When you’re in constant pain, falling asleep feels impossible. And when you finally do drift off, you wake up exhausted, sore, and in even more pain. It’s not just bad luck-it’s a cycle. A real, biological loop where pain keeps you awake, and lack of sleep makes the pain worse. This isn’t something you can just power through. It’s not laziness. It’s not "being dramatic." It’s neuroscience.
The Cycle You’re Trapped In
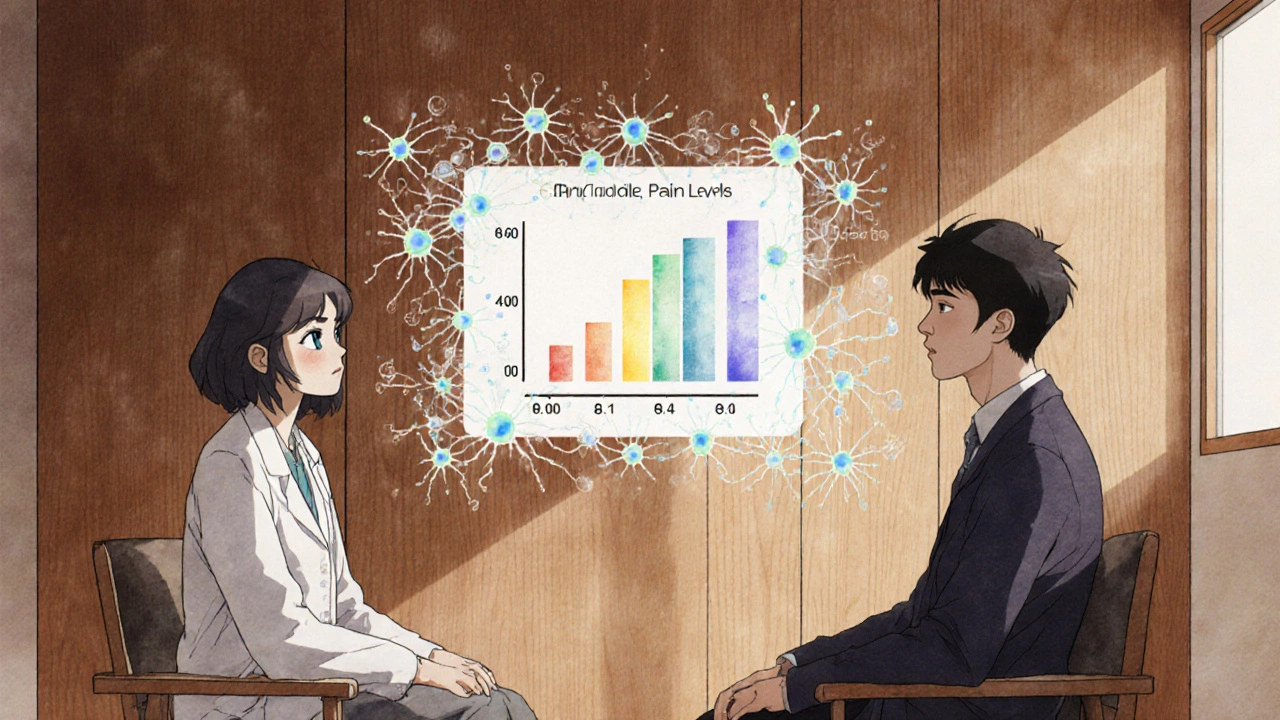
Chronic pain doesn’t just make it hard to sleep-it rewires your brain to feel more pain when you’re tired. Studies show that people with chronic pain who also struggle with sleep report pain levels that are 35-45% higher than those who sleep well. That’s not a small difference. That’s going from a manageable 4 out of 10 to an unbearable 8 out of 10. And it’s not just the intensity. Pain lasts longer. Recovery takes weeks instead of days.
Meanwhile, your body is working against you. When you don’t sleep enough, your brain’s natural painkillers-like endogenous opioids-drop by 30-40%. At the same time, your immune system ramps up inflammation, spiking cytokines like IL-6 by 25-35%. These chemicals don’t just make you feel sick-they make your nerves hypersensitive. You start feeling pain from things that never hurt before. A light touch. A breeze. The weight of a blanket.
And here’s the kicker: even if you don’t have chronic pain yet, poor sleep raises your risk of developing it by 56% over five years. That’s not a guess. That’s data from the NIH. Sleep isn’t just a side effect of pain. It’s a trigger.
