Understanding Secondary Hypogonadism
Before we delve into the connection between secondary hypogonadism and the aging process, it's crucial to grasp what secondary hypogonadism is. It's a condition that impacts the production of testosterone in men and estrogen in women. However, unlike primary hypogonadism, which is caused by problems directly in the testes or ovaries, secondary hypogonadism arises from issues with the pituitary gland or hypothalamus—parts of the brain that signal the sex organs to produce hormones. It's a complex condition that requires a thorough understanding before we can begin to explore its relationship with aging.
Causes of Secondary Hypogonadism
Secondary hypogonadism can be caused by a variety of factors. Certain diseases such as HIV/AIDS, pituitary disorders, and inflammatory diseases can lead to the onset of this condition. It can also be caused by obesity, rapid weight loss, medication side effects, or even severe emotional stress. It's important to remember that this condition doesn't discriminate based on age. Both young and old people can develop secondary hypogonadism, although the causes may differ.
Symptoms of Secondary Hypogonadism
The symptoms of secondary hypogonadism can vary widely depending on the individual and their hormone levels. In men, symptoms might include erectile dysfunction, decreased body hair, loss of muscle mass, and decreased libido. Women may experience menstrual irregularities, hot flashes, and decreased sexual desire. It's important to note that these symptoms can also be related to other health conditions, so it's crucial to seek a professional diagnosis if you're experiencing any of these issues.
Secondary Hypogonadism and Aging
As we age, our bodies naturally undergo numerous changes, and our hormone production is no exception. While the reduced hormone production associated with aging doesn't necessarily cause secondary hypogonadism, it can exacerbate the condition for those who already have it. Additionally, aging can also bring about conditions like obesity or pituitary disorders, which are known to cause secondary hypogonadism.
The Impact of Aging on Testosterone Levels
Testosterone levels naturally decrease as men age. This decline often begins around middle age and continues gradually into the later years. This natural decrease is sometimes mistaken for secondary hypogonadism, but it's important to differentiate between the two. While a decline in testosterone is a normal part of aging, secondary hypogonadism is a medical condition that requires treatment.
Diagnosing Secondary Hypogonadism
Diagnosing secondary hypogonadism can be a complex process. It typically involves blood tests to measure hormone levels, and may also include imaging tests to check for abnormalities in the pituitary gland or hypothalamus. It's important to seek a diagnosis if you're experiencing symptoms, as untreated secondary hypogonadism can lead to serious health complications such as osteoporosis.
Treatment Options for Secondary Hypogonadism
Treatment for secondary hypogonadism often involves hormone replacement therapy to restore normal hormone levels. In some cases, treating the underlying cause of the condition, such as obesity or a pituitary disorder, can also help manage the symptoms. It's crucial to consult with a healthcare professional to determine the most appropriate treatment plan for you.
Living with Secondary Hypogonadism
Living with secondary hypogonadism can be challenging, but it's important to remember that it's a manageable condition. With proper treatment, most people can live normal, healthy lives. Engaging in regular physical activity, maintaining a healthy weight, and managing stress can all help manage the symptoms and improve your quality of life.
Conclusion: Secondary Hypogonadism and the Aging Process
In conclusion, while secondary hypogonadism can be impacted by the aging process, it's a separate condition that requires medical diagnosis and treatment. As we age, it's crucial to pay attention to our bodies and seek medical advice if we notice changes that concern us. With a proactive approach to health and wellness, it's possible to manage secondary hypogonadism and maintain a high quality of life into our golden years.






Let's be real-this article reads like a pharmaceutical brochure. 'Secondary hypogonadism' is just a fancy term doctors use to sell you testosterone patches while ignoring that most men over 40 are just sedentary, eating junk, and blaming biology. You don't need hormone therapy-you need to lift weights, sleep 7 hours, and stop drinking soda. The pituitary gland isn't broken; your lifestyle is.
Wait-hold on-this is... uh... problematic... I mean, the article says 'testosterone levels naturally decrease'-but does it, though? I mean, according to the 2017 JAMA study (doi:10.1001/jama.2017.0000), the decline is only significant in men with BMI >30, and even then-it's not 'secondary hypogonadism' unless LH/FSH are low-so, if you're just aging and your LH is normal? You're not hypogonadal-you're just... old. And yes-I capitalized 'JAMA' because it's an acronym, and you're supposed to do that.
