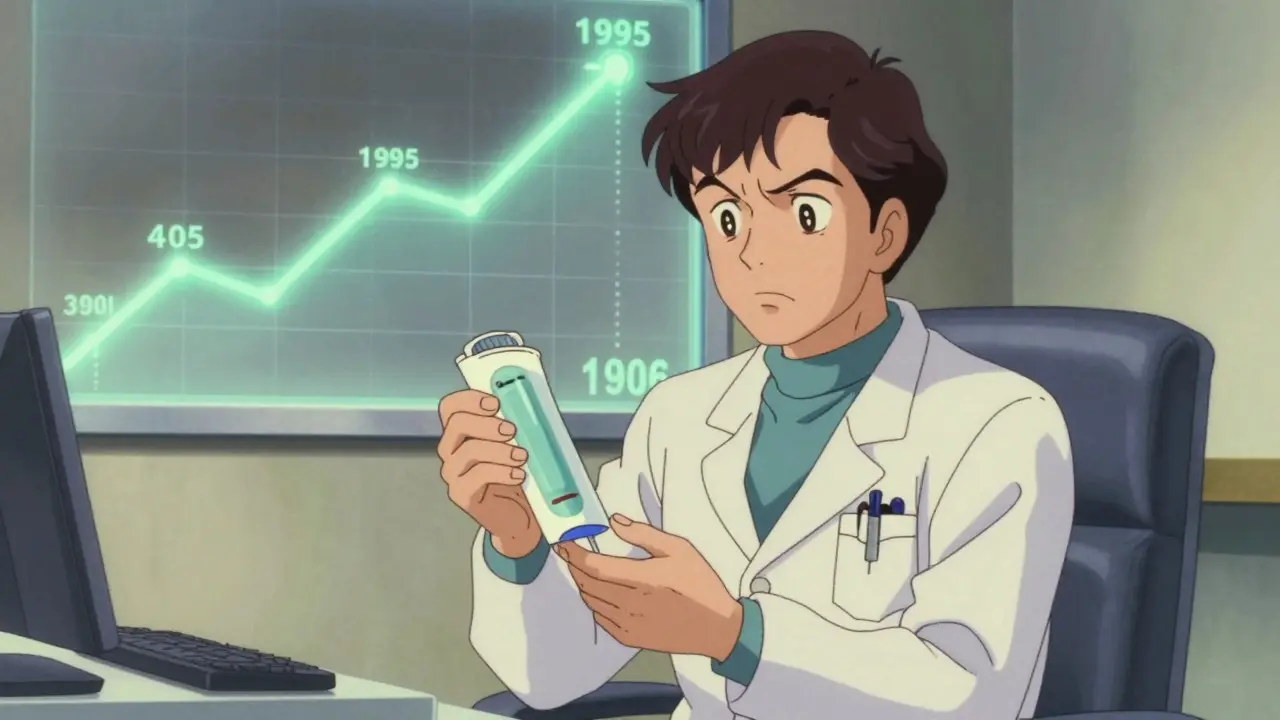
Colorectal cancer is no longer just a concern for people over 50. Since 2021, major health organizations in the U.S. have unanimously lowered the recommended starting age for screening to 45. This shift wasn’t made lightly-it’s a direct response to rising rates of colon and rectal cancer in younger adults. Between 1995 and 2019, incidence in people under 50 climbed by 2.2% each year. Today, one in five new cases happens in someone younger than 55. If you’re 45 or older, skipping screening isn’t an option. It’s the single most effective way to catch cancer early-or stop it before it starts.
Colonoscopy: The Gold Standard for Prevention
Colonoscopy remains the most powerful tool in colorectal cancer screening. Unlike stool tests that only detect blood or DNA markers, a colonoscopy lets a doctor see the entire colon in real time. If they find a polyp-a small growth that can turn cancerous-they can remove it right then and there. That’s prevention, not just detection.
Studies show colonoscopy reduces colorectal cancer incidence by 67% and cuts deaths by 65%. The procedure is recommended every 10 years for people at average risk, as long as the first one comes back clean. But it’s not perfect. Bowel prep is brutal-most people say it’s the worst part. You’ll need to drink a large volume of laxative solution the day before, which can cause nausea, cramps, and dehydration. Some newer prep kits use less fluid, but they’re not always as effective.
