When a pharmacist hands you a new prescription, they’re not just giving you pills. They’re handing you a chance to take control of your health. But too often, that chance gets lost in the rush. The average counseling session in a community pharmacy lasts just over two minutes. That’s not enough time to explain why a medication matters, how to take it safely, or what to watch out for - unless the pharmacist has a clear, reliable script to follow.
Why Scripts Aren’t Just for Robots
Many people think counseling scripts sound robotic. Like a cashier reading a script to ask, "Would you like fries with that?" But that’s not how they work in pharmacy. A good script is a safety net, not a straightjacket. It ensures no critical piece of information slips through the cracks - especially when you’re juggling ten patients at once. The foundation for modern pharmacist counseling comes from the OBRA '90 the Omnibus Budget Reconciliation Act of 1990, which mandated that pharmacists offer counseling to Medicaid patients. Before this law, many patients left the pharmacy with no idea how to use their meds. Now, it’s not optional. In 18 states, pharmacists are legally required to actually counsel - not just offer to. In 32 others, they must at least offer it. And even if your state doesn’t require it, your pharmacy probably still uses scripts because they work.The Core Three: What Every Script Must Cover
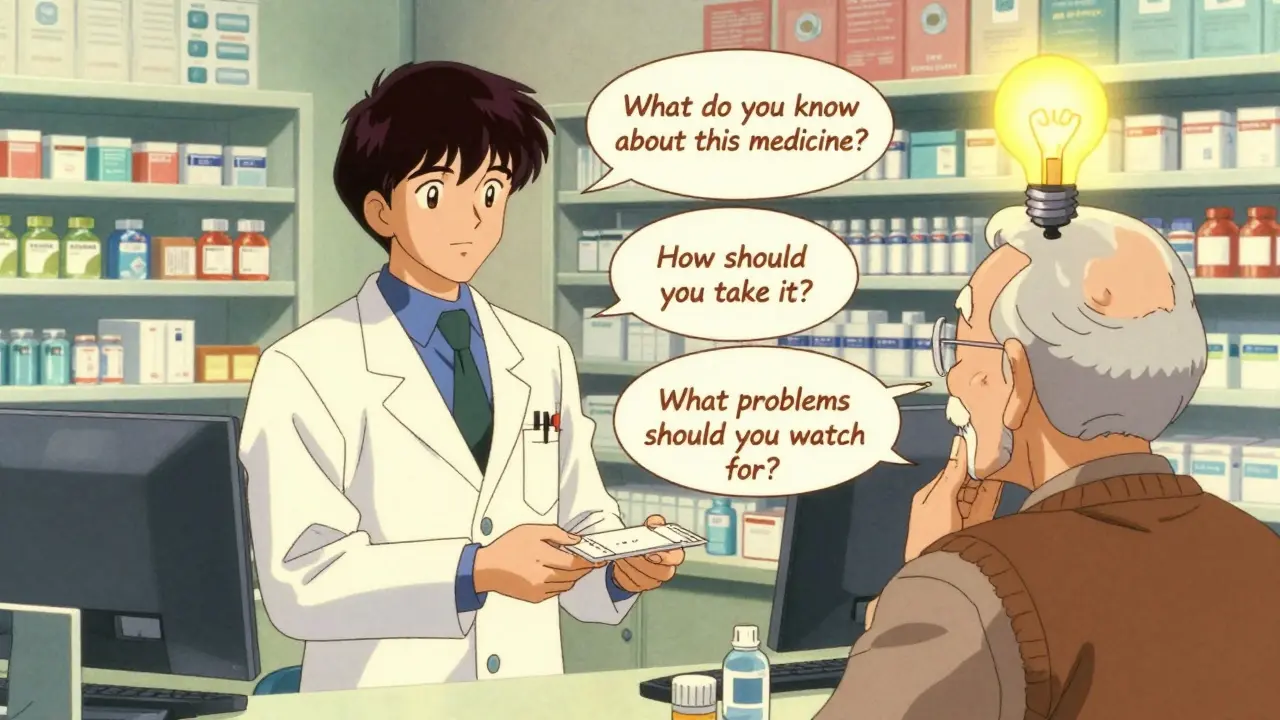
You don’t need a 20-page document to do effective counseling. The most proven framework comes from the Indian Health Service a U.S. federal agency whose simplified counseling model is widely adopted in training programs. It’s built on just three questions:- What do you know about this medicine? This isn’t a test. It’s a way to find out what the patient already understands - or misunderstands. Maybe they think the pill is for headaches, but it’s actually for high blood pressure. That’s a dangerous gap.
