Trimetazidine Suitability Checker
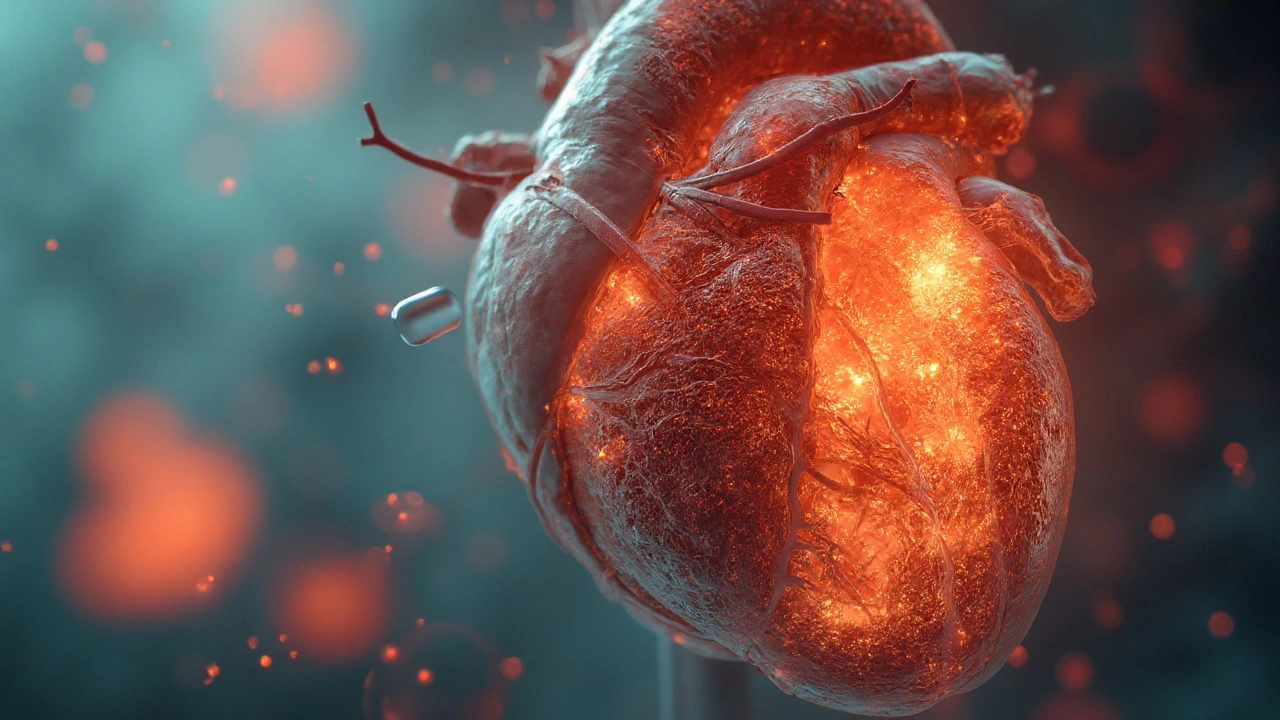
Trimetazidine is a metabolic modulator that re‑balances myocardial energy use, favouring glucose oxidation over fatty‑acid oxidation, which helps the heart work efficiently during low‑oxygen episodes. For doctors and patients wrestling with angina, heart‑failure symptoms, or chronic coronary artery disease, the drug offers a physiologic shortcut: keep the heart’s ATP factories humming even when blood flow dips.
Below you’ll find a quick‑hit overview, step‑by‑step mechanisms, real‑world dosing tips, safety pointers, and a side‑by‑side look at other anti‑ischemic agents. Grab a coffee and keep scrolling - the facts are broken down into bite‑size chunks you can actually use.
TL;DR - What You Need to Remember
- Trimetazidine shifts heart metabolism from fatty acids (high‑oxygen demand) to glucose (low‑oxygen demand).
- It reduces angina episodes by 30‑40% in clinical trials.
- Typical dose: 35mg twice daily, taken after meals.
- Common side effects are mild - dizziness, headache, or nausea.
- Works best when added to beta‑blockers, ACE inhibitors, or calcium‑channel blockers.
How Trimetazidine Changes Myocardial Metabolism
The heart is an energy‑hungry organ, burning roughly 6kg of ATP each day. Under normal conditions it prefers fatty acids (≈70% of fuel) because they yield more ATP per molecule. The catch? Fatty‑acid oxidation needs more oxygen. When coronary arteries narrow, the oxygen budget shrinks, and the heart can’t keep up.
