When you take antacids and antibiotics, a common combination used to treat stomach upset and infections. Also known as acid reducers and antibacterial drugs, it’s a pairing many people don’t realize can interfere with each other. Antacids work by neutralizing stomach acid to relieve heartburn or ulcers, but that same acid is often needed for your body to absorb antibiotics properly. If you take them together, the antibiotic might not reach the right level in your blood—making it less effective, or even useless.
This isn’t just theory. Studies show that drugs like doxycycline, a common antibiotic for acne, respiratory infections, and Lyme disease—and ciprofloxacin, used for urinary tract and sinus infections—bind to the minerals in antacids (like calcium, magnesium, or aluminum). That binding stops the antibiotic from being absorbed. The result? Your infection doesn’t clear up, and you might end up needing stronger meds—or worse, a hospital visit.
It’s not just about timing. Some people take antacids daily for acid reflux and pop an antibiotic when they get sick, thinking they’re doing the right thing. But if you’re on long-term acid-reducing meds, even proton pump inhibitors like omeprazole, your body’s ability to absorb certain antibiotics changes over time. That’s why your doctor needs to know everything you’re taking—not just prescriptions, but over-the-counter pills, supplements, and even herbal teas.
There are safe ways to use both. Wait at least two hours after taking an antacid before you take your antibiotic. Or take the antibiotic two hours before the antacid. Simple, but it makes a real difference. Some antibiotics, like amoxicillin, aren’t as affected by stomach acid, so your pharmacist can help you pick the right one if you’re already on an antacid. And if you’re on a long-term acid-reducing plan, ask if switching to a different class of meds might help your antibiotic work better.
It’s not just about avoiding bad interactions—it’s about making sure your treatment actually works. When antibiotics fail, it’s not always because the bug is resistant. Sometimes, it’s because the pill never got absorbed. That’s why the FDA and WHO both stress the importance of medication timing and patient awareness. You’re not just taking pills—you’re managing how your body uses them.
Below, you’ll find real-world guides on how to spot dangerous drug combos, when to ask for a second opinion about side effects, and how generic versions can behave differently than brand names. You’ll also see how mail-order pharmacies test for quality, how bioequivalence works, and what to do when your meds don’t seem to be working. These aren’t just articles—they’re tools to help you take control before things go wrong.
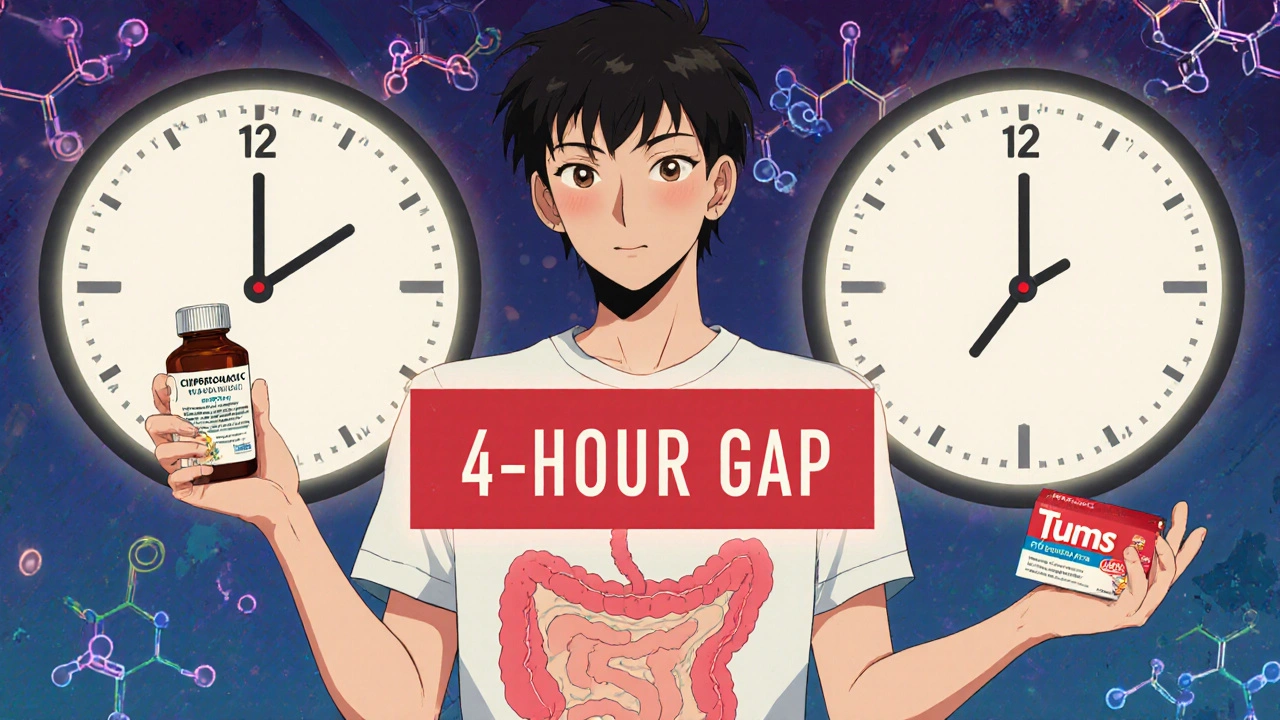
Learn how to time antacids and antibiotics correctly to avoid dangerous interactions that can reduce antibiotic effectiveness by up to 90%. Essential advice for anyone taking ciprofloxacin, doxycycline, or other common antibiotics.