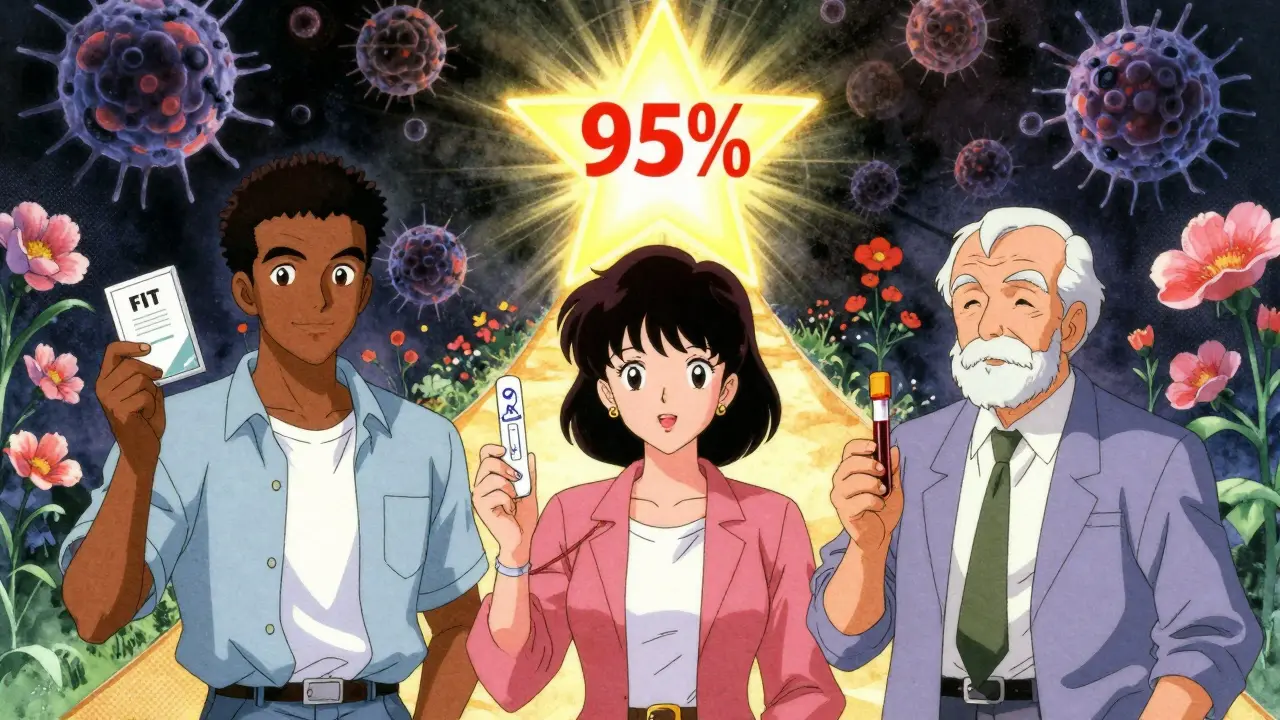
Complications are rare but real. Perforation (a tear in the colon) happens in about 1 out of every 1,000 to 1,500 procedures. Bleeding after polyp removal occurs in about 1% of cases. Still, the benefits far outweigh the risks. A 2023 case report in Gastroenterology & Hepatology followed a 47-year-old African American man who had stage I cancer found during his first colonoscopy at age 45. His 5-year survival rate was 95%. Had he waited until 50, the cancer might have been stage IV-with a survival rate of just 14%.
Alternatives to Colonoscopy: Stool Tests and Imaging
Not everyone wants a colonoscopy. That’s why there are other options, each with trade-offs.
Fecal Immunochemical Test (FIT) is the most common stool test. It looks for hidden blood in your stool-something that can signal cancer or large polyps. It’s simple: collect a sample at home, mail it in, and wait for results. Sensitivity for detecting cancer is 79-88%, but it only catches about half of large polyps. You need to do it every year. In safety-net clinics, adherence is 67% with FIT versus just 42% for colonoscopy. Hispanic patients are more likely to complete FIT than non-Hispanic White patients.
Multi-target stool DNA test (sDNA-FIT) is newer and more sensitive. It checks for both blood and abnormal DNA shed by cancer cells. It finds 92% of colorectal cancers-better than FIT’s 74%. But it has a downside: only 87% specificity means more false positives. That leads to unnecessary colonoscopies. It’s approved every three years, but it’s expensive and not always covered by insurance.
CT colonography (also called virtual colonoscopy) uses X-rays to create a 3D image of your colon. No sedation, no scope. But you still need bowel prep. And if they find anything, you still need a colonoscopy to remove it. Plus, you’re exposed to low-dose radiation-about the same as a mammogram. It’s good for people who can’t tolerate sedation, but it’s not ideal for routine screening.
