Every pill you take should work the way it’s supposed to. But what if it doesn’t? What if the active ingredient is missing, diluted, or replaced with something dangerous? This isn’t science fiction. It’s a real threat - and it’s why generic drug quality control isn’t just paperwork. It’s the last line of defense against counterfeit medicines that can kill.
Why Generic Drugs Need Tighter Controls Than You Think
People often assume brand-name drugs are safer than generics. That’s a myth. The FDA requires generic drugs to meet the exact same standards as brand-name drugs. Same active ingredient. Same dosage. Same performance. But here’s the catch: generics make up 90% of all prescriptions in the U.S. by volume. That means if quality control fails, millions of people are at risk - not just a few. Counterfeiters don’t target expensive brand-name drugs as often. They go for high-volume, low-cost generics. Why? Because they’re easier to replicate, easier to distribute, and harder for patients to notice if something’s wrong. A fake pill might look identical. It might even contain the right chemical. But if the crystal structure is off, or the binding agent is wrong, the drug won’t dissolve properly. Your body never absorbs it. The infection doesn’t go away. The blood pressure stays high. You think the medicine isn’t working - when it’s the fake that’s failing you.The Foundation: cGMP and the ‘Built-In’ Safety Model
The system that keeps most generic drugs safe is called current Good Manufacturing Practices, or cGMP. It’s not optional. It’s the law. And it’s built on one core idea: quality can’t be tested into a product - it has to be built in from the start. That means every step of manufacturing is controlled - from the moment raw materials arrive to the final package leaving the plant. It’s not enough to test a few pills at the end. You need to monitor temperature, humidity, mixing time, equipment cleanliness, and even the air quality in the room where the drug is made. The FDA requires clean rooms to meet ISO Class 5 standards - meaning no more than 3,520 particles per cubic meter larger than 0.5 microns. That’s stricter than most hospital operating rooms. And here’s the key: every batch must be tracked. Every ingredient must be verified. Every machine must be calibrated. If a single step fails, the whole batch is rejected. No exceptions. This isn’t about perfection. It’s about predictability. If you control every variable, you eliminate the chaos that counterfeiters rely on.The SQUIPP Framework: What ‘Quality’ Actually Means
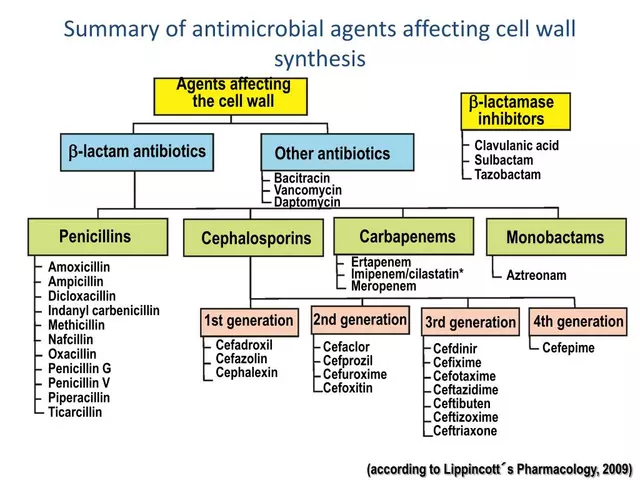
Pharmaceutical manufacturers don’t just say “it’s safe.” They prove it using a framework called SQUIPP: Safety, Quality, Uniformity, Identity, Potency, and Purity. Each letter represents a non-negotiable test.- Identity: Is this the right drug? Infrared spectroscopy and high-performance liquid chromatography (HPLC) confirm the chemical fingerprint matches the original. Accuracy? Better than 99.9%.
- Potency: Does it contain the right amount of active ingredient? Too little? Ineffective. Too much? Dangerous. The FDA requires results within 95-105% of the target.
- Dissolution: Will your body absorb it? A pill must release at least 80% of its drug within 30-45 minutes under simulated stomach conditions. If it doesn’t, it’s thrown out.
- Purity: Are there harmful impurities? Even trace amounts of toxic byproducts - like the ones found in the 2018 valsartan recall - trigger batch recalls.
