It’s not just about hot flashes and irregular periods. For many women in their 40s and early 50s, the real surprise of perimenopause isn’t the physical changes-it’s how emotional everything feels. One day you’re fine, the next you’re crying over a spilled cup of coffee or snapping at your partner for no clear reason. You feel like you’re losing control of yourself, and no one seems to understand why. The truth? You’re not imagining it. Your hormones are shifting in ways that directly affect your brain chemistry, and mood swings aren’t a sign of weakness-they’re a biological response.
Why Your Mood Feels Like a Rollercoaster
Perimenopause is the years-long transition before your periods stop completely. It usually starts in your early 40s but can begin as early as your mid-30s. During this time, estrogen and progesterone levels don’t just drop-they swing wildly. One week, estrogen might be high; the next, it plummets. These fluctuations happen without warning, and your brain doesn’t have time to adjust. Estrogen doesn’t just regulate your cycle. It’s deeply involved in producing serotonin and dopamine-the brain chemicals that help you feel calm, focused, and happy. When estrogen drops, so does serotonin. That’s why many women report feeling anxious, irritable, or suddenly overwhelmed. Progesterone, which has a calming effect by boosting GABA (your brain’s natural relaxant), also declines. Without enough progesterone, your nervous system stays on high alert. Add to that sleep problems-63% of perimenopausal women struggle with insomnia or night sweats-and it’s no surprise mood suffers. Poor sleep doesn’t just make you tired; it lowers your emotional resilience. A minor stressor becomes a meltdown. A quiet evening turns into an argument. You start wondering, “Is this me? Or is it the hormones?”It’s Not Just Depression-It’s Hormone-Driven
Many women are told they’re “depressed” and handed an antidepressant. But perimenopausal mood changes aren’t always clinical depression. They’re often a direct result of hormonal chaos. Research from Harvard Health shows that while 10%-20% of women experience significant mood symptoms during perimenopause, only about 20-30% of those cases are purely depression unrelated to hormones. The rest are tied to estrogen swings. There’s a key difference between perimenopausal mood changes and other types of depression. With clinical depression, symptoms are persistent. With perimenopause, they come in waves-sometimes daily, sometimes weekly, sometimes just after a stressful event. And unlike premenstrual dysphoric disorder (PMDD), which follows a monthly cycle, perimenopausal mood shifts are unpredictable and last for years. Women with a history of depression are five times more likely to have severe mood symptoms during this phase. But even women who’ve never struggled with mental health can suddenly feel like they’ve lost their emotional baseline. Reddit users describe it as “feeling like a different person.” One woman wrote: “I used to be patient. Now I yell at the dog for breathing too loud.”What Treatments Actually Work