Flexible sigmoidoscopy checks only the lower third of the colon. It’s faster, needs less prep, and has fewer complications. But it misses up to 40% of polyps and cancers in the upper colon. It’s recommended every five years and is rarely used alone anymore.
Who Needs to Start Earlier Than 45?
If you have a family history of colorectal cancer, especially in a parent or sibling diagnosed before age 60, you may need to start screening at 40-or even earlier. The same goes for people with inherited syndromes like Lynch syndrome or familial adenomatous polyposis (FAP). These conditions can cause dozens to hundreds of polyps, turning cancerous by your 30s.
People with inflammatory bowel disease (IBD)-Crohn’s disease or ulcerative colitis-also need earlier and more frequent screening. After 8-10 years of IBD, your risk of colon cancer increases significantly. Doctors often recommend colonoscopy every 1-2 years starting at age 40 or sooner.
African Americans have the highest incidence and mortality rates from colorectal cancer in the U.S. They’re 20% more likely to get it and 40% more likely to die from it. Guidelines now recommend colonoscopy as the preferred screening method for this group, not just stool tests. Starting at 45 is critical.

Chemotherapy for Colorectal Cancer: When and How It’s Used
Screening saves lives-but if cancer is found, treatment begins. Chemotherapy isn’t used for early-stage polyps or stage I cancer. Once cancer has spread beyond the inner lining of the colon or rectum, chemo becomes part of the plan.
For stage II and III colorectal cancer, chemotherapy after surgery (called adjuvant therapy) reduces the risk of recurrence. The most common regimens are:
- FOLFOX: Fluorouracil (5-FU), leucovorin, and oxaliplatin. This combo is used in 60% of stage III cases.
- CAPOX (XELOX): Capecitabine (an oral pill) and oxaliplatin. It’s just as effective as FOLFOX but avoids IV infusions.
- 5-FU with leucovorin: Older, less intense option for patients who can’t tolerate oxaliplatin.
Oxaliplatin can cause nerve damage-numbness or tingling in hands and feet-that sometimes lasts for months or years. This side effect is why some patients choose CAPOX: they can take the pill at home and avoid the IV.
For stage IV (metastatic) cancer, chemo is used to control growth and extend life, not cure it. Targeted drugs like cetuximab or bevacizumab are often added to chemo regimens if the tumor has certain genetic markers (like RAS wild-type). Immunotherapy works only in about 5% of cases-those with mismatch repair deficiency (dMMR) or microsatellite instability-high (MSI-H) tumors.
Chemotherapy isn’t easy. Nausea, fatigue, hair loss, and low blood counts are common. But survival rates have improved. Five-year survival for stage III cancer is now over 70% with modern chemo. For stage IV, it’s jumped from under 10% in the 1990s to nearly 15% today-and some patients live much longer.
Barriers to Screening-and How to Overcome Them
Despite the evidence, only 67% of adults aged 50-75 are up to date with screening. In uninsured people, that number drops to 58%. Rural areas have even worse access: only 32% of clinics offer patient navigators to help people schedule tests, compared to 87% in urban hospitals.
One of the biggest problems? Lack of follow-up. If a stool test comes back positive, many people don’t get the recommended colonoscopy. About 30% of people with a positive FIT never complete the next step. That’s where patient navigators help. They call, send reminders, help with transportation, and answer questions. Clinics that use them see a 35% increase in screening completion.
Automated reminders-texts, emails, or phone calls from your doctor’s office-boost adherence by 28%. Team-based care, where nurses and medical assistants handle prep instructions and scheduling, cuts no-show rates by 42%.
Cost is another barrier. Medicare covers colonoscopy with no copay for people 45-75. But if you’re uninsured, a colonoscopy can cost $3,000 or more. Many states now offer free or low-cost screening programs through public health departments. Ask your local health clinic. You might qualify.