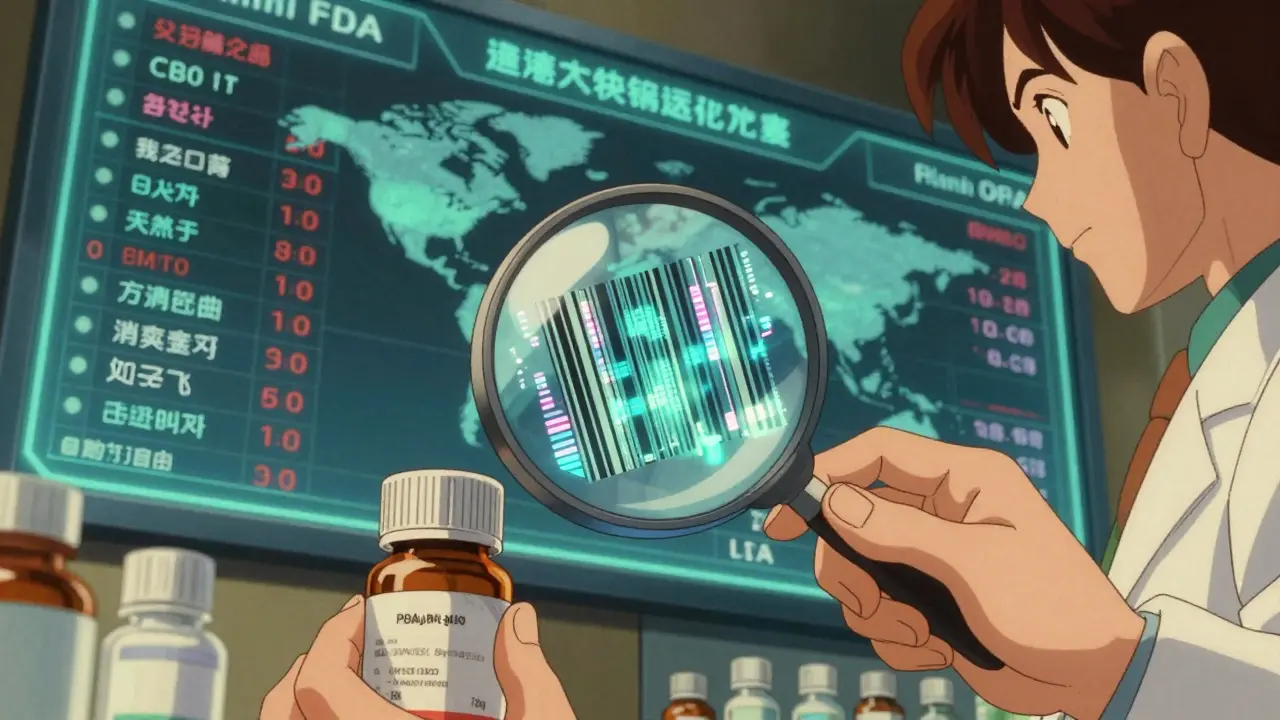
Track-and-Trace: The Digital Shield Against Fakes
In 2023, the U.S. Drug Supply Chain Security Act made it law: every prescription drug package must have a unique digital code. Think of it like a license plate for your medicine. Scanned at the pharmacy, the warehouse, even the hospital. If the code doesn’t match the FDA’s database, the drug is blocked. This system - called serialization - has cut counterfeit entries by over 90% in markets where it’s fully implemented. The code isn’t just a barcode. It’s encrypted, tamper-proof, and linked to the batch, expiration date, and manufacturing location. Counterfeiters can copy the label. They can’t copy the digital fingerprint. Big manufacturers like Teva and Sandoz use cloud-based Quality Management Systems (eQMS) that tie every test result, every machine log, and every shipment into one real-time dashboard. One quality manager at a major generic maker told a Reddit forum: “Our eQMS cut our deviation resolution time from two weeks to under two days.” That speed matters. The faster you catch a problem, the fewer fake pills reach patients.Where the System Still Has Gaps
The system works - but it’s not perfect. The biggest blind spot? Polymorphs. Some drugs can exist in different crystal forms. One form works. Another doesn’t. Standard tests can’t always tell the difference. That’s how the valsartan recall happened: a chemical impurity formed during a slight change in manufacturing that wasn’t caught because the test didn’t look for it. Also, not every factory follows the rules. FDA inspections show 94% compliance in U.S. plants. But in India, it drops to 78%. In China, it’s 65%. That’s why the WHO estimates 1% of medicines in developed countries are fake - but up to 30% in low-income regions. Smaller manufacturers struggle with cost. A single near-infrared spectrometer - used to verify identity - costs $500,000 to $1 million. Many can’t afford it. That’s why the FDA and WHO are pushing for shared testing labs and AI-powered tools that can analyze data faster and cheaper.