There’s no one-size-fits-all fix, but the most effective approaches combine medical, lifestyle, and psychological strategies. Hormone Replacement Therapy (HRT) is the most direct solution for hormone-driven mood symptoms. Low-dose estrogen-either as a patch, gel, or pill-can stabilize mood in 45-55% of women within 2-3 months. It doesn’t just help with hot flashes; it rebuilds serotonin levels. The North American Menopause Society now recommends starting low-dose estrogen for moderate to severe mood symptoms, even if hot flashes aren’t the main issue. SSRIs and SNRIs (like sertraline or venlafaxine) help about half of women with mood symptoms. Interestingly, they work even at low doses-much lower than what’s used for clinical depression. And unlike HRT, they don’t require estrogen to be present to be effective. That’s why they’re often used for women who can’t take hormones due to breast cancer history or blood clot risks. Combination therapy-HRT plus a low-dose antidepressant-is the most effective for women with both severe mood swings and physical symptoms. A 2023 update from the North American Menopause Society found this combo improved mood in over 70% of cases.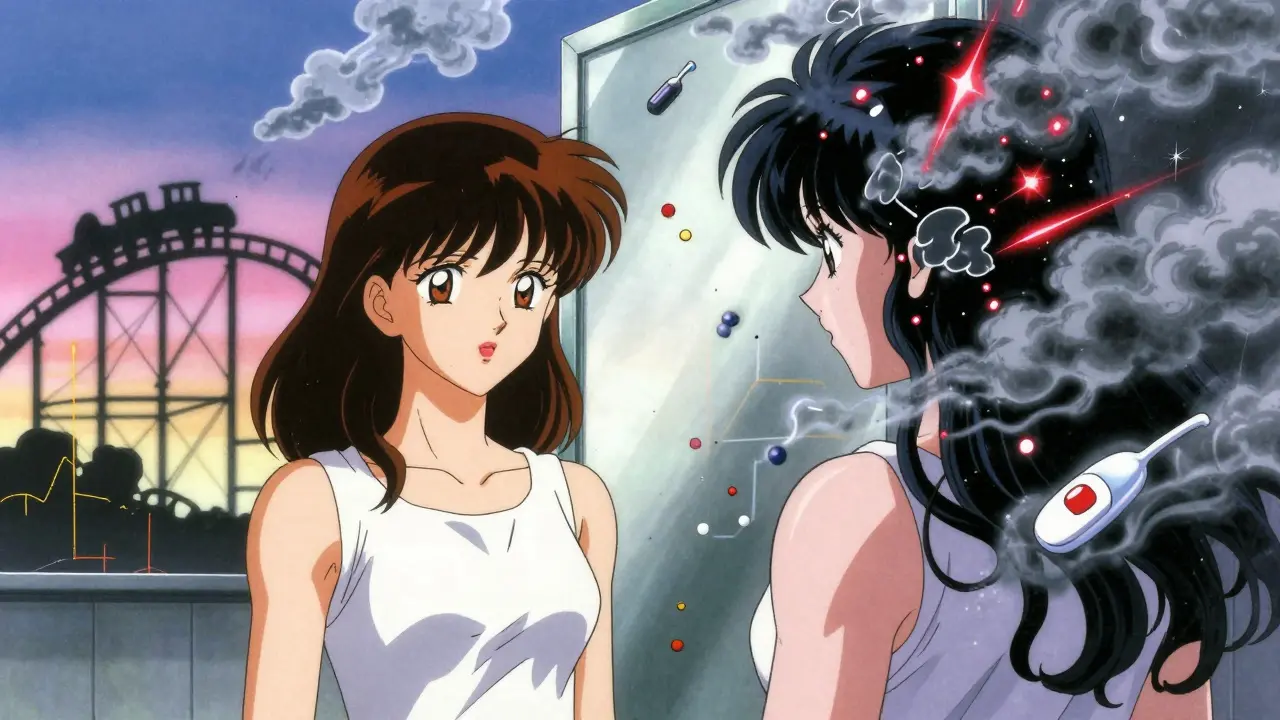
What Doesn’t Work (and Why)
Many women try herbal supplements like black cohosh or evening primrose oil. Some report feeling better, but clinical trials show no consistent benefit for mood. The FDA doesn’t regulate these supplements, so quality varies wildly. Don’t waste time or money on them if your mood is truly impacting your life. Therapy alone-without addressing hormones-often falls short. Cognitive behavioral therapy (CBT) helps with coping skills, but if your brain is flooded with unstable hormones, it’s like trying to fix a leaky roof during a hurricane. CBT works best when paired with hormone stabilization. And don’t wait until you’re in crisis to act. A 2022 study from My Menopause Centre found that women who waited more than a year to seek help took twice as long to find relief. Early intervention makes a huge difference.Lifestyle Changes That Actually Help
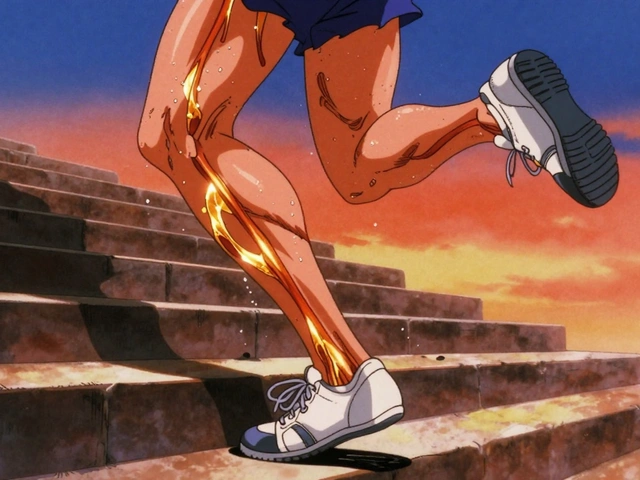
You can’t outrun hormones, but you can support your brain while they settle.- Exercise: Just 30 minutes of brisk walking or cycling five days a week boosts serotonin and reduces cortisol (the stress hormone). Strength training is especially helpful-it improves sleep and self-esteem.