I appreciate the clarity here, but I think we need to be careful about how we frame aging and hormone decline. For many people, especially women going through perimenopause, the line between 'normal aging' and 'medical condition' is blurry-and it's not just about testosterone or estrogen. It's about dignity, quality of life, and not being told you're 'just getting old' when you're struggling with fatigue, brain fog, and low libido. If someone feels off, they deserve to be heard-not dismissed as 'just aging.' Maybe the real issue isn't the hormone levels-it's that we don't take midlife health seriously enough.
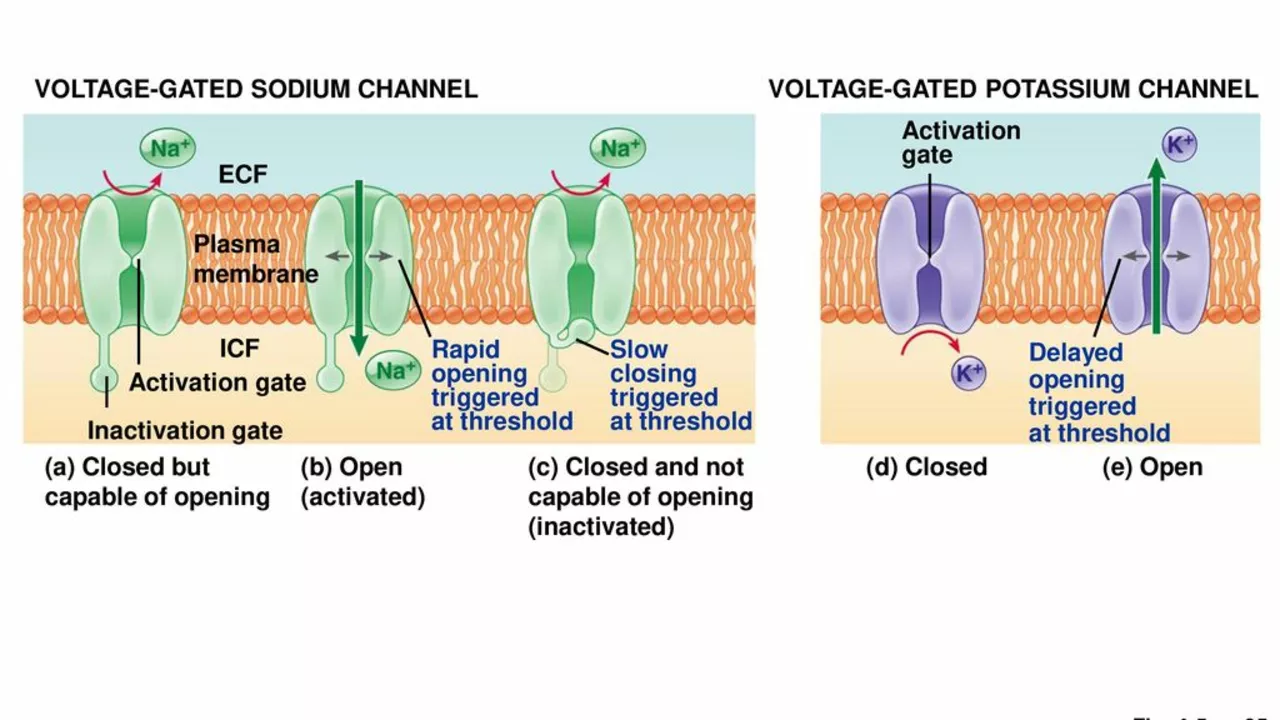
It's critical to differentiate between age-related physiological decline and pathological hypogonadism, as the former is a neuroendocrine adaptation to chronic energy imbalance and systemic inflammation, whereas the latter involves hypothalamic-pituitary-gonadal axis dysfunction-often manifesting as low gonadotropins in the context of low sex steroids, which necessitates a dynamic stimulation test, not just a single serum testosterone measurement. Moreover, the diagnostic criteria outlined in the Endocrine Society Guidelines (2018) require exclusion of confounding variables including sleep apnea, chronic opioid use, and hyperprolactinemia-all of which are prevalent in aging populations and may mimic secondary hypogonadism.
Hey, I get that this stuff can be confusing. The key thing is: if you're tired all the time, losing muscle, or just not feeling like yourself-don't just brush it off as 'getting old.' Talk to your doctor. Get your levels checked. And if they say 'it's normal,' ask for a second opinion. There's no shame in wanting to feel good in your body, no matter your age. I've seen guys in their 60s turn their lives around with simple fixes-sleep, protein, lifting, and sometimes, yes, a little help from hormones. You deserve to feel strong. Don't give up.