- How should you take it? This covers dose, timing, food interactions, and special instructions. "Take one by mouth twice daily" sounds simple - until you realize the patient has no idea what "by mouth" means, or they’re taking it with grapefruit juice because they’ve always done it that way.
- What problems should you watch for? Not every side effect. Just the serious ones. For antibiotics, it’s diarrhea that won’t stop. For blood thinners, it’s unusual bruising or bleeding. For opioids, it’s extreme drowsiness or trouble breathing.
How Scripts Evolve With Experience
New pharmacists often start by reading scripts word-for-word. It’s how they learn. But experienced pharmacists don’t memorize lines - they memorize the structure. They use the script as a checklist, then adapt based on the person in front of them. Dr. Daniel Holdford, a leading researcher in pharmacy education, put it simply: "Scripts help inexperienced students learn. As experience grows, they adapt the script to their own style." That’s the key. A script isn’t meant to be read. It’s meant to be remembered. Think of it like a recipe. You don’t read every word while cooking. You know the steps: chop, sauté, simmer. The script is the same. You know: assess, explain, verify.What Happens When Scripts Are Too Rigid?
Here’s where things go wrong. Some corporate pharmacies force pharmacists to follow scripts so tightly they become robotic. One pharmacist on Pharmacy Times described it as "talking to a vending machine." Patients tune out. They nod along, but they don’t absorb anything. The fix? Always use the teach-back method a proven technique where patients repeat instructions in their own words to confirm understanding. After explaining how to take the medicine, ask: "Can you tell me how you’ll take this at home?" If they say, "I’ll take it when I remember," you’ve got work to do. If they say, "I’ll take one pill at breakfast and one at dinner, even if I’m not hungry," you know they got it. This isn’t just good practice - it’s required by ASHP guidelines the American Society of Health-System Pharmacists’ standards for patient counseling, considered the gold standard in the U.S.. And it’s the single biggest predictor of whether someone will actually take their meds.
Special Cases Need Special Scripts
Not every prescription is the same. A diabetes medication needs different counseling than an antibiotic. And opioids? That’s a whole different ballgame. The RXCE 2023 training materials a widely used set of standardized counseling protocols for controlled substances in U.S. pharmacies require four extra points for opioid prescriptions:- How to store it safely (out of reach of kids and pets)
- How to dispose of unused pills (don’t flush them)
- Signs of overdose (slow breathing, unresponsiveness)
- Availability of naloxone (the overdose reversal drug)
Documentation: The Invisible Part of Counseling
Counseling isn’t complete until it’s recorded. CMS guidelines the Centers for Medicare & Medicaid Services’ official documentation standards for pharmacist counseling require two things:- That counseling was offered and accepted (or refused)
- That the pharmacist assessed the patient’s understanding
Time Constraints Are Real - But Not Impossible
The average counseling session is 2.1 minutes. That’s less time than it takes to brew a cup of coffee. So how do pharmacists cover everything? They use scripts. And they use them well. A 2023 study found that using the three-question framework from Indian Health Service cut average counseling time from 4.2 minutes to 2.9 minutes - without losing quality. That’s 30% faster. And in a busy pharmacy, that’s the difference between helping five patients or ten. The trick? Don’t try to explain everything. Focus on what matters most: safety, clarity, and confirmation.Language Barriers and How to Beat Them
If a patient doesn’t speak English, a script written in English won’t help. That’s why leading pharmacies now use pre-translated materials in over 150 languages. Services like the Language Access Network a national service providing translated patient education materials in multiple languages for healthcare providers provide printed handouts, QR codes linking to audio instructions, and even video explanations. Many pharmacies also use telephonic interpretation services. But even then, the script must be adapted. You can’t just translate words - you have to translate meaning. "Take on an empty stomach" means something different in cultures where meals are structured differently. A good script accounts for that.What’s Next? AI and Dynamic Scripts
The next big shift isn’t just better scripts - it’s smarter ones. Pilot programs at CVS and Walgreens are testing AI-assisted dynamic scripting a system that adapts counseling content in real-time based on patient responses during interactions. These tools listen to how a patient answers, then adjust the next question. If someone says, "I’m scared of side effects," the system prompts the pharmacist to focus on safety, not dosage. Early results show a 23% improvement in patient comprehension compared to static scripts. That’s not science fiction - it’s happening now.Why This Matters More Than Ever
Medication non-adherence costs the U.S. healthcare system $312 billion every year. That’s not just wasted pills. It’s hospital visits, emergency trips, and lives lost. Pharmacists are on the front line. And scripts? They’re the tool that turns good intentions into real results. It’s not about reading lines. It’s about making sure the person leaving the pharmacy knows exactly what to do - and why it matters.Getting Started: What You Need to Know
If you’re a new pharmacist or trainer, here’s your starting checklist:- Master the three core questions from Indian Health Service.
