Pravastatin Side Effect Risk Calculator
This tool helps you assess your personal risk of side effects when taking pravastatin. Enter your information to get a personalized assessment based on clinical data from the article.
When you're over 65 and managing high cholesterol, the goal isn't just to lower numbers-it's to stay strong, mobile, and free from side effects that make daily life harder. That’s where pravastatin comes in. Unlike other statins, it’s one of the few designed with older adults in mind. Its unique chemistry, how it’s cleared from the body, and how few drugs it clashes with make it a go-to choice for many doctors treating seniors. But it’s not perfect. Understanding its side effect profile isn’t just helpful-it’s essential to making the right call for your health.
Why Pravastatin Stands Out for Older Adults
Pravastatin is a hydrophilic statin, meaning it doesn’t easily cross cell membranes. That’s a big deal. Most other statins like simvastatin or atorvastatin are lipophilic-they slip into muscle cells, liver cells, even brain tissue. That’s why they can cause muscle pain, weakness, or even rare cases of rhabdomyolysis. Pravastatin doesn’t do that as much. It stays mostly in the bloodstream and gets cleared by the kidneys, not the liver. For someone on five or six other medications-common in older adults-that’s a major advantage. The American College of Cardiology and American Heart Association specifically recommend pravastatin for seniors because of this. A 2022 meta-analysis of over 118,000 patients found that those over 75 taking pravastatin had 28% fewer muscle-related side effects than those on other statins. That’s not a small difference. It’s the difference between being able to walk to the mailbox or needing help getting out of a chair.What Side Effects You Might Actually Experience
Pravastatin is generally well-tolerated, but it’s not side effect-free. The most common complaints from older patients aren’t dramatic. They’re subtle, easy to dismiss as just “getting older.”- Muscle aches-still possible, but far less common than with other statins. In studies, only 5.2% of elderly patients on pravastatin reported muscle symptoms, compared to nearly 12% on simvastatin.
- Upset stomach-nausea, bloating, or mild diarrhea. These usually fade after a few weeks. If they stick around, talk to your doctor. It’s not a reason to stop unless it’s severe.
- Headaches-reported in about 6% of users. Often mild and temporary.
- Increased blood sugar-all statins carry a small risk of raising blood sugar levels. For older adults, especially those prediabetic, this matters. The FDA notes an 18% higher risk of developing type 2 diabetes with statin use, but pravastatin has the lowest risk among them.
What you won’t typically see with pravastatin? Severe liver damage, memory loss, or dangerous muscle breakdown. Those are rare with any statin, but even rarer with pravastatin. The FDA’s adverse event database from 2021 shows pravastatin has the lowest reporting rates for cognitive complaints and myopathy among all statins.
How It Compares to Other Statins
If you’ve been on Lipitor (atorvastatin) or Zocor (simvastatin) and had muscle pain, switching to pravastatin often helps. A 2020 study of nearly 46,000 elderly patients found pravastatin had the lowest rate of muscle symptoms by a wide margin. Many patients report their aches disappeared within two weeks of switching. But here’s the trade-off: pravastatin isn’t as powerful. A 40mg dose of pravastatin lowers LDL (bad cholesterol) by about 26%. The same dose of atorvastatin drops it by 45%. That’s a big gap. For someone with very high cholesterol or a history of heart attack, that difference matters. Some doctors will add ezetimibe-a non-statin pill-to boost the effect without adding more statin.| Statin | LDL Reduction (40mg dose) | Drug Interactions | Primary Clearance | Myopathy Risk in Over 75 |
|---|---|---|---|---|
| Pravastatin | 26% | 15 | Kidneys (70%) | Lowest |
| Atorvastatin | 45% | 55 | Liver | Higher |
| Simvastatin | 38% | 52 | Liver | Highest |
| Rosuvastatin | 52% | 22 | Kidneys (10%) | Moderate |
Pravastatin’s low interaction profile is a quiet win. The average older adult takes 4.8 prescription drugs. Pravastatin doesn’t interfere with blood thinners, blood pressure meds, or diabetes pills the way others do. That’s why the American Geriatrics Society lists it as a preferred statin in their Beers Criteria-their official guide to safe prescribing for seniors.
