When you pick up a generic pharmacy practice, the system that ensures affordable, FDA-approved medications are dispensed safely and consistently. Also known as generic drug dispensing, it’s how most people in the U.S. get their prescriptions today—without paying brand-name prices. It sounds simple: same drug, lower cost. But behind that simple swap are strict rules, hidden risks, and real-world checks that keep you safe.
At the heart of every generic drug, a medication legally approved to work the same as a brand-name version. Also known as bioequivalent medication, it must pass the same tests for strength, purity, and how fast your body absorbs it. The FDA oversight, the federal system that inspects drug factories, reviews data, and enforces quality standards. Also known as pharmaceutical regulation, it doesn’t just look at pills on a shelf—it sends inspectors to factories in India, China, and beyond to check if the raw materials and processes meet CGMP standards. You might think all generics are the same, but that’s not true. Some batches fail. Some manufacturers cut corners. That’s why the FDA now does unannounced visits to over 80% of foreign plants making drugs for Americans.
Then there’s pharmacy safety, the day-to-day actions pharmacists take to prevent mistakes in filling, labeling, and advising on medications. Also known as medication safety protocols, it’s not just about giving the right pill—it’s about checking for interactions, confirming dosages, and spotting when a patient’s new generic might not work like the old one. Think levothyroxine: even tiny changes in absorption can throw your thyroid levels off. Or antibiotics like doxycycline: if an antacid is taken too close, the drug becomes useless. These aren’t edge cases—they’re common risks in everyday pharmacy practice.
What you won’t see on the bottle? The stability testing. The batch-to-batch consistency checks. The dual verification steps in compounding pharmacies. Or how patent laws in the U.S. delay generic entry longer than in Canada or the EU. These are the invisible layers that make generic pharmacy practices work—or fail.
Some people assume generics are cheaper because they’re lower quality. That’s a myth. Most are identical. But some aren’t. That’s why knowing what to ask—about bioequivalence, manufacturer changes, or side effect shifts—is your best defense. The posts below dig into real cases: how a switch to a different generic caused panic in thyroid patients, why foreign manufacturing inspections are tightening, how stability testing proves a pill won’t break down in your medicine cabinet, and when you should push back if your new generic doesn’t feel right.
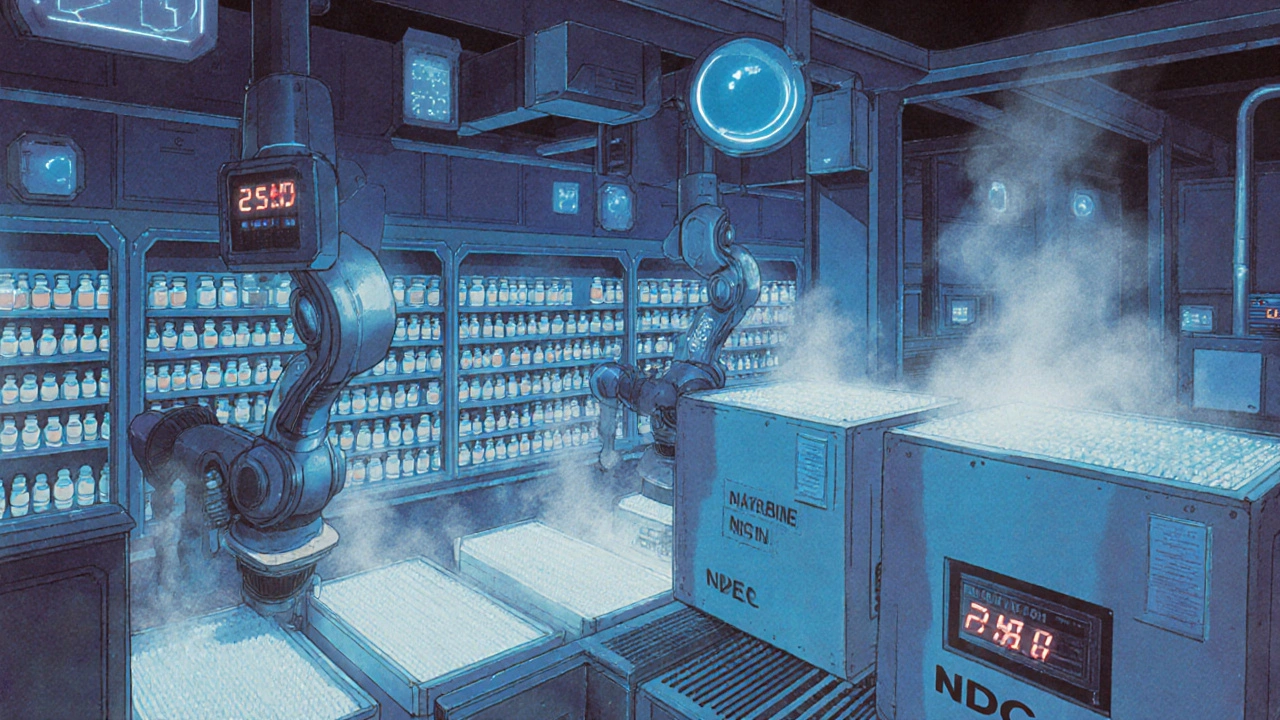
Mail-order pharmacies dispense 90% generic drugs with strict quality controls. Learn how temperature tracking, batch testing, and double verification ensure your meds are safe-even when shipped across the country.
