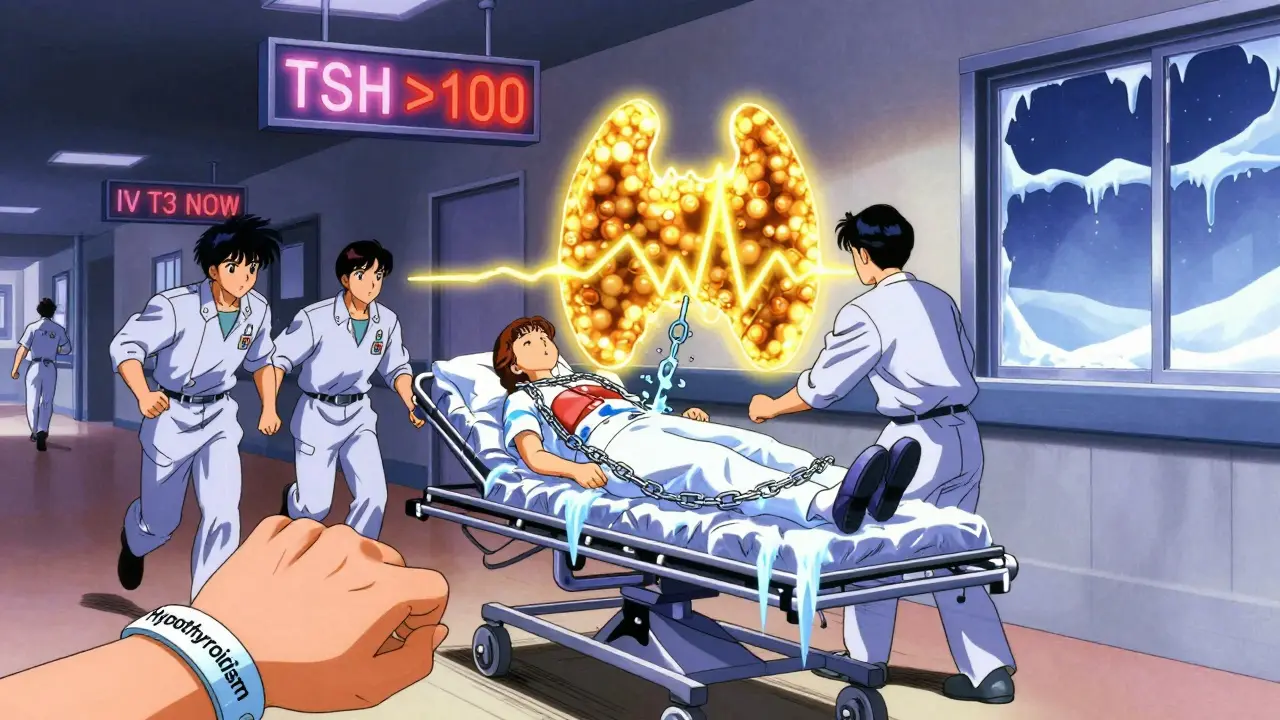
Myxedema coma isn’t just a rare complication of hypothyroidism-it’s a ticking time bomb. People with long-standing, untreated low thyroid function can slip into this life-threatening state without warning, often during winter or after an infection. And here’s the scary part: myxedema coma kills between 25% and 60% of those who develop it, even with modern care. The delay isn’t usually in treatment-it’s in recognition. Many patients are misdiagnosed for months with depression, dementia, or just "getting older." By the time they’re admitted to the ER, their body is shutting down: core temperature below 95°F, heart rate under 50, breathing so slow it’s barely there, and confusion that’s turned to unresponsiveness.
What Actually Happens in Myxedema Coma?
