Why Doctors Sometimes Prescribe Separate Pills Instead of One Combined Tablet
Imagine you’re on three different pills for high blood pressure. Each one is a different color, size, and shape. You have to remember which one to take in the morning, which one at night, and when to refill each. Now imagine a single tablet that does the same job-same ingredients, same effect, but just one pill. That’s a fixed-dose combination (FDC). But in many cases, doctors don’t prescribe that single tablet. Instead, they write separate prescriptions for each generic drug. This is called a de facto combination.
It sounds strange. Why would anyone choose three pills over one? The answer isn’t simple. It’s not about laziness or confusion. It’s about real clinical needs, cost differences, and gaps in the system. In the UK, US, India, and beyond, this practice is common-especially for chronic conditions like hypertension, diabetes, and HIV. But it comes with hidden risks that most patients never hear about.
What Exactly Is a De Facto Combination?
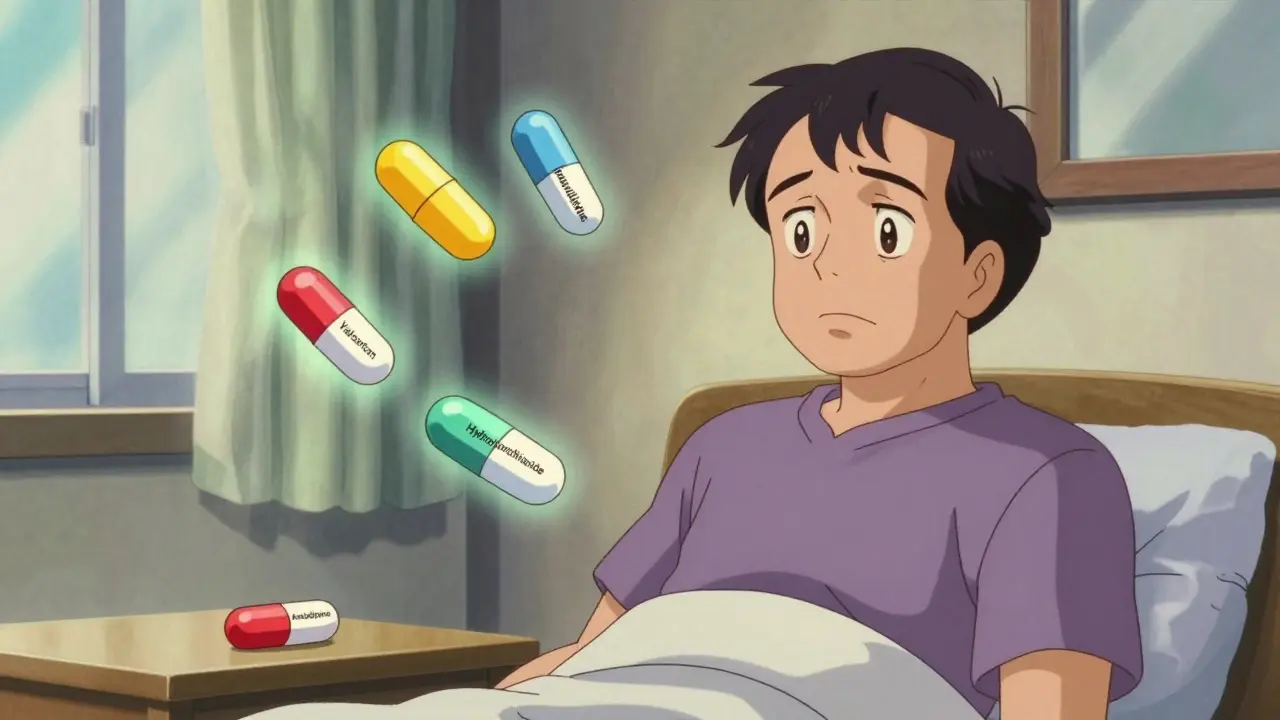
A de facto combination isn’t an approved drug. It’s not listed on any drug label. It’s just a clinical workaround. A patient takes two or more separate generic medications that, together, match the ingredients of an approved FDC. For example: instead of taking a single tablet with amlodipine and valsartan, a doctor prescribes a 5mg amlodipine pill and a 160mg valsartan pill-two separate pills, bought separately.