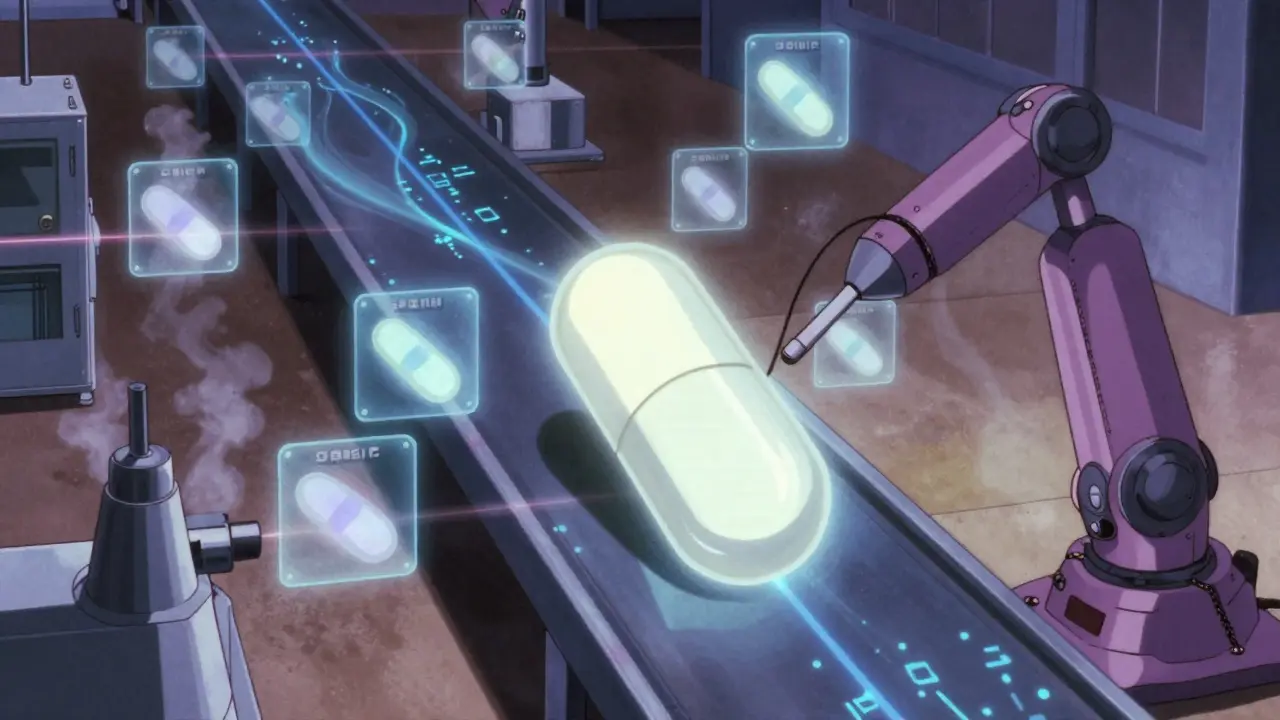
What’s Next? AI, Blockchain, and Molecular Tags
The future of counterfeit prevention isn’t just better tests. It’s smarter systems. By 2025, the FDA expects all manufacturers to use continuous manufacturing - where the drug is made in one flowing process, not in batches. Sensors check quality every five seconds. If something’s off, the line stops before a single bad pill is made. In Africa, the WHO is testing blockchain for antimalarial generics. Each dose is recorded on a public ledger. Patients can scan a code and see the full history: where it was made, when it passed inspection, where it traveled. No one can alter it. Even more advanced? Molecular taggants - invisible chemicals added to the drug that can be detected with a smartphone app. These tags are unique to each manufacturer. No one can replicate them without access to the formula. Pilot programs are already underway.What You Can Do
As a patient, you don’t need to understand chromatography or serialization. But you can protect yourself:- Buy from licensed pharmacies - not random websites.
- Check your pills. If they look different from last time, ask your pharmacist.
- Use the FDA’s Drugs@FDA database to verify your medication’s details.
- Report suspicious products. The FDA takes every report seriously.
Why This Matters Beyond Pills
This isn’t just about drugs. It’s about trust. When you take a generic, you’re trusting the system to keep you safe. That trust isn’t given. It’s earned - through thousands of inspections, millions of data points, and billions of dollars invested in keeping fakes out. The $200 billion in counterfeit drug sales prevented each year? That’s not a number. That’s millions of people who didn’t get sicker. Who didn’t die. Who kept living because the system worked. The goal isn’t perfection. It’s resilience. And right now, that’s exactly what generic drug quality control delivers.Are generic drugs as safe as brand-name drugs?
Yes - if they’re made under proper quality control. The FDA requires generics to have the same active ingredient, strength, dosage form, and performance as the brand-name version. Studies show the adverse event rate for FDA-approved generics is actually slightly lower than for brand-name drugs (0.02% vs. 0.03%). The difference isn’t in the drug - it’s in whether the manufacturer follows cGMP standards.
How can I tell if my generic drug is fake?
You can’t always tell by looking. Fake pills often look identical. But if your pill looks different from previous refills - different color, shape, or imprint - ask your pharmacist. Check the packaging for spelling errors, missing barcodes, or poor print quality. Buy only from licensed pharmacies. Use the FDA’s Drugs@FDA website to verify your drug’s details. If something feels off, report it.