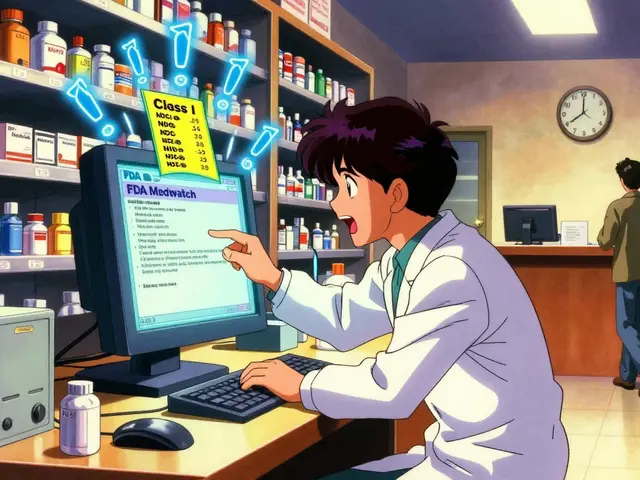
What Comes Next: Blood Tests and AI
The future of screening is getting less invasive. In 2023, a blood test called Guardant SHIELD showed 83% sensitivity for detecting colorectal cancer in a trial of 10,000 people. It’s not ready for prime time yet, but it’s coming fast. Another promising approach is methylation-based blood tests that detect cancer DNA changes. These could one day be part of a multi-cancer early detection panel.
AI is already here. The FDA-approved GI Genius system uses artificial intelligence to highlight polyps during colonoscopy. In a 2022 Lancet study, it increased adenoma detection by 14%. That means more cancers caught early.
By 2030, experts predict personalized screening will be the norm. Instead of everyone getting a colonoscopy at 45, you’ll get a risk score based on your genes, diet, weight, and lifestyle. Low-risk? Maybe a stool test every 5 years. High-risk? Colonoscopy every 3-5 years. This could cut unnecessary procedures by 30% without losing effectiveness.
Bottom Line: Don’t Wait
Colorectal cancer is preventable. It’s treatable. But only if you act. If you’re 45 or older, talk to your doctor about screening. Don’t wait for symptoms-by then, it’s often too late. Colonoscopy is the best tool we have. If you’re scared of the prep or the procedure, ask about alternatives. But don’t skip it.
One screening could mean the difference between living 10 more years and not seeing your grandkids grow up. That’s not a gamble worth taking.
At what age should I start getting screened for colorectal cancer?
If you’re at average risk, start at age 45. This is the current standard recommended by the U.S. Preventive Services Task Force, the American Cancer Society, and the American College of Gastroenterology. If you have a family history of colorectal cancer, inflammatory bowel disease, or a genetic syndrome like Lynch syndrome, you may need to start earlier-sometimes as early as age 40 or even younger. Talk to your doctor about your personal risk.
Is colonoscopy the only way to screen for colorectal cancer?
No. Other options include annual FIT (fecal immunochemical test), every-three-years multi-target stool DNA test (like Cologuard), and CT colonography every five years. But colonoscopy is the only test that can both detect and prevent cancer by removing precancerous polyps during the same procedure. If you choose a stool test and it’s positive, you’ll still need a colonoscopy to confirm.
How often do I need to get screened?
If you have a normal colonoscopy with no polyps, you don’t need another for 10 years. If you have one or two small adenomas, you’ll need another in 5-7 years. For FIT, do it every year. For stool DNA tests, every 3 years. For CT colonography, every 5 years. Your doctor will adjust based on your results and risk factors.
What are the side effects of chemotherapy for colorectal cancer?
Common side effects include fatigue, nausea, vomiting, diarrhea, hair loss, and low blood counts. Oxaliplatin, a key drug in FOLFOX and CAPOX regimens, can cause nerve damage leading to tingling or numbness in hands and feet-sometimes lasting months after treatment ends. Most side effects improve after treatment stops. Your care team can help manage them with medications and lifestyle changes.
Can colorectal cancer be cured if caught early?
Yes. When caught at stage I-before it spreads beyond the colon wall-the 5-year survival rate is over 90%. Even at stage II and III, modern surgery and chemotherapy can lead to long-term survival in 70% or more of cases. The key is early detection through screening. By the time symptoms appear, the cancer is often advanced and harder to treat.
Are there free or low-cost screening programs available?
Yes. Many states and local health departments offer free or low-cost colorectal cancer screening for uninsured or underinsured adults. Medicare covers colonoscopy with no out-of-pocket cost for people 45-75. Medicaid coverage varies by state. Contact your state health department or visit the CDC’s screening program website to find options near you.





It's astonishing how many people still treat colorectal cancer screening as a discretionary wellness activity rather than a non-negotiable medical imperative. The data is unequivocal: a 67% reduction in incidence via colonoscopy isn't a suggestion-it's a statistical lifeline. The fact that 30% of individuals with a positive FIT never follow up with colonoscopy reflects a dangerous conflation of discomfort with insignificance. We are not discussing a minor inconvenience; we are discussing preventable mortality.