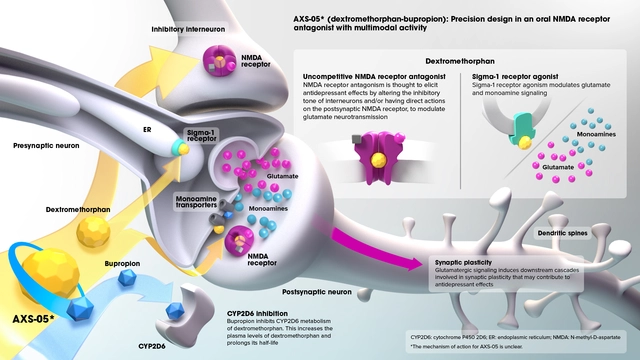
This happens because FDCs are made in fixed ratios. If a patient needs 10mg of drug A and 40mg of drug B, but the only available FDC is 5mg/80mg, the doctor can’t use it. So they reach for the generics. The result? The same therapeutic effect, but with no regulatory oversight. No safety studies. No bioequivalence checks. No testing to see if the two drugs interact in this exact combination.
The European Medicines Agency (EMA) says FDCs must prove that the combination is safer or more effective than taking the drugs alone. De facto combinations? They skip that step entirely. That’s not a loophole-it’s a blind spot.
Why Do People Choose Separate Generics?
There are three big reasons: flexibility, cost, and availability.
Flexibility is the strongest argument. Patients with kidney disease, liver problems, or changing conditions often need precise dosing. A diabetic with declining kidney function might need 500mg of metformin and 25mg of sitagliptin. But the only FDC available is 1000mg/50mg. That’s too much. So the doctor splits the doses. That’s not guesswork-it’s science. The American Diabetes Association found that nearly 70% of type 2 diabetes patients need individualized dosing that FDCs can’t provide.
Cost is another driver. In some places, the combined cost of two generic pills is lower than the branded FDC. In India, a 2012 parliamentary report found many FDCs offered no real benefit over separate drugs-and were often more expensive. In the US, a 2022 study showed that for certain hypertension combinations, separate generics were 15-20% cheaper than the FDC version. For patients paying out of pocket, that matters.
Availability is the third. Not every FDC is approved everywhere. In the EU, regulators are strict about what combinations get approved. In India, over 300 FDCs were banned in 2016 for lacking evidence. That pushed doctors toward separate generics-even when an FDC might have been better.
The Hidden Cost: Adherence and Mistakes
Here’s the problem no one talks about enough: people forget pills.
Every extra pill in a regimen cuts adherence by about 16%, according to a study in PubMed. That means if you’re on three pills instead of one, you’re 48% more likely to miss a dose. In a 2022 analysis of 1,247 patients on PatientsLikeMe, 63% of those on separate generics said they struggled to remember which pill was which. Only 31% of those on FDCs said the same.
One Reddit user wrote: “My doctor switched me from a single Amlodipine/Benazepril pill to two separate ones to save $15 a month. I missed two doses last month because I forgot which blue pill was which.”
It’s not just memory. Pharmacists see errors all the time. A 2022 survey of 1,532 US pharmacists found 72% worried about medication mix-ups with de facto combinations. A patient might grab the wrong generic because the pill looks similar to another. Or refill one but not the other. Or take both at the same time by accident.
These aren’t hypothetical risks. The FDA issued a safety warning in January 2023 after 147 adverse events were linked to untested combinations. Some patients ended up in the ER because they took too much of one drug, or because the two generics didn’t play well together.

When De Facto Combinations Make Sense
Let’s be clear: this isn’t always a bad idea.
For patients on dialysis, or those with severe liver impairment, or those titrating doses slowly, separate generics are the only safe option. A 5-star Drugs.com review from a diabetic patient said: “I’m on separate Metformin and Sitagliptin because the FDC dose was too strong for my kidneys. My A1c has been at 6.2% for 18 months.”