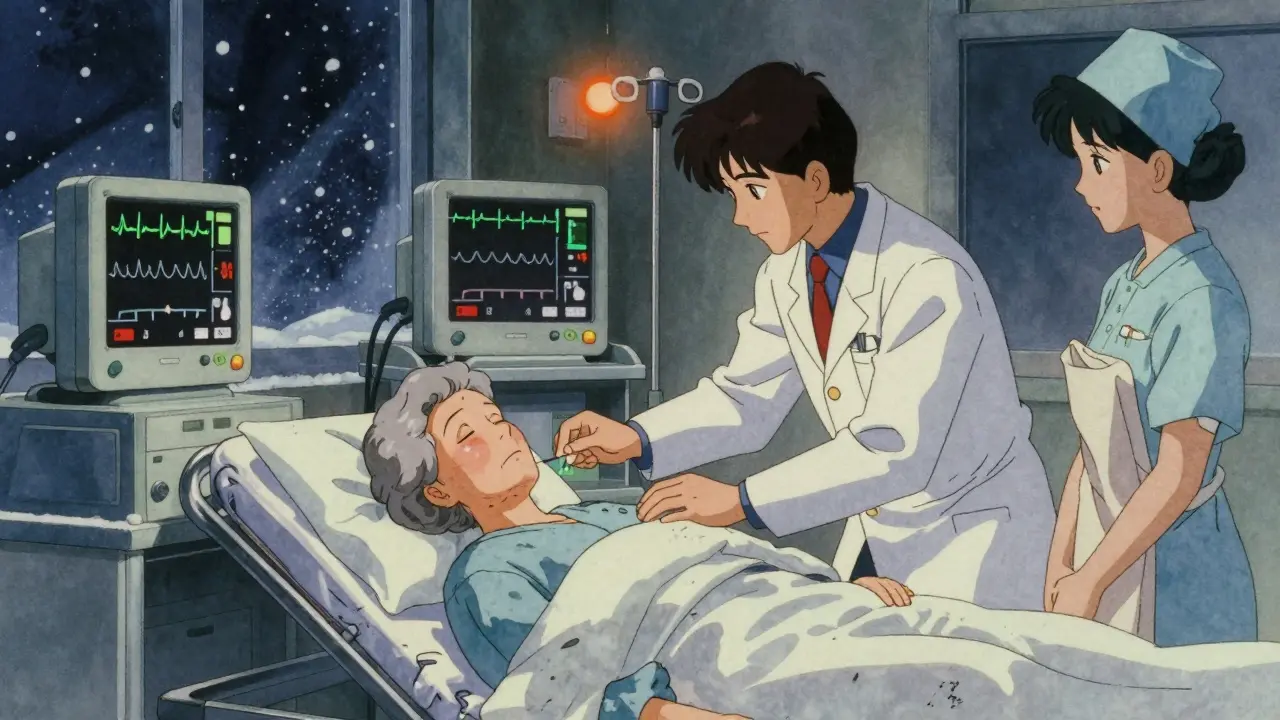
Your thyroid hormones-T3 and T4-run your metabolism like a furnace. When they drop too low, every system in your body slows down. Blood flow decreases. Your kidneys can’t filter properly. Your lungs stop responding to rising carbon dioxide levels. Your brain gets foggy, then numb. The classic signs aren’t subtle: extreme lethargy (seen in 98% of cases), dangerously low body temperature (80-90% of patients), and a clear trigger like pneumonia, a heart attack, or stopping thyroid meds during a hospital stay.But here’s what makes it dangerous: not everyone looks textbook. Elderly patients, especially women over 60, often don’t have puffy faces or dry skin. Instead, they might just seem "quiet," "sleepy," or "not themselves." A 70-year-old woman might be admitted for a UTI and quietly slip into coma because her thyroid levels were already borderline. Her doctors miss it because they’re looking for fever, not hypothermia. Or they think her slow heart rate is just aging.
Lab tests confirm it: TSH above 100 mIU/L (normal is 0.4-4.0), free T4 below 0.9 ng/dL, sodium under 135 mmol/L, and high CO2 in the blood. But waiting for those results can cost lives. Experts agree: if you suspect myxedema coma, start treatment before the labs come back.