Why are counterfeit drugs more common in some countries?
Countries with weak regulatory systems, limited inspections, and poor supply chain tracking are more vulnerable. The WHO estimates counterfeit rates of 10-30% in some low-income regions, compared to under 1% in the U.S. and EU. This isn’t about culture - it’s about resources. Without mandatory serialization, real-time testing, and trained inspectors, fake drugs slip through.
Do all generic manufacturers follow the same rules?
Legally, yes - all must meet FDA or WHO cGMP standards. But compliance varies. U.S. facilities have a 94% compliance rate. In India, it’s 78%. In China, it’s 65%. The FDA inspects foreign plants less often than U.S. ones, and some smaller manufacturers lack the budget for advanced testing equipment. That’s why international collaboration and audits are critical.
Can AI really help stop counterfeit drugs?
Yes - and it already is. AI tools analyze thousands of test results to spot patterns humans miss. They can detect subtle changes in chemical composition or manufacturing deviations before a batch is released. IBM and Siemens have invested over $1.2 billion in AI for pharmaceutical quality control. By 2027, AI is expected to reduce counterfeit incidence by 40%. It’s not a magic fix - but it’s a powerful tool.
Is it safe to buy generic drugs online?
Only if the website is verified. The FDA warns that 96% of online pharmacies selling drugs without a prescription are illegal. Many sell counterfeit or substandard products. Use only pharmacies with the VIPPS seal (Verified Internet Pharmacy Practice Sites). Never buy from sites that don’t require a prescription or offer “miracle” discounts. Your health isn’t worth the risk.






Quality control in pharma isn't glamorous but it's the reason your blood pressure med actually works
no drama no fanfare just science doing its job
Let’s be honest the entire cGMP framework is a performative ritual designed to satisfy regulatory vanity
the real truth lies in the unmeasured variables the unmonitored humidity shifts the silent polymorphic transitions
we’re not safeguarding health we’re maintaining bureaucratic equilibrium
The system works because it’s layered not because it’s perfect
each layer reduces risk
that’s all we need
AI will never replace human judgment in quality control
it can flag anomalies but only a trained mind knows what’s meaningful
It’s easy to admire the infrastructure-the clean rooms the serialization the AI-driven analytics-but what’s harder to see is the quiet discipline of the technicians who never get thanked
the ones who notice a 0.03% variance in dissolution rates at 3 a.m.
the ones who reject a batch because the tablet’s surface has a microscopic crack no one else would catch
the system works because people care enough to stop the line even when no one is watching
we treat medicine like a commodity but it’s not-it’s the last thing standing between a person and the dark
and every time a machine flags a deviation or a human says no that’s not just compliance that’s dignity
They say the FDA inspects foreign plants less often-yeah well that’s because they’re too busy protecting their own industry
China and India make 80% of our generics and they’re cutting corners
we’re letting foreign labs run our medicine while we sit here with our iPhones and our trust fund babies
this isn’t science it’s surrender
what if the whole system is rigged like the vaccines
what if they just make the pills look right but the real stuff is somewhere else
they control the database right
so even if you scan the code it just says legit
they could be feeding us sugar pills and we’d never know
they’ve got the tech to fake everything
Love that they’re using blockchain in Africa for antimalarials 😊
imagine if every person could trace their medicine back to the lab
that’s justice in action
no more guessing no more fear
just truth in a scan
we need this everywhere 🌍❤️
It’s beautiful how Canada and the U.S. share standards-it’s not just about drugs it’s about mutual care
we’re not just trading pills we’re trading responsibility
and that’s something worth protecting
The fact that generics have a slightly lower adverse event rate than brand-name drugs is a powerful rebuttal to the myth that they’re inferior
the data doesn’t lie
the difference isn’t in the molecule-it’s in the manufacturing discipline
and that discipline is what we must protect
my pharmacist just told me my generic lisinopril looks different this time
so i checked Drugs@FDA and sure enough the imprint changed
they didn’t tell me but i asked
turns out it’s the same drug just a new maker
never assume
always check
your body remembers
The polymorph issue is the quiet crisis no one talks about
the same molecule can exist in multiple crystalline forms and only one of them delivers the therapeutic effect
standard HPLC can’t distinguish them
the difference is in the lattice structure
and it’s not just valsartan-there are at least a dozen other drugs where this has been documented in peer-reviewed literature but never made public
the FDA’s current testing protocols simply aren’t designed to catch this
we’re relying on a 1970s-era analytical framework to detect 21st-century molecular subtleties
until we invest in single-crystal X-ray diffraction as a routine screening tool we’re playing Russian roulette with millions of prescriptions
just had my dad on generic metformin for 12 years and he’s still kicking
no drama no side effects
the system works
trust the process
and if your pill looks weird ask your pharmacist
they got your back