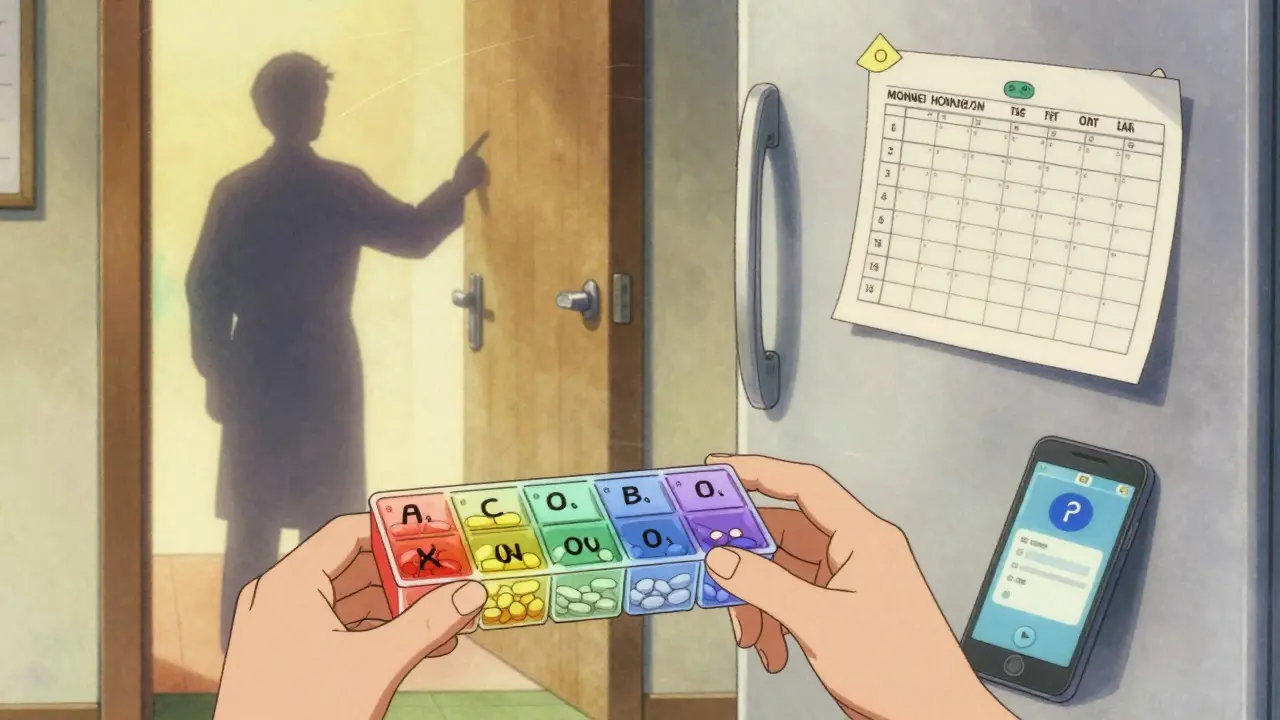
Doctors who use de facto combinations wisely know the rules. They pick generics with similar release profiles. They avoid combinations with known interactions. They give patients written schedules. Some even use color-coded pill boxes.
A physician on Student Doctor Network shared: “I prescribe separate generics for HIV patients who need dose tweaks. But I always give them a printed schedule. It adds work, but it prevents errors.”
For these patients, the flexibility outweighs the risk. But that’s the key: it’s intentional, not accidental.
What’s Missing: Support Systems
Most patients on de facto combinations get no extra help. No counseling. No pill organizers. No automated refill reminders. That’s a system failure.
Compare that to FDC users. They often get adherence programs built in-blister packs, mobile app alerts, pharmacy follow-ups. But the patient on three separate pills? They’re on their own.
Some organizations are stepping in. PillPack by Amazon launched a “Combination Therapy Support Program” in 2021. It pre-sorts pills by time of day, sends reminders, and includes counseling. Patients using it saw a 41% drop in missed doses.
But that’s not standard. It’s a luxury. Most patients don’t have access to it.
And here’s the irony: FDCs were created to reduce complexity. But when we abandon them for separate generics without support, we make things worse.
The Future: Better FDCs, Not More Pills
Pharma companies are starting to listen. AstraZeneca filed a patent in 2022 for a “modular FDC”-a tablet that lets you adjust the dose of one component without changing the other. It’s like a Lego version of a combination pill.
AI is also helping. Delta4 AI used machine learning to identify new, safe combinations for rare kidney diseases. The goal? To replace guesswork with data.
Regulators are watching too. The EMA is running a 2023-2025 project to study off-label combinations. The FDA’s 2021 guidance says any combination-whether in one pill or two-needs evidence of benefit.
And the WHO added new guidance in 2023: “Separate components may be preferable to fixed combinations… but only when justified by clinical need.”
