When a standard pill doesn’t work—or causes side effects you can’t tolerate—customized medications, medications made specifically for an individual’s body, allergies, or dosing needs. Also known as compounded drugs, they’re not mass-produced. Instead, they’re mixed by pharmacists to match what a patient actually needs. This isn’t science fiction. It’s daily practice for people with rare allergies, swallowing problems, or conditions that need exact doses not available in stores.
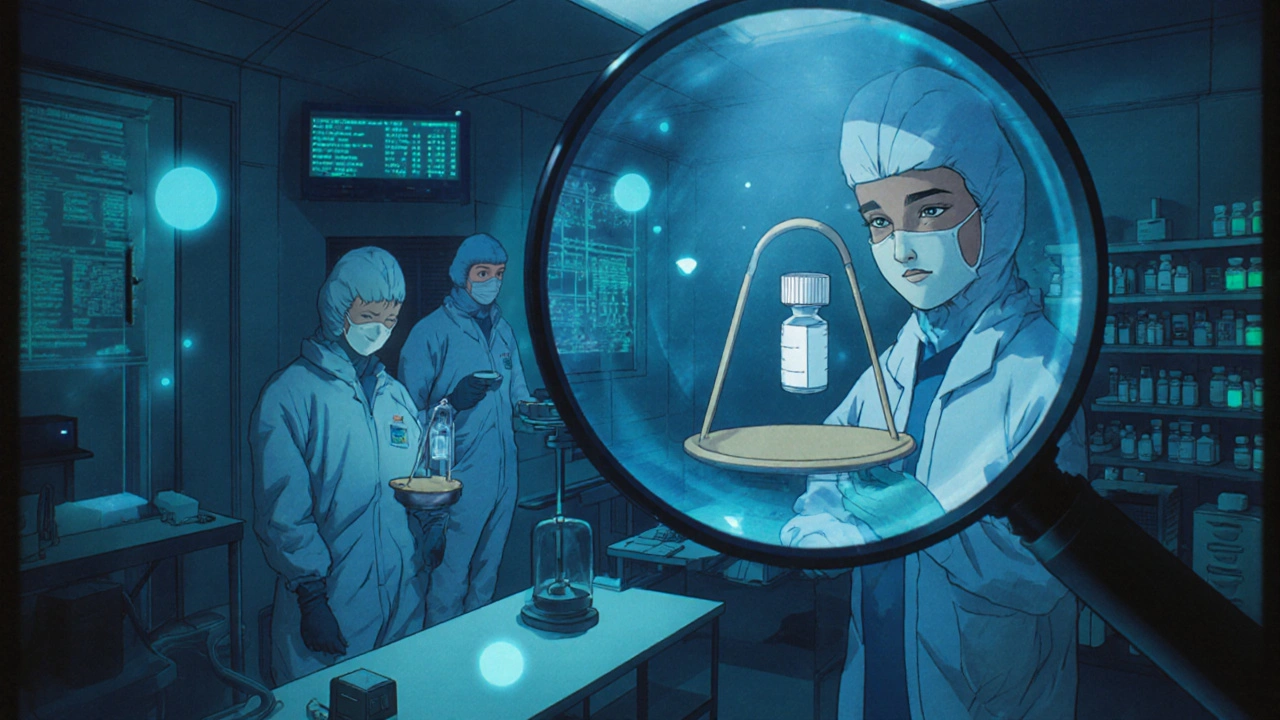
Customized medications often come from compounding pharmacies, specialized labs that mix ingredients to create unique formulations. These aren’t the same as regular pharmacies. They don’t just fill prescriptions—they build them. Need a hormone cream without dye? A pain pill without lactose? A child’s liquid antibiotic without sugar? That’s their job. And while the FDA doesn’t approve each batch like it does with big pharma drugs, it does require these pharmacies to follow strict clean-room and quality rules under USP standards.
There’s also a quiet overlap between customized meds and bioequivalent medications, generic versions proven to act the same in your body as brand-name drugs. Sometimes, what feels like a custom solution is just a generic version with a different filler. The FDA checks these generics to make sure they release the same amount of active ingredient at the same rate. That’s why switching from brand to generic usually works—but not always. If your body reacts differently, your doctor might turn to compounding to fine-tune the formula.
People often think customized meds are only for rare diseases. But they’re also used for everyday issues: seniors who can’t swallow pills, athletes needing precise hormone levels, or patients with chronic pain needing topical creams instead of oral drugs. The goal is simple: give you the right medicine, in the right form, at the right dose—without unnecessary chemicals or side effects.
But it’s not magic. Customized medications require more communication. You need to track how you feel, report side effects clearly, and understand that not all compounding pharmacies are equal. Some follow high standards. Others cut corners. The FDA has stepped up oversight in recent years, especially after outbreaks linked to unsafe compounding. That’s why knowing where your med comes from matters as much as what’s in it.
Below, you’ll find real-world guides on how these systems work—from how the FDA tests generic versions to how patients use compounded drugs to avoid allergic reactions. You’ll see how bioequivalence isn’t always enough, why some people need pills made from scratch, and how to spot the difference between quality and risk. Whether you’re managing thyroid levels, chronic pain, or a reaction to a common filler, the answers here are practical, not theoretical. No fluff. Just what you need to know to get the right treatment.
Learn how to prevent dangerous errors in customized medications through dual verification, proper labeling, cleanroom standards, and accreditation. Essential safety steps for pharmacists and patients alike.
