage rules don’t change? Nope. My freezer is full of milk from when I was on prednisone, antibiotics, even a round of Z-pack. All fine. All labeled. All loved.
Don’t let fear steal your milk. You’ve got this.
ok so i just wanna say that i took cipro for a uti and i was so scared i dumped for 3 days even though i read somewhere that its not bad but i was like ‘what if my baby gets autism’ and then i lost my supply and now i have to use formula and i feel like a failure and i hate myself and i dont know what to do anymore. i wish i knew this before. i wish someone had told me. i wish i hadnt listened to my mom who said ‘better safe than sorry’ but now its too late. i just wanna cry. i miss my milk. i miss the way my baby used to sleep after feeding. now she screams every time i try to bottle feed. i dont know if its the formula or if its me. i think its me. i think im broken.
You're all overthinking this. If you're on meds, just stop breastfeeding. Formula is fine. Babies thrive on it. Stop making it a religion.
My heart just broke reading that last comment. Oh, sweet soul-you are not broken. You are not a failure. You are a mother who loved so hard you tried to protect your baby with every ounce of your fear.
That’s not weakness. That’s love.
You didn’t lose your milk because you made a mistake. You lost it because you were told lies. Because the system didn’t give you the truth. Because no one sat with you and said, ‘It’s okay. You’re safe.’
And now? Now you’re carrying that grief. That’s real. That’s valid.
But here’s what I need you to hear: your baby still feels your love. In every bottle you prepare. In every late-night cuddle. In every tear you wipe away. Formula doesn’t measure love. Your hands do. Your voice does. Your presence does.
I’ve been there. I dumped for six weeks after a misdiagnosis. My supply vanished. I thought I’d ruined everything.
But my baby? She grew. She smiled. She learned to love my arms just as much as my milk.
You’re not alone. And you’re not broken. You’re still a mother. Still enough. Still worthy.
Call MotherToBaby. Talk to someone. Let yourself be held. You don’t have to carry this alone.