The normalization of stool-based tests as adequate substitutes is a public health misstep. While FIT has utility in resource-limited settings, it is not equivalent to direct visualization. Polyps are not binary events-they are dynamic, evolving lesions. Waiting for blood or DNA markers is like waiting for smoke before checking the oven. Colonoscopy remains the gold standard because it intervenes, not just observes.
And let’s not romanticize the prep. Yes, it’s unpleasant. But comparing it to childbirth or dental surgery is hyperbolic and unhelpful. The real issue is systemic: lack of patient navigation, inadequate insurance transparency, and cultural stigma around bowel health. These are fixable. The science isn’t the barrier. The bureaucracy is.
I’ve seen too many friends delay screening because they were afraid of the prep or thought they were ‘too healthy’ to need it. One of my colleagues, 48, ignored symptoms for a year because she ‘didn’t want to be that person’ who complains about her gut. She ended up with stage III cancer. Now she’s doing chemo and wishes she’d just done the colonoscopy at 45 like her doctor said.
It’s not about being dramatic-it’s about being proactive. We talk about mental health, sleep, and exercise, but bowel health? Still taboo. Maybe we need to reframe this: colonoscopy isn’t about fear. It’s about control. You get to choose whether your body becomes a statistic-or a success story.
And yes, the side effects of chemo are brutal. But modern protocols have improved so much. I know someone on CAPOX who works remotely, takes her pills with breakfast, and still hikes on weekends. It’s not easy, but it’s not the end of the world either. Early detection changes everything.
man i just got my first colonoscopy last month at 46 and honestly? the prep was the worst part. like, i thought i was ready but wow. drank the whole thing and felt like i was gonna die. but the actual procedure? slept through it. woke up and they were like ‘all good, no polyps’. felt like i won the lottery. if you’re scared, just do it. it’s over faster than your morning coffee.
It is interesting how medical guidelines evolve with epidemiological data, yet societal attitudes lag behind. In India, where colorectal cancer incidence is rising rapidly, screening remains inaccessible to most. The conversation here often centers on cost and infrastructure-but perhaps we should also reflect on the cultural silence surrounding bowel health. Why is it that we discuss hypertension or diabetes openly, yet avoid mentioning colonoscopies as if they were shameful?
There is dignity in prevention. The fact that a simple procedure can prevent suffering, death, and financial ruin should make it a civic duty, not a privilege. I hope that as global awareness grows, we do not replicate the American model of inequality in access. Screening should be a right, not a reward for the insured.
yo if you’re 45+ and haven’t done a screen yet-just do it. i waited till 48 because i thought i was fine. turns out i had a polyp the size of a pea. removed in 10 mins. no big deal. now i tell everyone: your gut doesn’t care if you’re ‘too busy’ or ‘not sick yet’. it just grows. don’t be that guy who regrets it later. your future self will thank you.
So let me get this straight-we’ve got AI systems that can spot polyps better than some gastroenterologists, blood tests on the horizon that might make colonoscopies feel like medieval rituals, and yet we’re still having people argue about whether the prep is ‘too hard’?
It’s like refusing to wear a seatbelt because the buckle feels awkward. The tech is here. The data is clear. The only thing left is willpower. And apparently, we’ve run out of that.
Also, can we stop pretending that ‘I’m healthy so I don’t need it’ is a valid argument? Cancer doesn’t knock. It just shows up. And by then, it’s already thrown a party in your colon.
While I commend the thoroughness of this article, I must emphasize that the continued reliance on colonoscopy as the primary screening modality reflects a systemic bias toward invasive, high-cost interventions rather than scalable, population-level solutions. The emphasis on patient navigation and automated reminders is commendable, yet insufficient without structural investment in public health infrastructure. Furthermore, the normalization of colonoscopy as the default-particularly for African Americans, who face disproportionate disparities in care-risks reinforcing medical paternalism rather than empowering informed choice.
Why not prioritize equitable access to multi-target stool DNA testing as a first-line option, with colonoscopy reserved for high-risk or positive cases? This approach would reduce unnecessary procedures, lower costs, and increase adherence. The goal should not be to make colonoscopy more palatable, but to make screening more accessible. Prevention is not a luxury reserved for those who can tolerate a laxative.
I did the stool test. Got a positive result. Went to the colonoscopy. They found nothing. Now I feel like a sucker for falling for this medical scam. $1,200 later and I’m just glad I didn’t die from anxiety. If I’d known the false positive rate was 13%, I’d have just ignored it and ate my bacon.