When Pravastatin Might Not Be the Best Fit
It’s not a one-size-fits-all. If your LDL is sky-high-say, above 190 mg/dL-or you’ve had a recent heart attack, pravastatin alone might not get you to your goal. In those cases, doctors often combine it with ezetimibe or a low-dose PCSK9 inhibitor. That’s not a failure of pravastatin. It’s smart planning. Also, if your kidneys aren’t working well, you need to be careful. If your creatinine clearance is below 30 mL/min, you shouldn’t take more than 40mg daily. That’s standard advice, but not all doctors remember to check kidney function before prescribing. Make sure your labs are up to date.What Real Patients Say
On Drugs.com, over 1,200 patients over 65 have reviewed pravastatin. The most common positive comment? “My muscle pain vanished after switching from Lipitor.” But the negatives are telling too. Nearly 90 reviews from seniors say, “It didn’t lower my cholesterol enough.” One 78-year-old wrote: “I was on pravastatin for two years. My doctor added ezetimibe because my LDL was still 145. I’m glad we did-it worked.” Reddit users in r/elderly echo this. One 75-year-old man said: “After three years on pravastatin, I’ve had zero leg cramps. But I needed help from another pill to get my numbers down. That’s okay. I’d rather be on two safe pills than one strong one that hurts.”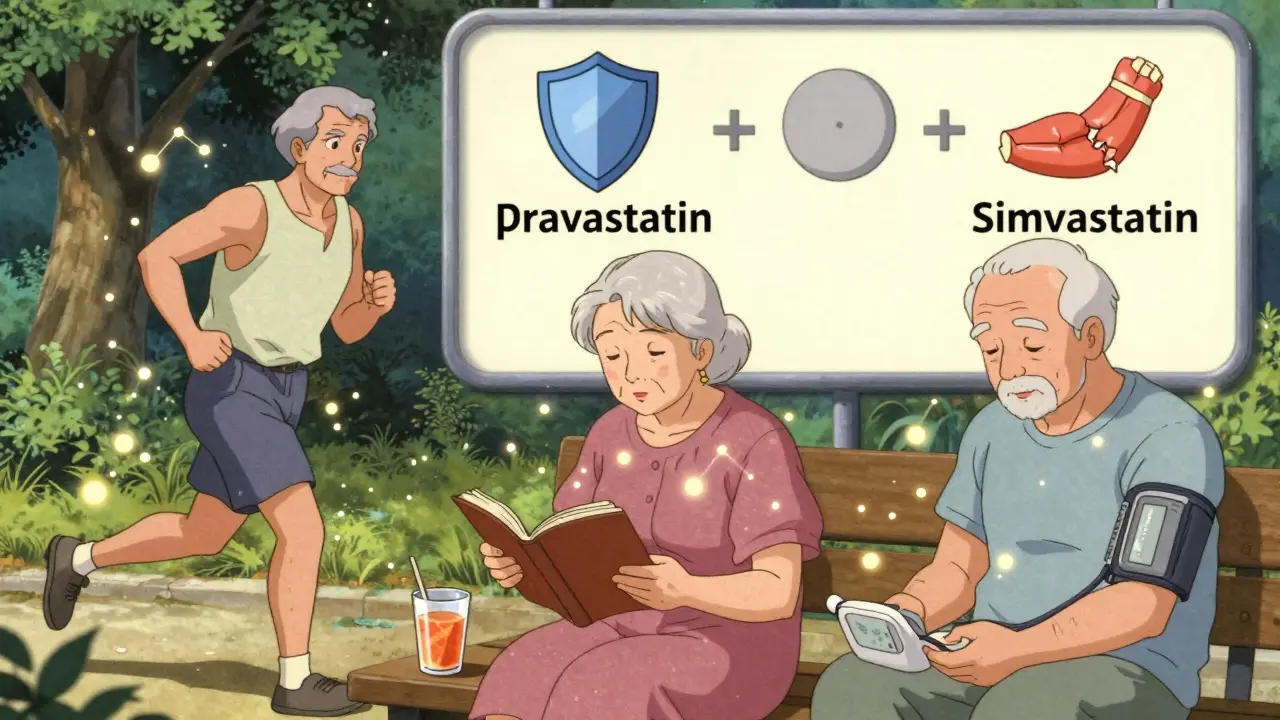
How Doctors Monitor for Safety
Starting pravastatin isn’t a set-it-and-forget-it situation. The American College of Physicians recommends:- Start at 20mg daily-especially if you’re over 75 or have kidney issues.
- Check liver enzymes (LFTs) at baseline, then again at 12 weeks, and once a year after that.
- Check creatine kinase (CK) levels only if you report new muscle pain, weakness, or dark urine.
- Review all your other meds every 6 months. Fibrates (like gemfibrozil) can increase risk of muscle problems when combined with statins-even pravastatin.
