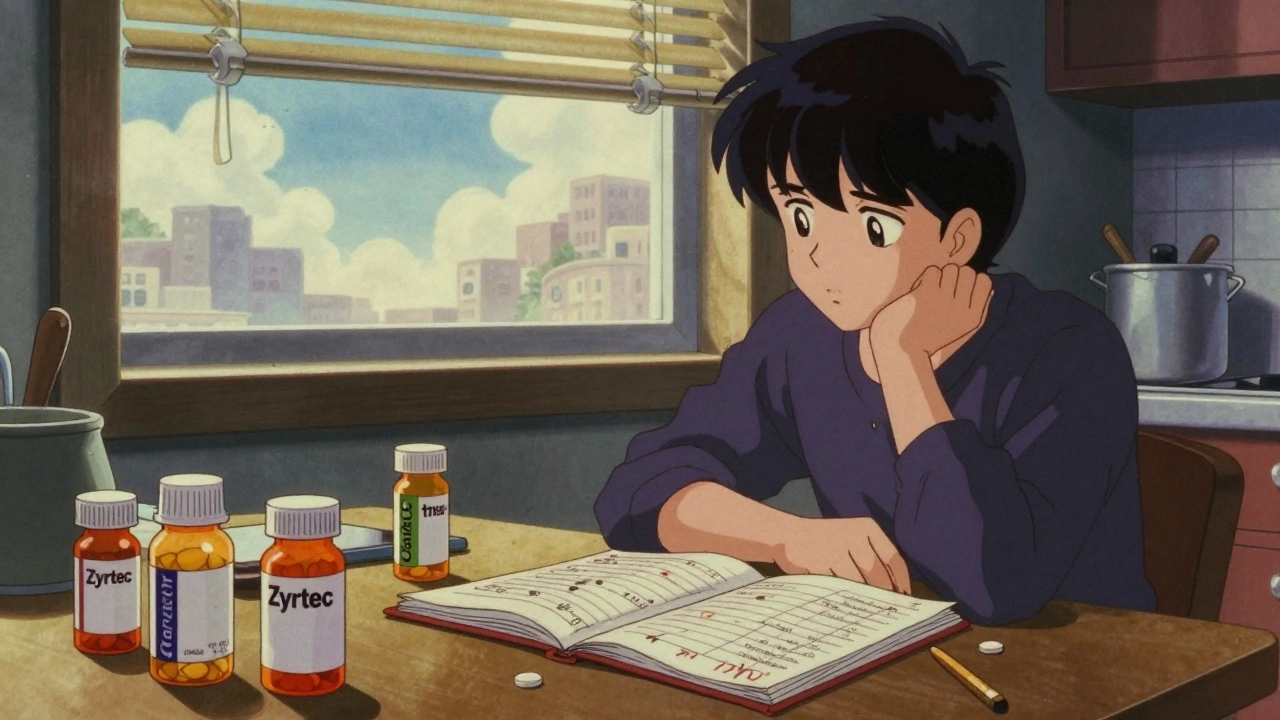
When your go-to antihistamine stops controlling your sneezes and itchy eyes, it’s not just in your head—it’s antihistamine tolerance, a reduced response to the drug after regular use, leading to diminished symptom relief. This isn’t addiction. It’s your body adapting. Over time, repeated exposure to antihistamines can lower receptor sensitivity, making the same dose less effective. It’s why someone who once took one pill for seasonal allergies now needs two—or finds nothing helps at all. Also known as drug tolerance, a physiological decrease in response to a medication after prolonged use, this happens with many long-term medications, but it’s especially common with antihistamines, drugs that block histamine, a chemical your body releases during allergic reactions.
Not all antihistamines cause tolerance the same way. First-gen ones like diphenhydramine (Benadryl) cross into the brain and cause drowsiness, which can lead to faster tolerance because they affect more systems. Second-gen ones like loratadine (Claritin) or cetirizine (Zyrtec) are designed to stay out of the brain, so tolerance develops slower—but it still happens. Studies show up to 40% of people using daily antihistamines for over a year report reduced effectiveness. And if you’re switching brands or generics thinking that’ll help, it won’t. Bioequivalent generics work the same way in your body. The issue isn’t the pill—it’s your body’s response to the active ingredient.
What can you do? First, don’t just crank up the dose. That’s risky and doesn’t fix the root problem. Try skipping doses for a few days to reset your receptors. Use antihistamines only when you need them, not every day. Consider switching to a different class—like nasal corticosteroids or leukotriene blockers—which work differently and don’t trigger the same tolerance. And if your allergies are year-round, it might be time to look at triggers: dust mites, pet dander, or mold. Medication isn’t always the answer. Environmental changes can cut your reliance on pills entirely.
You’ll find posts here that dig into how drug interactions, genetic differences, and even how you time your doses can change how antihistamines behave in your system. Some posts show why mixing antacids with certain meds can throw off absorption. Others explain how genetic testing can reveal why one person needs twice the dose of another. And there’s real talk on when to ask for a second opinion—if your allergy meds aren’t working, it might not be your fault. This isn’t about pushing more pills. It’s about understanding your body’s response and finding smarter, longer-lasting solutions.
Many people think antihistamines stop working over time, but true tolerance is rare. Learn why your allergy meds might seem less effective-and what actually helps when they don't.