This isn’t about banning de facto combinations. It’s about making them intentional, safe, and supported.
What Patients Should Do
If you’re on separate generics that make up a combination:
- Ask your doctor: “Is this the best option for me, or is there an FDC that could work?”
- Request a printed schedule with pill colors, times, and doses.
- Use a pill organizer with compartments for morning, afternoon, evening.
- Set phone reminders for each pill-don’t assume you’ll remember.
- Ask your pharmacist: “Are these generics bioequivalent to the ones studied in the FDC?”
- Report any side effects-even small ones. They might be from an interaction.
If your doctor refuses to consider an FDC, ask why. Is it cost? Dose flexibility? Availability? Know the reason so you can make an informed choice.
What Providers Should Do
Doctors and pharmacists need to stop treating de facto combinations as routine. They’re not. They’re high-risk interventions.
- Document the clinical reason clearly: “Patient requires 7.5mg amlodipine; no FDC available at this dose.”
- Use electronic prescribing systems that flag potential interactions between separate generics.
- Offer pill organizers or refer patients to services like PillPack.
- Reassess every 3-6 months. Is the separate regimen still necessary? Or can an FDC be tried now?
- Don’t default to separate generics just because they’re cheaper. The long-term cost of missed doses and ER visits is higher.
Training matters. A 2021 study found physicians who got special training on combination therapy were 37% less likely to prescribe inappropriate de facto combinations.
This isn’t about blaming doctors. It’s about giving them better tools.
Final Thought: One Pill Is Easier. But Only If It’s Right.
De facto combinations aren’t evil. They’re a symptom of a system that doesn’t always offer the right tools. FDCs are great for adherence. But they’re useless if they don’t match the patient’s needs.
The goal isn’t to eliminate separate generics. It’s to make sure they’re used only when necessary-and that patients get the support they need to stay safe.
Because in the end, it’s not about how many pills you take. It’s about whether you take them right.






I’ve been on three separate blood pressure pills for two years now, and honestly? I forgot one last week and ended up dizzy at work. I didn’t even realize I missed it until my head started spinning. I wish my doctor had mentioned the adherence stats-no one told me each extra pill cuts my chances of taking them right by 16%. I’m switching to a pill organizer tomorrow. And yes, I’m asking about an FDC next visit. This post? Lifesaver.
In India, we use separate generics because FDCs are either banned or overpriced 🤷♂️. My uncle takes amlodipine + atenolol separately-costs half of the combo pill. But yeah, he uses a color-coded box. No one teaches us this stuff. Pharma companies don’t care if we survive-they care if we buy their branded combo. 🤨💊
i just started on separate pills last month and honestly i have no clue what any of them do. my doc just handed me a bag with three different colors and said 'take these'. i think one is blue and one is white and the other is kinda green? i use my phone to remind me but sometimes i still mix them up 😅
As someone who’s lived with diabetes for 18 years, I’ve seen the evolution of these combos. I used to take three pills-now I’m on a single FDC. The difference in my A1c? 7.8% down to 6.3%. But here’s the truth: it only worked because my doctor took the time to match my kidney function. That’s what matters-not the number of pills, but the precision. We need more doctors who think like scientists, not cost-cutters. And patients? We need better education. This isn’t just medical-it’s human.
I’m so glad someone finally wrote about this. I’ve been quietly terrified of my own meds for months. I take metformin, sitagliptin, and a statin-all separate. I’m terrified I’ll accidentally take two of the same pill. I bought a pill sorter, but I still feel guilty every time I forget. I wish there was a system that helped people like me… not just the ones who can afford PillPack. Why is adherence support a luxury? It should be standard.
It is an egregious failure of the medical-industrial complex to allow this practice to persist without mandatory adherence protocols. The FDA’s silence on untested combinations is not oversight-it is negligence. Patients are being used as unwitting test subjects. This is not ‘flexibility’-it is systemic abandonment masked as clinical autonomy. The EMA has standards. The WHO has guidelines. Yet here we are, in the United States, where profit dictates pharmacology and patients pay with their health. I demand accountability.
bro in india we do this because its cheaper and doctors dont have time to explain fdc. i use a small notebook to write down what pill to take when. simple. no fancy apps needed. just write it down. my dad does it too. we live, we survive. no drama.
One pill is easier. But only if it fits.