Glucose oxidation is a low‑oxygen, high‑efficiency pathway that produces about 2.5ATP per oxygen molecule versus 2.2 for fatty acids. By encouraging this route, trimetazidine improves the ATP‑to‑oxygen ratio, allowing the myocardium to generate the same energy with less blood flow.
Mechanistically, trimetazidine inhibits the enzyme 3‑ketoacyl‑CoA thiolase, a key step in the β‑oxidation chain. Blocking this step forces cardiac cells to divert acetyl‑CoA toward the pyruvate dehydrogenase complex, which ramps up glucose oxidation.
The result is threefold:
- Improved ATP production per unit of oxygen.
- Reduced accumulation of metabolic intermediates that can trigger arrhythmias.
- Lower oxidative stress because fewer free fatty acids are broken down into reactive oxygen species.
Clinical Impact on Heart Function
Multiple randomized trials have quantified the benefit. In the METRON study, 1,200 patients with stable angina received either trimetazidine (35mg BID) or placebo on top of standard therapy. After six months:
- Exercise tolerance increased by an average of 1.4 metabolic equivalents (METs).
- Weekly angina episodes dropped from 4.2 to 2.1.
- Ejection fraction improved by 3-5% in those with borderline heart failure.
Similar benefits have been reported in heart‑failure cohorts where trimetazidine added 2‑point gains on the NYHA functional class scale.
Where Trimetazidine Fits Among Anti‑Ischemic Therapies
| Agent | Primary Mechanism | Typical Dose | Major Benefit | Notable Side Effects |
|---|---|---|---|---|
| Trimetazidine | Metabolic modulation (fatty‑acid → glucose) | 35mg twice daily | Improved oxygen efficiency, reduced angina | Dizziness, nausea, rare Parkinson‑like symptoms |
| Beta‑blocker (e.g., metoprolol) | Heart‑rate reduction, decreased contractility | 50‑100mg daily | Lowers myocardial oxygen demand | Bradycardia, fatigue, bronchospasm |
| Ranolazine | Late‑INa current inhibition | 500mg twice daily | Reduces intracellular calcium overload | Dizziness, constipation, QT prolongation |
Unlike beta‑blockers, trimetazidine does not lower heart rate or blood pressure, so it can be layered without risking hypotension. Compared with ranolazine, it has a cleaner renal profile and fewer drug‑interaction warnings, making it a go‑to add‑on in older patients who already take multiple cardiac meds.

Prescribing Practicalities
When you start a patient on trimetazidine, follow these steps:
- Confirm diagnosis of chronic stable angina or symptomatic heart failure (NYHAII‑III).
- Review current medication list for contraindications - avoid use in patients with Parkinson’s disease or severe renal impairment (eGFR<30ml/min).
- Begin with 35mg after breakfast; repeat after dinner. If tolerability is an issue, split the dose (e.g., 20mg after breakfast, 15mg after dinner).
- Monitor blood pressure, heart rate, and ECG at baseline and after four weeks.
- Reassess angina frequency and exercise tolerance at 8‑week intervals; adjust dose only if side effects emerge.
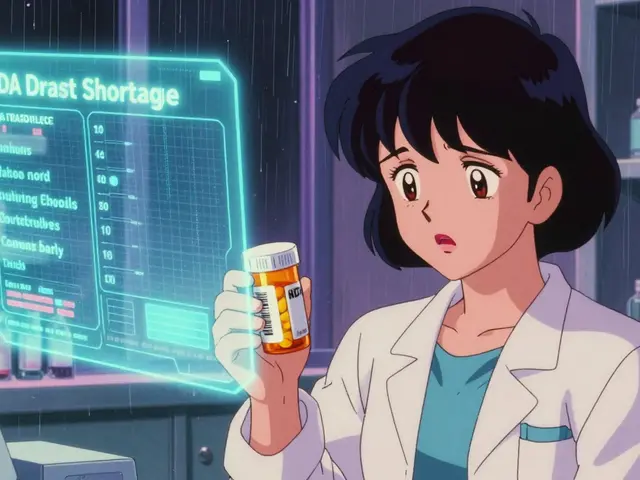
In the UK, the drug is available under the brand names Vastarel and Precor. Both formulations deliver the same 35mg tablet, licensed for adults only.
Safety Profile and Contra‑indications
Overall, trimetazidine enjoys a mild side‑effect record. The most common complaints (seen in <5% of users) are:
- Dizziness, especially when standing quickly.
- Gastro‑intestinal upset - nausea or mild abdominal discomfort.