What’s Actually Happening in Your Brain
It’s not just "my back hurts so I can’t sleep." There’s a system in your brain that acts like a thermostat for pain. When you’re sleep-deprived, that thermostat gets stuck on high. Researchers at Massachusetts General Hospital compared it to a broken heater that keeps turning up the heat even when the room is already boiling.
One key player is dopamine. This chemical helps you feel motivated, focused, and yes-even less pain. But after a night of broken sleep, dopamine levels drop by 20-30%. That’s why you feel flat, unmotivated, and more sensitive to discomfort. It’s not in your head. It’s in your chemistry.
Then there’s the kappa opioid receptor. This little-known system in your brain helps regulate both pain and sleep. When it’s not working right, you get stuck in a loop: pain keeps you awake, and sleep loss makes your pain receptors scream louder. New drugs targeting this receptor are showing 40-60% improvement in sleep quality in early trials. But you don’t have to wait for a new pill to start breaking the cycle.
Why Over-the-Counter Sleep Aids Don’t Work (and Often Make It Worse)
72% of people with chronic pain try melatonin, antihistamines, or OTC sleep aids. Only 35% say they help. And 42% say they feel groggy the next day-worse than before they took them.
Why? Because these pills don’t fix the root problem. They just sedate you. They don’t restore healthy sleep architecture. They don’t reduce inflammation. They don’t reset your brain’s pain thermostat. And if you wake up foggy, your body can’t recover properly. That grogginess? It’s another stressor that spikes cortisol and makes your pain worse.
One patient in Manchester, Sarah M., described it perfectly: "After four nights of bad sleep from my back pain, my fibromyalgia flares go from a 4/10 to an 8/10. It takes me two weeks to recover-even after I finally sleep." She didn’t need more pills. She needed a new system.
The Only Treatment That Actually Breaks the Cycle
There’s one intervention proven to work better than any drug: Cognitive Behavioral Therapy for Insomnia (CBT-I).
It’s not a sleep app. Not a supplement. Not a fancy mattress. It’s a structured, evidence-based program that retrains your brain and body to sleep again-even with pain.
Studies show CBT-I reduces insomnia symptoms in 65-75% of chronic pain patients. And here’s the game-changer: it also reduces pain intensity by 30-40%. That’s not a side effect. It’s the point.
How? CBT-I works in four key ways:
- Stimulus control: You only go to bed when sleepy. No lying in bed watching the clock. Your bed becomes a sleep-only zone.
- Sleep restriction: You limit time in bed to match actual sleep time. This builds sleep pressure so you fall asleep faster and stay asleep longer.
- Cognitive restructuring: You challenge thoughts like "I’ll never sleep" or "If I don’t sleep, my pain will kill me." These thoughts keep your nervous system on high alert.
- Sleep hygiene: You adjust light, temperature, caffeine, and bedtime routines-not just to help sleep, but to reduce pain triggers.
It takes 8-10 weekly sessions. But the results last. Unlike pills, CBT-I doesn’t wear off. You learn skills that keep working for years.
What to Track (and Why)
If you’re serious about breaking the cycle, you need data. Not guesses. Data.
Start a simple sleep diary for two weeks. Write down:
- Time you got into bed
- Time you actually fell asleep
- Number of times you woke up
- How long you were awake after each wake-up
- Total hours slept
- Pain level on a scale of 1-10 when you woke up
- How rested you felt
Then use the Insomnia Severity Index (ISI). It’s a free, 7-question tool. Score above 15? You have clinically significant insomnia. That’s your green light to seek help.
Don’t wait for your doctor to ask. Bring this diary to your next appointment. Say: "I think my sleep is making my pain worse. I want to try CBT-I."
What to Look for in a Provider
Not all pain clinics treat sleep. And not all sleep clinics understand chronic pain.
Look for providers who:
- Use CBT-I as a first-line treatment, not a last resort
- Have a sleep specialist and pain specialist working together
- Don’t push opioids or sedatives as the main solution
- Ask about your sleep habits before adjusting your pain meds
Patients who get integrated care report satisfaction ratings of 4.7/5. Those who get pain-only treatment? 3.2/5. The difference? Sleep.
Real Progress, Not Quick Fixes
You can’t sleep your way out of chronic pain overnight. But you can break the cycle. One night at a time.
Start small. Get up at the same time every day-even if you slept badly. Get sunlight within 30 minutes of waking. Avoid caffeine after 2 p.m. Make your bedroom cool, dark, and quiet. Use your bed only for sleep and sex. No scrolling. No TV. No worrying.