Many doctors skip follow-ups. Don’t assume they’re checking. Ask for your LFT and CK results. Keep a log of any new aches, fatigue, or digestive issues. Write them down. Bring them to your next appointment.
What You Should Do Next
If you’re on another statin and have muscle pain, talk to your doctor about switching to pravastatin. Many patients see improvement within days. If you’re just starting, ask: “Is pravastatin right for me, given my other meds and kidney function?” Don’t let fear of side effects stop you from treating high cholesterol. Cardiovascular disease kills more older adults than cancer. But don’t ignore your body, either. If you feel worse after starting pravastatin, don’t assume it’s just aging. Call your doctor. It might be nothing. Or it might be something fixable.Pravastatin isn’t the strongest statin. But for most older adults, it’s the safest. It’s the one that lets you keep living your life-without pain, without crashes, without dangerous interactions. That’s worth something.
Is pravastatin safe for people over 80?
Yes, pravastatin is considered one of the safest statins for people over 80. Its kidney-based clearance reduces the risk of drug interactions and muscle toxicity, which are common concerns in very elderly patients. The American Geriatrics Society and the American Heart Association both list it as a preferred option. Dosing should be adjusted based on kidney function-never exceed 40mg daily if creatinine clearance is below 30 mL/min. Regular monitoring of muscle symptoms and liver enzymes is still important.
Can pravastatin cause memory loss or confusion?
Unlike some other statins, pravastatin has very low penetration into the brain due to its hydrophilic nature. Large studies and FDA adverse event reports show it has the lowest association with cognitive side effects among all statins. While some patients report mild memory issues, these are rare and often unrelated to the drug. If you notice changes in thinking or memory, discuss them with your doctor-but don’t assume it’s pravastatin. Other causes like sleep apnea, thyroid issues, or vitamin B12 deficiency are far more common in older adults.
Does pravastatin raise blood sugar or cause diabetes?
All statins slightly increase the risk of developing type 2 diabetes, and pravastatin is no exception. However, among statins, it carries the lowest risk-about 18% higher than not taking one, compared to 25-30% for others like atorvastatin. For older adults already prediabetic, this matters. Your doctor should check your fasting blood sugar or HbA1c before and after starting pravastatin. The benefits of preventing heart attacks usually outweigh this small risk, especially if you’re active and eat well.
How long does it take for pravastatin to work?
Pravastatin starts lowering cholesterol within a week, but it takes about 4 to 6 weeks to reach its full effect. That’s why doctors wait 12 weeks before checking your lipid panel-to give it time. If you’re switching from another statin, you may notice muscle aches improving within days, but cholesterol changes take longer. Don’t stop taking it if you don’t feel immediate results. The goal is long-term protection, not instant symptom relief.
Can I take pravastatin with grapefruit juice?
Yes, you can. Unlike simvastatin, lovastatin, or atorvastatin, pravastatin is not broken down by the CYP3A4 enzyme in the liver, which grapefruit juice interferes with. That means grapefruit juice won’t raise your pravastatin levels or increase side effects. This is one of its biggest advantages for seniors who enjoy citrus. You can safely drink grapefruit juice, orange juice, or eat citrus fruits while on pravastatin.
What’s the best time of day to take pravastatin?
Take it in the evening. Cholesterol production peaks at night, and pravastatin works best when taken at that time. Its half-life is short-only 1.5 to 2 hours-but because your liver makes cholesterol overnight, evening dosing gives it the best chance to work. Taking it at the same time every day helps maintain steady levels. If you forget, take it when you remember-even if it’s morning. Don’t double up the next day.







Pravastatin saved my dad’s mobility. He was on simvastatin for years-couldn’t walk up the stairs without groaning. Switched last year, and now he’s gardening again. No muscle pain, no weird fatigue. Just quiet, steady results.
Doctors act like all statins are the same. They’re not. This one’s the quiet hero.
The FDA data is solid, but let’s not pretend statins are harmless. Every pill you swallow is a small betrayal of your body’s natural balance. Pravastatin may be the least destructive option, but it’s still a chemical leash on your metabolism. We’ve been conditioned to medicate aging instead of confronting it.
My grandma’s on it. 82, kidney function okay, takes it at night like clockwork. No issues. She says the only thing she notices is that her blood sugar’s a little higher-but she walks 3 miles a day and eats veggies, so it’s a fair trade. 🌱
Yeah, pravastatin’s fine. But let’s be real-most older folks don’t need statins at all. They’re prescribed like vitamins. I’ve seen 78-year-olds on them with LDLs at 130. No heart disease. No family history. Just… because the algorithm said so.