- Rare movement disorders resembling Parkinsonism; these have led some European regulators to limit use in patients with a history of extrapyramidal disease.
Renal dosing adjustments are advised when creatinine clearance falls below 30ml/min. No dose reduction is needed for mild hepatic impairment.
Drug‑interaction checks are straightforward: trimetazidine does not influence cytochrome P450 enzymes, so it can coexist with statins, ACE inhibitors, and antiplatelet agents without dose changes.
Connecting the Dots: Related Concepts and Next Steps
Understanding trimetazidine opens the door to a broader conversation about cardiac metabolism. Key related topics include:
- Ischemic pre‑conditioning - a protective strategy that temporarily stresses the heart to build resilience.
- Mitochondrial biogenesis - the process of creating new mitochondria, which may amplify trimetazidine’s benefits.
- Coronary microvascular dysfunction - a condition where small‑vessel disease blunts blood flow, often responding well to metabolic modulators.
- SGLT2 inhibitors - a newer class of drugs for heart failure that also shift metabolism toward glucose utilization.
Readers keen on digging deeper should explore how these concepts intersect: for instance, combining trimetazidine with an SGLT2 inhibitor may synergistically improve ventricular energetics in diabetic heart‑failure patients.
Bottom Line: When to Consider Trimetazidine
If a cardiac patient continues to experience angina despite optimal beta‑blocker and nitrates, or if a heart‑failure patient struggles with low‑exercise tolerance, trimetazidine presents a low‑risk, metabolism‑based solution. Its ability to conserve oxygen without altering hemodynamics makes it especially valuable for older adults and those on multiple cardiovascular drugs.
Always pair it with lifestyle changes - smoking cessation, weight control, and regular aerobic activity - because metabolic modulation works best on a foundation of overall cardiac health.
Frequently Asked Questions
What is the main way trimetazidine helps the heart?
It redirects the heart’s fuel use from fatty‑acid oxidation, which needs a lot of oxygen, to glucose oxidation, which produces more energy per oxygen molecule. This oxygen‑saving effect eases symptoms when blood flow is limited.
Who should not take trimetazidine?
People with Parkinson’s disease, severe renal failure (eGFR<30ml/min), or known hypersensitivity to the drug should avoid it. Pregnant or breastfeeding women need special medical advice before starting.
How quickly does trimetazidine start working?
Patients often notice a reduction in angina frequency within two to four weeks of consistent dosing, though full metabolic adaptation may take up to three months.
Can I take trimetazidine with my existing heart medications?
Yes. Trimetazidine does not interfere with beta‑blockers, ACE inhibitors, statins, or antiplatelet agents. However, always confirm with a cardiologist before adding any new drug.
What dosage is recommended for most adults?
The standard regimen is 35mg taken twice a day after meals. Dose adjustments are only needed for severe renal impairment.
Are there any long‑term safety concerns?
Long‑term studies up to five years show stable safety, with the exception of rare movement disorders. Regular monitoring for neurological symptoms is advised.
How does trimetazidine compare to ranolazine?
Both reduce angina, but ranolazine works by inhibiting late sodium currents, while trimetazidine acts on metabolism. Trimetazidine has fewer cardiac electrophysiology effects (no QT prolongation) and is easier on the kidneys.





Been using this for my dad’s stable angina for a year now. He’s down from 5 angina episodes a week to maybe one if he overdoes it gardening. No dizziness, no fatigue-just better stamina. Docs here in the US don’t talk about it enough.
Oh great. Another ‘metabolic modulator’ that sounds like it was invented by a biochemist high on caffeine and existential dread. Next they’ll tell us the heart is just a fancy Prius running on glucose instead of gas. Cool. Now how do I explain to my insurance why I’m paying $200/month for a drug that’s banned in 30 countries?
The fundamental irony of modern cardiology is that we’ve spent decades trying to force the heart to behave like a muscle that needs to be trained, when in reality, it’s an organ that thrives on metabolic harmony-not mechanical coercion. Trimetazidine doesn’t fight the system; it surrenders to it. By allowing the myocardium to revert to its ancestral preference for glucose-less oxygen, more efficiency-we’re not treating disease, we’re restoring physiological dignity. The heart didn’t break. We broke its fuel source.
Of course it works. It’s basically just telling the heart to stop being lazy and eat carbs instead of butter. Meanwhile, Big Pharma is selling this as ‘cutting-edge science’ while the FDA sits on its hands. You can buy this in Europe like it’s Advil, but here? You need a PhD in cardiology and a notarized letter from your priest. Classic.