- Learn the OBRA '90 requirements for your state.
- Practice the teach-back method until it feels natural.
- Use the script as a guide, not a script.
- Document what matters: was it offered? Was it understood?
- For opioids, always include storage, disposal, and naloxone.
- Have translated materials ready for non-English speakers.



This is all just corporate propaganda wrapped in a white coat. You think these scripts are for patients? Nah. They're for liability. Pharmacies don't care if you understand your meds-they care that they can check the box and get reimbursed. I've seen it: pharmacists reading like robots while scrolling through TikTok on their phone. The 'teach-back method'? More like 'nod-back method.' Patients just say yes to get out of there. It's a scam dressed up as care.
Script = crutch. Real pharmacists dont need scripts. They know meds. They talk. They listen. This over-engineering? Pure bureaucracy. OBRA 90? More like OBRA 90-lose-your-soul.
Let’s be brutally honest: this whole system is performative. You can’t ‘counsel’ someone in 2.1 minutes. You can’t ‘assess understanding’ by clicking a checkbox. You can’t ‘save lives’ with a pre-written script that ignores cultural context, literacy levels, and mental health. This isn’t healthcare-it’s compliance theater. And anyone who defends it is either paid by the system or too afraid to admit it’s broken.
Scripts are for people who can’t think on their feet. If you need a script to explain how to take a pill, you shouldn’t be a pharmacist. Real professionals adapt. Real professionals talk like humans. This is why people hate pharmacies.
YES. YES. YES. This is exactly what we need more of! I’ve been training new pharmacists for 12 years, and the three-question framework? Game-changer. I’ve watched shy, nervous students turn into confident counselors just by learning to ASSESS, EXPLAIN, VERIFY. And the teach-back? That’s the magic. One patient told me, ‘I didn’t know my blood pressure med was also for my kidneys-I thought it was just for headaches.’ That’s why we do this. Not for the checkbox. For the moment they get it. And AI-assisted scripts? I’ve seen them in action-they’re not replacing us. They’re helping us be better. 🙌
Interesting read. I’ve worked in both rural and urban pharmacies. The script thing works better where there’s high turnover. Where I am, most pharmacists know their patients by name. They don’t need a script-they need time. But I get it. For the big chains, it’s the only way to keep consistency. Still, the real issue isn’t the script. It’s the 5-minute window we’re given to talk to someone who’s in pain, confused, and stressed. No script fixes that.
OMG I CRIED READING THIS. I had a pharmacist last week just hand me my antibiotics and say 'take 2 a day' and walk away. I didn't even know what it was for. I had to google it. My grandma died because no one explained her blood thinner. I'm so mad. This needs to change. I'm telling everyone. #PharmacistCounselingMatters
I think the tension here is between standardization and humanity. Scripts ensure no one falls through the cracks, especially in high-volume settings. But they’re not meant to replace connection. The best pharmacists I’ve known use the script as a backbone, then lean in and ask, 'How’s your week going?' That’s when real understanding happens. It’s not either/or-it’s both.
Love this! 🌍 I work with refugees and non-English speakers daily. The translated QR codes and audio scripts? Lifesavers. One woman from Syria didn’t know 'by mouth' meant 'swallow.' We showed her a video of someone taking a pill with water. She cried and hugged me. That’s not a script. That’s dignity. Keep pushing for multilingual tools. 🙏❤️
It’s infuriating how this entire system has been reduced to a compliance checklist. The ASHP guidelines? The CMS documentation? The OBRA mandates? All noble intentions-until they’re weaponized by corporate pharmacy chains to justify minimal interaction. And then they wonder why medication adherence is below 50%? Because patients don’t trust the process. They don’t trust the people. And why? Because they’ve been talked to like robots for years. This isn’t counseling. It’s coercion disguised as care.
While the three-question framework is efficient, it must be adapted with cultural sensitivity. In some Indian communities, patients defer to authority figures and rarely challenge medical advice-even if they do not understand. A script that assumes verbal confirmation equals comprehension may be dangerously inadequate. The teach-back method must be paired with observational cues and family involvement. A script without context is a hollow tool.