How It’s Different From Other Endocrine Emergencies
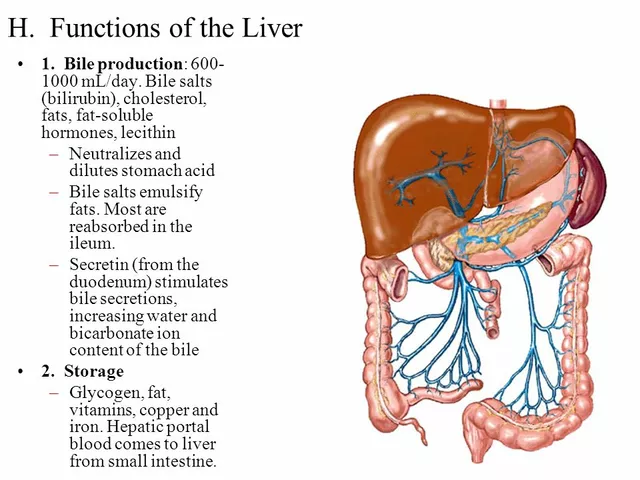
Thyroid storm is the hyperthyroid opposite-fast heart rate, high fever, agitation. Myxedema coma is the opposite: cold, slow, quiet. Diabetic ketoacidosis has clear numbers: high blood sugar, low pH, ketones in urine. Myxedema coma doesn’t. There’s no single test that says "yes, this is it." That’s why clinical judgment matters more than any lab value.Adrenal crisis can look similar-low blood pressure, confusion, nausea-but adrenal patients usually have skin darkening and vomiting. Myxedema coma patients have puffy eyelids, dry skin, and constipation so bad it leads to ileus or megacolon. The key difference? In adrenal crisis, you give steroids. In myxedema coma, you give thyroid hormone-immediately.
And mortality? Myxedema coma is deadlier than diabetic ketoacidosis (which kills 2-5%) and closer to adrenal crisis (15-25%). But unlike those, myxedema coma often has a slow build-up. Patients may have had untreated hypothyroidism for years. One patient on a thyroid support forum said she felt like she was "moving through molasses" for 18 months before collapsing. Her doctor called it depression.
Emergency Protocol: What to Do Right Now
There’s no time for hesitation. If you think myxedema coma, here’s what happens next:- Secure the airway. Half to 70% of patients need intubation because their breathing is too slow to keep oxygen up and CO2 down.
- Give IV thyroid hormone within 30 minutes. Start with 300-500 mcg of levothyroxine (T4). In severe cases-especially with heart problems-add 10-20 mcg of liothyronine (T3) every 8 hours. The 2022 Endocrine Society update says T3 should be first-line in cardiac compromise; it works faster.
- Warm gently. No heating blankets, no warm baths. Active rewarming can cause heart failure because the body can’t handle the increased metabolic demand yet. Use warm blankets, turn up the room, and monitor core temperature every 30 minutes.
- Treat the trigger. Infection is the cause in 30-50% of cases. Start broad-spectrum antibiotics right away-even if you’re not sure. Pneumonia and UTIs are the most common.
- Fix electrolytes slowly. Hyponatremia is common. But correcting sodium too fast can cause brain damage. Limit correction to 4-6 mmol/L in the first 24 hours.
The DIMES mnemonic helps remember triggers: Drugs (like sedatives or lithium), Infection, Myocardial infarction or stroke, Exposure to cold, Stroke. Check for all five.

Why Delay Is Deadly
Every hour you wait increases the chance of death by 10%. In one study, patients treated within 2 hours had a 30% lower mortality rate than those treated after 6 hours. But delays happen. Why?First, the symptoms are easy to miss. A 65-year-old man with confusion and low sodium? Maybe dementia. A woman with fatigue and constipation? Maybe menopause. Second, labs take time. Blood tests for TSH and T4 can take hours. Third, some clinicians still think you need coma to diagnose it. You don’t. The term "myxedema crisis" is now preferred because coma isn’t required.
One case from a UK hospital in 2023 involved a woman who stopped her levothyroxine during a hip surgery. She developed pneumonia, got confused, and was admitted. Staff thought she was delirious from pain meds. It took 10 hours before someone checked her thyroid levels. She spent 14 days in ICU. She survived-but barely.
Who’s at Risk?
Women over 60 make up 75% of cases. But men aren’t immune-they’re just diagnosed later. Healthline data shows men have a 40% longer delay in diagnosis, likely because doctors don’t expect hypothyroidism in them. Cold weather is a major trigger. Scandinavian countries report 50% more cases than Mediterranean ones. And it’s not just climate-it’s access to care.Uninsured patients wait 35% longer for treatment and have 22% higher death rates. In places where thyroid testing isn’t routine, undiagnosed hypothyroidism is common. The Global Burden of Disease Study predicts a 20% rise in myxedema coma cases by 2030, mostly because the elderly population is growing-and so is the number of people with untreated thyroid disease.