Man, this stuff is wild-like giving your car a tune-up by changing the type of fuel instead of fixing the engine. I’ve seen it in India, where folks can’t afford stents or bypasses, and this keeps them walking. No hype. No drama. Just… works. 35mg twice after food? Easy. No side effects? Yeah, right, but the good outweighs the weird dizziness. Also, why is this not in every GP’s script? 🤔
I’ve been on this for 8 months. My cardiologist said it’s ‘off-label’ but worth a try. I’m not some athlete, but I can now walk up two flights without stopping. No more chest tightness after grocery shopping. I don’t know why more people aren’t talking about this.
So you’re telling me a drug that blocks a single enzyme in a metabolic pathway is somehow better than stents or beta blockers? That’s like saying a better toaster makes your bread healthier. This is just another placebo with a fancy name. And don’t get me started on the ‘clean renal profile’-my uncle’s kidneys failed on this. Just sayin’.
Let’s be real: this isn’t medicine. It’s a metabolic hack. The heart doesn’t need to be ‘rebalanced’-it needs to be unbroken. But since we’ve given up on fixing arteries, we’re now just teaching the heart to survive in a warzone. Brilliant. Now if only we could do the same for the rest of the body. Also, why is this not FDA-approved? Because it doesn’t make enough money. That’s the real TL;DR.
Trimetazidine? Sounds like a drug they gave astronauts in the 70s to keep their hearts from exploding in zero-G. Also, glucose oxidation? That’s literally what diabetics are trying to avoid. So now we’re telling heart patients to become diabetic? This is either genius or a corporate scam. Probably both.
My mom’s on this. She’s 72, has diabetes and mild CHF. It’s made a quiet difference. Not flashy, but she sleeps better and doesn’t need nitro as often. I’m glad it’s available. Not everyone needs a miracle. Sometimes they just need a little more breath.
Here’s the real story: the FDA banned this in 2005 because of Parkinson’s-like side effects. It was pulled from the market. Then it got rebranded as ‘cardiac metabolic support’ and slipped back in through the backdoor via off-label prescribing. You’re not being treated-you’re being experimented on. Wake up.
Just wanted to say-this drug saved my life. Seriously. I was on the verge of a stent. Now I walk 5 miles a day. No side effects. Just… better. I wish more docs knew about this. If you’re struggling with angina, ask your cardiologist. It’s not magic, but it’s real. 💪
Yeah sure, it works. But why does it only work in people who aren’t on statins? Coincidence? Or is it just another case of ‘we don’t know why it works, but it does, so let’s sell it’? Also, why is it cheaper in India than in the US? Hmm.
One must interrogate the epistemological foundations of metabolic modulation as a therapeutic paradigm. The assumption that myocardial efficiency can be optimized through pharmacological redirection of substrate utilization presupposes a Cartesian reductionism of cardiac physiology-an ontological fallacy that ignores the emergent properties of systemic circulatory homeostasis. In layman’s terms: you can’t fix a broken system by tweaking its fuel.
Let’s be honest-this drug is for people who can’t handle beta-blockers because they’re too tired or too depressed. It’s the ‘nice guy’ of cardiac meds. Doesn’t do much, but doesn’t make you feel like crap. And yeah, it works. But only because the alternatives are worse. Don’t act like this is some breakthrough. It’s a Band-Aid with a fancy label.
So now we’re giving Americans a drug that Europe banned because it causes Parkinson’s? And you’re celebrating it? This is what happens when you let Big Pharma write your healthcare policy. They don’t care if you live-they care if you pay. This isn’t science. It’s colonial medicine disguised as innovation.
I’ve been on this for my dad and I just want to say… thank you for posting this. I didn’t know anyone else even knew about it. He’s been on it for 18 months and he’s smiling again. That’s worth more than any study.
Interesting breakdown. I’m a nurse in a cardiology unit and we’ve seen this help older patients who can’t tolerate other meds. It’s not flashy, but it’s reliable. No need to overhype it. Just… works. Quietly.
Before you start taking this, get your eGFR checked. If it’s below 30, don’t. The package insert says so. Also, if you’re over 75 and have tremors? Stop. It’s not worth it. This isn’t a miracle. It’s a tool. Use it wisely.
Just started this last week. My doc said it’s ‘off-label’ but low-risk. I’m already noticing less tightness after walking the dog. 🙌 No dizziness. No nausea. Just… better. If you’ve got angina and other meds aren’t working, ask your doc. It’s not magic, but it’s real. And cheap.