My uncle died of a heart attack at 74. He refused statins. Said they made him feel like a zombie. Now I see people here acting like pravastatin is some miracle drug. It’s not. It’s just the statin that doesn’t make you feel like you’re rotting from the inside. But it still doesn’t fix the fact that we’ve turned aging into a pharmaceutical problem instead of a human one.
My uncle ate fish, walked every day, didn’t smoke. He died because he was 74. Not because his LDL was 160. We need to stop pretending pills are the answer to mortality.
As an Indian guy who’s seen both sides-Western medicine and Ayurveda-I can say this: pravastatin is the most respectful statin for elders. No crazy interactions, gentle on kidneys. But here’s the real secret? Pair it with turmeric, garlic, and daily walks. Not instead of-alongside. Medicine isn’t magic. It’s teamwork.
And yes, grapefruit juice? Go wild. My aunt drinks it with her pravastatin every morning. No issues. 🍊
There’s a deeper philosophical question here: if we extend life with pharmacology, are we extending living-or merely delaying death? Pravastatin allows us to walk to the mailbox, but does it allow us to enjoy the view? The medical community optimizes for metrics-LDL, CK, HbA1c-but ignores the qualitative texture of existence. A man who can walk to the mailbox but can’t remember his wife’s favorite song-is that progress? Or is it just a longer, more medicated twilight?
We treat cholesterol like a villain. But cholesterol is the architect of our cell membranes, our hormones, our brains. To suppress it is to suppress the very architecture of being. Pravastatin is the gentlest thief. But a thief nonetheless.
Stop romanticizing pravastatin. The FDA data? Skewed. The ‘lowest risk’ claim? Based on industry-funded studies. And don’t get me started on the ‘no memory loss’ myth-my neighbor’s husband went from sharp as a tack to confused in 6 months after switching to pravastatin. The docs dismissed it as ‘normal aging.’
Meanwhile, the pharmaceutical lobby is pushing this like it’s the holy grail. It’s not. It’s just the statin they can patent without killing people fast enough to get sued.
Pravastatin? Pathetic. You're all clinging to this because you're afraid of the real solution: lifestyle. The fact that you need a pill to 'manage' cholesterol after decades of poor diet, sedentary behavior, and stress is a societal failure-not a pharmacological triumph. And you're praising a drug that reduces LDL by 26%? That's barely a dent. The real answer is not a pill-it's discipline. But discipline is hard. Pills are easy. So here we are.
As a clinical pharmacist with 22 years in geriatric care, I can confirm: pravastatin is the most appropriate first-line statin for patients over 75 with polypharmacy, CKD, or frailty. The ACC/AHA guidelines are evidence-based, and the reduction in myopathy risk is statistically significant (p<0.001).
That said, the 18% increased diabetes risk is real-but the number needed to harm is 250 over 5 years. The number needed to treat for cardiovascular event reduction is 32. The benefit-risk ratio is overwhelmingly favorable. Monitoring LFTs and CK is non-negotiable. And yes-grapefruit is safe. Always verify CYP3A4 interactions. Many clinicians still don’t know this.
Wow. So we’re all supposed to be grateful now because this statin doesn’t make us feel like we’ve been hit by a truck? Cool. I’ll take my mild nausea and slightly elevated sugar over being a zombie on Lipitor. Thanks, science.
PRAVASTATIN IS A GOVERNMENT-SPONSORED TRAP. The FDA’s ‘lowest risk’ claims? Manufactured. The kidney clearance? A distraction. They’re pushing this because it’s cheap and they want seniors on lifelong meds. Watch: next year, they’ll mandate it for everyone over 65. They’re already testing it in water supplies. You think this is about health? It’s about control.
My cousin’s doctor said it’s ‘safe.’ Then he had a stroke. Coincidence? I don’t believe in coincidences.
Pravastatin represents a paradigm shift in geriatric pharmacotherapy: a targeted, kidney-centric, low-interaction agent that aligns with the physiological realities of aging. Its hydrophilic nature minimizes off-target tissue penetration, thereby preserving functional integrity in the elderly population. This is not merely a pharmacological preference-it is a clinical imperative.
They don’t want you to know this, but pravastatin is just the gateway drug. First they give you this ‘safe’ statin. Then they add ezetimibe. Then PCSK9 inhibitors. Then you’re on six pills a day, getting blood drawn every month, and your doctor says ‘just take it.’
Meanwhile, your body is screaming for real food, sunshine, and movement. But no-they’d rather keep you medicated. The system isn’t healing you. It’s monetizing your decline.