What’s New in Treatment?
The big shift? T3 is now recommended upfront in severe cases. For years, doctors used only T4 because it’s longer-lasting. But T4 takes days to convert to active T3 in the body. In crisis, you need speed. A 2022 multicenter trial showed using T3 with T4 cut 30-day mortality by 15%.In January 2023, the FDA approved a new IV thyroid hormone formulation called Thyrogen® with faster absorption. It’s not widely available yet, but it’s a step toward quicker, more reliable dosing.
Research is also moving toward early warning signs. A 2023 Lancet study found that elevated thyrotropin receptor antibodies predict decompensation in Hashimoto’s patients with 85% accuracy. Point-of-care thyroid tests are in phase 3 trials-they can give results in 15 minutes. Imagine an ER nurse running a quick finger-stick test and knowing within minutes if it’s myxedema coma.
What Patients Say
On support forums, survivors talk about the same things: feeling dismissed, being told it’s "just stress," or being labeled as "difficult" because their symptoms didn’t fit a mold. One man said, "I wore three layers inside my house in July because I was freezing. My doctor laughed and said I was just sensitive to air conditioning."Those who get treated fast often say they felt better within 24-48 hours. Their mental fog lifted. Their heart rate returned. Their temperature climbed. But those who waited? They spent weeks in rehab, had brain damage from low oxygen, or never fully recovered.
One woman shared: "I stopped my thyroid meds because I was in the hospital for pneumonia. No one checked them. When I woke up in ICU, I had no idea how I got there. My family said I hadn’t spoken for three days. I was 68. I thought I was just tired."
Prevention Is Possible
Most myxedema coma cases are preventable. If you have hypothyroidism:- Never stop your medication without talking to your doctor.
- Get your TSH checked every 6-12 months-even if you feel fine.
- Call your doctor immediately if you get sick, especially with infection, or if you feel unusually tired, cold, or confused.
- Keep a list of your meds and doses with you at all times.
- Wear a medical alert bracelet that says "Hypothyroidism" and lists your medication.
Hospitals in the U.S. are now required to have myxedema coma protocols in their ERs. But outside major centers, awareness is still uneven. If you’re a caregiver, know the signs. If you’re a clinician-don’t wait for the labs. If someone looks cold, slow, and confused with a history of thyroid disease-treat it like a heart attack. Time is brain. Time is life.
Can myxedema coma happen without a known thyroid history?
Yes. Up to 20% of cases occur in people who didn’t know they had hypothyroidism. Symptoms like fatigue, weight gain, or cold intolerance were mild or ignored. In older adults, especially, the signs can be hidden under other conditions like dementia or depression. That’s why unexplained hypothermia, bradycardia, or hyponatremia in an elderly patient should always prompt a thyroid test.
Is myxedema coma the same as myxedema crisis?
They’re the same condition, but "myxedema crisis" is the preferred term now. The word "coma" was dropped because patients don’t need to be unconscious to be in crisis. Many are just severely confused or lethargic. The key is the combination of hypothyroidism, hypothermia, and a triggering event-regardless of mental status.
Why can’t we just give more thyroid pills by mouth?
Because absorption is unreliable when the gut is shut down. Myxedema coma often causes ileus-no gut movement. Oral meds won’t be absorbed. Also, IV dosing gives precise control over hormone levels. Levothyroxine and liothyronine are available as IV formulations specifically for emergencies. Oral doses can be given later once the patient stabilizes.
Can steroids be given along with thyroid hormone?
Yes, if adrenal insufficiency is suspected. Severe hypothyroidism can mask adrenal problems. If the patient has low blood pressure that doesn’t improve with fluids or thyroid hormone, giving a low-dose IV hydrocortisone is recommended. It’s not routine, but it’s lifesaving if adrenal failure is present.
How long does recovery take after treatment?
Improvement can start within 24-48 hours of IV hormone replacement-mental clarity returns, temperature rises, heart rate normalizes. But full recovery can take weeks. Patients often need weeks of ICU care and months of rehab. Some have lasting cognitive issues if they went too long without oxygen. Lifelong thyroid replacement is always needed afterward.
