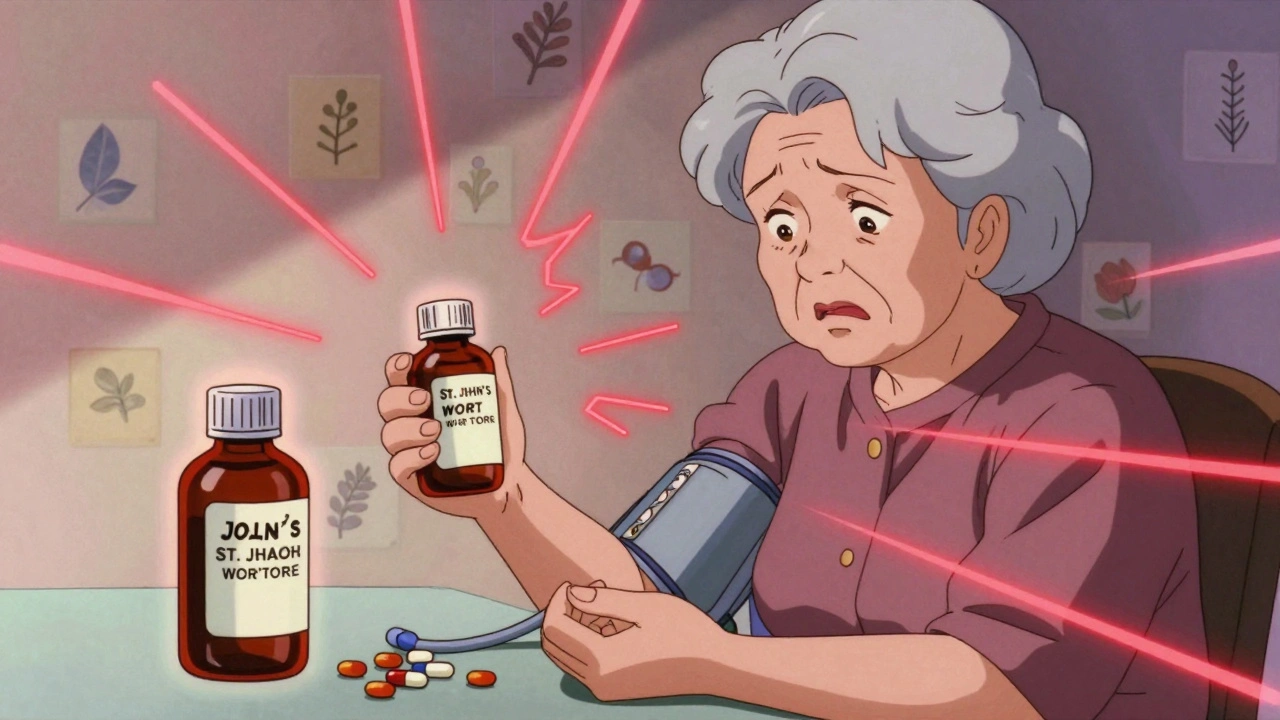
When you take a drug-supplement interaction, a harmful or reduced effect that happens when a medication and a supplement affect each other in your body. Also known as medication-supplement conflict, it can turn a safe routine into a health risk—no matter how natural the supplement seems. Many people assume that because something is sold as a "natural remedy" or "herbal supplement," it’s harmless. But that’s not true. Garlic pills, St. John’s wort, magnesium, or even vitamin K can change how your blood thinner, antidepressant, or antibiotic works—sometimes with life-threatening results.
Take warfarin, a blood thinner that requires precise dosing and is sensitive to diet and supplements. Also known as Coumadin, it’s one of the most common drugs involved in dangerous interactions. A daily vitamin K supplement can make warfarin less effective, raising your risk of stroke. On the flip side, taking St. John’s wort with warfarin can cause dangerous bleeding. This isn’t theory—it’s why doctors ask about every pill, powder, or tea you take. The same goes for antibiotics, like doxycycline or ciprofloxacin, which can lose up to 90% of their power if taken with antacids or calcium supplements. Also known as antibiotic interference, this is one of the most preventable mistakes in medicine. Timing matters: take your antibiotic two hours before or after your antacid. Most people don’t know this—and pharmacies rarely warn them.
It’s not just about prescription drugs. Even over-the-counter painkillers like ibuprofen can react badly with fish oil or ginkgo biloba, increasing bleeding risk. People with diabetes, high blood pressure, or thyroid conditions are especially vulnerable because their meds have narrow safety margins. One small change in how your body absorbs or breaks down a drug can throw everything off. That’s why pharmacy safety, the practice of checking all medications and supplements together before dispensing. Also known as medication review, it’s a critical step that’s often skipped in busy clinics. And if you’re getting meds from a mail-order pharmacy or compounding lab, you’re even more at risk—because no one’s asking what else you’re taking.
You don’t need to stop your supplements. You just need to know which ones are safe with your meds. The FDA gets thousands of reports each year about people ending up in the ER because they didn’t realize their turmeric capsule was interfering with their blood pressure pill. You can avoid that. Start by making a list: every prescription, every vitamin, every herbal tea, every probiotic. Bring it to your doctor or pharmacist—not just once, but every time you get a new prescription. Ask: "Could this interact with anything else I’m taking?" Don’t assume they know. Don’t assume it’s harmless. The safest supplement is the one you’ve checked.
Below, you’ll find real stories and science-backed guides on how these interactions happen, which ones are most dangerous, and exactly what to do to protect yourself—from warfarin and antibiotics to common OTC combos that catch people off guard. No fluff. Just what works.
Many supplements can dangerously interact with medications, reducing their effectiveness or causing life-threatening side effects. Learn which ones to avoid, how to check for risks, and what steps to take before taking any supplement with your prescriptions.