- Sleep hygiene: Keep your bedroom cool, avoid screens an hour before bed, and try magnesium glycinate (200-400 mg) if you struggle to fall asleep. Poor sleep makes everything worse.
- Reduce caffeine and alcohol: Both disrupt sleep and amplify anxiety. Cutting back-even just on weekends-can calm your nervous system.
- Manage stress: Deep breathing, yoga, or even 10 minutes of quiet meditation daily lowers cortisol and improves emotional regulation.






Just wanted to say I felt seen reading this. I thought I was losing it until my sister mentioned perimenopause. Now I know it's not me being "dramatic"-it's my body trying to rewrite the code. Took me two years to find a CMP, but now I'm on low-dose estrogen and my anxiety has calmed down like a storm passing. You're not broken. You're upgrading.
So let me get this straight-women’s brains are just hormonal rollercoasters with a subscription to Netflix and a cat that judges them? I mean, I’ve seen men get cranky after beer, but this is like a whole season finale of "Your Hormones Are Sabotaging You" with a side of serotonin sabotage. Respect.
Big yasss to the HRT + SSRI combo data. I’ve been on transdermal estradiol 50mcg + low-dose sertraline 25mg since last fall. My cortisol spikes? Down 70%. My sleep efficiency? Up to 85%. The neuroendocrine feedback loops are wild-estrogen modulates 5-HT1A receptor sensitivity, and when you stabilize that, the emotional lability just... decays. Also, magnesium glycinate > melatonin for GABA tone. Just saying.
For anyone reading this and thinking "I don’t need meds," I get it. I resisted too. But after 18 months of crying in the grocery store over oat milk, I went to a menopause clinic. They ran a hormone panel, checked my vitamin D, and found I was estrogen-deficient with low progesterone. Started on a patch. Within 6 weeks, I stopped yelling at my dog. And yes, I still love him. Just not when he snores.
Bro, in India we call this "maa ki bimari"-the mother’s illness. No one talks about it. My aunt used to say "beta, you’re just tired." But now? My cousin’s a nurse in Delhi and she’s starting a WhatsApp group for perimenopausal women-sharing tips, doctors, even where to get bio-identical creams without the markup. We’re breaking the silence. And honestly? It’s about time.
Perimenopause isn’t the end of your story-it’s the prologue to your second act. You’re not fading. You’re evolving. The rage? The tears? The sudden urge to quit your job and move to Bali? That’s your soul screaming to be heard. Hormones are just the megaphone. Listen. Then act. Not with fear-with fire. You’ve survived 40+ years of life. You’ve got this.
There’s emerging data on gut-brain axis modulation via estrogen-metabolizing probiotics like Lactobacillus reuteri and Bifidobacterium longum. Phase 2 trials show fecal estrobolome diversity correlates with mood stability. Also, cortisol clearance is tied to microbial production of short-chain fatty acids. Not saying you need a microbiome test-but if you’re going to try supplements, go for spore-based probiotics, not random powders from Amazon.
I cried during a TED Talk about trees. That’s when I knew I needed help.
So you’re saying hormones make you emotional? Wow. What a shock. I thought it was just women being dramatic. Maybe if you stopped eating sugar and watched less TikTok you’d feel better. Also, antidepressants are for weak people. Just breathe and think positive thoughts. It’s all in your head. Literally.
hrt works but dont let ur dr push u into it like its a cure all. i tried it and got migraines. now i do yoga, cut caffeine, and just let it be. its not a disease its a phase. chill out. your body knows what to do
It is of paramount importance to underscore that the neuroendocrinological perturbations attendant upon the perimenopausal transition constitute a distinct physiological paradigm, not a psychopathological entity per se. The administration of exogenous estrogen, while empirically efficacious in certain cohorts, must be carefully weighed against the potential for thromboembolic risk, particularly in patients possessing a familial predisposition. Cognitive behavioral interventions, though adjunctive, remain indispensable in the cultivation of affective resilience.