Are there any home remedies or supplements that help?
No. Myxedema coma is a medical emergency requiring hospital care and IV hormones. Supplements like selenium or iodine won’t help and can be dangerous. Trying to treat it at home delays life-saving care. If you suspect this condition, call emergency services immediately.





OMG I JUST SAW THIS AND MY HEART STOPPED 😭 My grandma almost died from this and they thought she was just "being old"! She was freezing in July, wouldn't talk, and they gave her antidepressants for 6 months. When she finally got her TSH checked? 147. She spent 3 weeks in ICU. Please, if you know someone with thyroid issues-CHECK THE NUMBERS. It’s not just fatigue, it’s a silent killer.
THIS IS ALL A BIG PHARMA LIE. Thyroid problems? They’re caused by fluoride in the water and 5G radiation poisoning your pineal gland. I’ve been healing mine with raw garlic, Himalayan salt, and moonlight baths. No meds needed. The doctors won’t tell you this because they get paid per pill. Look up the 1950s thyroid studies-they were ALL suppressed. Wake up.
Wow. So we’re now treating a condition that’s been known since the 1800s like it’s some newfangled mystery? The fact that this is even a discussion is a testament to how lazy modern medicine has become. If you’re not checking TSH in elderly patients with unexplained lethargy, you’re not just negligent-you’re embarrassing. And yes, T3 upfront? Of course. T4 is a slow boat to nowhere in a crisis. I’m surprised this isn’t in every ER protocol by now.
Man I’ve seen this too many times. A friend’s mom went from "just tired" to coma in 48 hours. They didn’t check thyroid until she stopped breathing. Don’t wait for the textbook signs. If someone with known hypothyroidism looks off-cold, slow, quiet-treat it like a heart attack. No labs needed. Just give the hormone. Save the paperwork for later.
It’s wild how medicine still treats symptoms like puzzles instead of systems. The body isn’t a machine with isolated parts-it’s a slow-burning candle. When the flame gets too low, everything dims. Myxedema coma isn’t a thyroid problem-it’s a system-wide collapse. We treat it like a switch we flip, but really we’re just trying to relight a dying fire before it goes out forever. The real tragedy? Most of these people were one checkup away from never getting there.
Okay but can we talk about how the word "coma" is so dramatic? Like, I get it’s life-threatening but calling it "myxedema coma" sounds like a horror movie title. "Myxedema Crisis" is way more accurate-and less terrifying to patients who aren’t actually unconscious. Also, I’m 28 and have Hashimoto’s. I used to get told I was "just anxious." Now I wear a bracelet that says "Hypothyroidism-TSH 147 last time". Just in case.
Wait so you’re telling me my ex’s mom died because her doctor didn’t check her thyroid? She was in the hospital for a UTI for 5 days and they never ran a TSH? That’s not negligence, that’s criminal. I’m gonna start a petition to make thyroid panels mandatory for anyone over 50 admitted to the ER. No more "she’s just tired." No more "it’s menopause." No more dead people because someone didn’t look at a lab.
People who say "I feel fine" on thyroid meds are lying to themselves. If you’re not checking your TSH every 6 months, you’re playing Russian roulette with your brain. And don’t even get me started on those who stop meds because they "don’t like side effects." There are no side effects from taking your hormone replacement. Only death. And yes, I’ve seen it. And no, I won’t stop talking about it.
Hey everyone, I just want to say-this is why we need better education, not just for doctors, but for families. I’m a nurse, and I’ve had patients’ kids come in saying, "She’s just been lazy lately." But when you dig deeper, they’ve been cold, constipated, slow to respond for months. I always hand out these simple one-page guides to families: "Signs Your Loved One Might Be in Myxedema Crisis." It’s not complicated. It’s just not taught. Let’s change that.
Just read this after my aunt got diagnosed. She was in ICU for 11 days. She’s okay now, but her memory is still shaky. I’m telling everyone I know: if you have thyroid disease, get tested. If you’re caring for someone older, ask for a TSH. Don’t wait for them to collapse. It’s not dramatic. It’s not scary. It’s just common sense. And if you’re a doctor? Don’t wait for the labs. Just give the hormone.