And when pain flares? Don’t fight it. Don’t lie there angry. Get up. Go to another room. Do something quiet. Read under dim light. Stretch gently. Come back when you feel sleepy.
This isn’t about forcing sleep. It’s about creating the conditions where sleep can return-naturally, safely, and without pain controlling the outcome.
And if you’re tired of being told to "just relax" or "take something"-you’re right to be frustrated. The answer isn’t in a bottle. It’s in your rhythm. Your habits. Your brain. And you can retrain it.
What’s Next for Treatment
Scientists are working on drugs that target the kappa opioid receptor. Gene studies are identifying who’s most likely to respond to CBT-I versus medication. Digital CBT-I apps like Sleepio are helping 60-65% of chronic pain users-but only if they finish the program.
The big shift? Pain clinics are now required to screen for sleep problems. In 2018, only 35% did. By 2023, it was 92%. That’s progress.
The market for integrated pain-sleep care is growing fast. Why? Because people are finally seeing the truth: you can’t manage pain without managing sleep. And you can’t sleep well without managing pain.
You’re not broken. You’re caught in a system that was never designed to treat both at once. But now we know how to fix it. And you don’t need to wait for a miracle drug to start healing.







okay but like... i tried CBT-I and it felt like my brain was being rewired with duct tape and hope. but after 6 weeks? i slept 7 hours straight for the first time in 3 years. no pills. no magic. just consistency.
so dopamine drops 20-30% after bad sleep? that explains why i cried over a spilled coffee yesterday.
the part about the blanket hurting? i thought i was broken. turns out my nerves are just screaming. thank you for naming it.
why do doctors still push melatonin like it’s a cure? i’ve taken it for 2 years. it just makes me dream about falling off cliffs.
you’re oversimplifying. CBT-I works for some, but if you have neuropathic pain from diabetes or MS, stimulus control won’t fix your nerve damage. also, not everyone can afford 10 weekly sessions. access is a huge barrier.
listen, i’ve been living with fibromyalgia for 14 years. i’ve tried everything: acupuncture, CBD, ketamine infusions, even that weird biofeedback headset from Amazon. nothing stuck until i started sleep restriction. i was only allowed 5 hours in bed. felt like torture. but after two weeks? my pain dropped from 8/10 to 4/10. not because i was relaxed. because my brain finally stopped thinking it was under attack. it’s not about willpower. it’s about reprogramming your nervous system. if you’re still stuck in the cycle, you’re not failing-you’re just waiting for the right tool. and CBT-I is that tool. stop looking for a pill. start building a rhythm.
So, let me get this straight: Pain → Sleep Loss → Inflammation → More Pain → Dopamine Crash → CBT-I? And you’re telling me this isn’t a metaphysical spiral? That this isn’t just the universe whispering, "You’re not ready to rest"? You’re reducing a cosmic feedback loop to a 10-session behavioral checklist? I’m not convinced. What about the soul? The spirit? The quiet, unspoken grief that lives in your bones at 3 a.m.?
the most beautiful thing about CBT-I is that it doesn’t ask you to be fixed-it asks you to be patient. you’re not broken, you’re just stuck in a loop your body learned out of survival. and the fact that you’re still here, reading this, still trying? that’s courage. not weakness. the bed isn’t your enemy. the fear is. and fear? it can be unlearned. one quiet night at a time.
so you wrote a 2000-word essay on why sleep matters... and the solution is "don’t use your bed for scrolling"? revolutionary. next you’ll tell me water is wet.
you cite NIH data, but ignore that 60% of CBT-I patients drop out before week 5. and the studies? mostly funded by sleep tech startups. also, your "pain diary" ignores emotional triggers. my pain spikes when I feel helpless. not when I’m on my phone. you’re treating symptoms like they’re the disease.
Thank you for this comprehensive, evidence-based breakdown. The integration of neurobiology with behavioral intervention is precisely what the field has needed for decades. I’ve trained clinicians in CBT-I for over a decade, and the most profound shifts occur not when pain disappears, but when patients reclaim agency over their nervous systems. The data is clear: sleep is not a luxury-it’s a biological imperative. To those still skeptical: this is not about discipline. It’s about neuroplasticity. And yes, it works-even when you’re exhausted. Start small. Track consistently. And remember: healing is not linear. But it is possible.